The Korean Society for Neuro-Oncology (KSNO) Guideline for Glioblastomas: Version 2018.01
- Affiliations
-
- 1Division of Neurooncology and Department of Neurosurgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 2Department of Neurosurgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 3Department of Neurosurgery, Bundang CHA Medical Center, CHA University, Seongnam, Korea.
- 4Department of Neurosurgery, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea.
- 5Department of Radiation Oncology, Ewha Women's University Mokdong Hospital, Ewha Women's University School of Medicine, Seoul, Korea.
- 6Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea.
- 7Department of Neurosurgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 8Department of Neurosurgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- 9Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 10Department of Radiation Oncology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 11Department of Neurosurgery, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea.
- 12Department of Pathology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 13Division of Medical Oncology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 14Department of Radiation Oncology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 15Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 16Department of Neurosurgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 17Clinic of Pediatric Oncology, National Cancer Center, Goyang, Korea.
- 18Department of Neurosurgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 19Department of Neurosurgery, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 20Department of Neurosurgery, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea. dschung@catholic.ac.kr
- 21Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea.
- 22Department of Neurology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 23Department of Radiation Oncology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 24Department of Pathology, Seoul St. Marry's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 25Department of Neurosurgery, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Gwangju, Korea.
- 26Department of Pediatrics, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 27Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 28Department of Pediatrics, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 29Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 30Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dh8lim@skku.edu
- KMID: 2444789
- DOI: http://doi.org/10.14791/btrt.2019.7.e25
Abstract
- BACKGROUND
There has been no practical guidelines for the management of patients with central nervous system (CNS) tumors in Korea for many years. Thus, the Korean Society for Neuro-Oncology (KSNO), a multidisciplinary academic society, started to prepare guidelines for CNS tumors from February 2018.
METHODS
The Working Group was composed of 35 multidisciplinary medical experts in Korea. References were identified through searches of PubMed, MEDLINE, EMBASE, and Cochrane CENTRAL using specific and sensitive keywords as well as combinations of keywords.
RESULTS
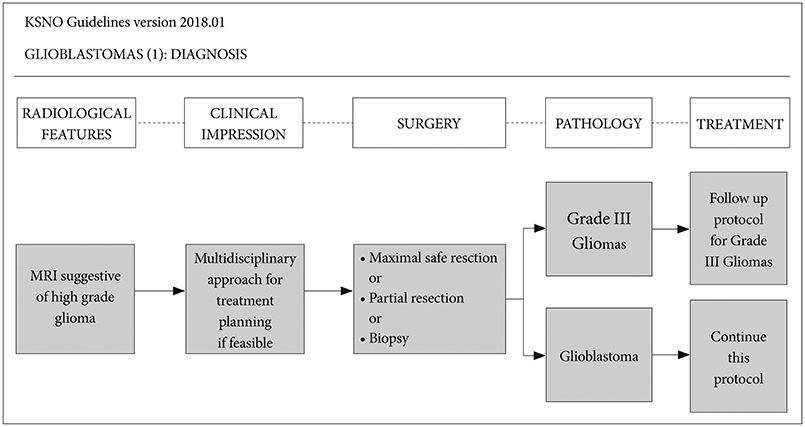
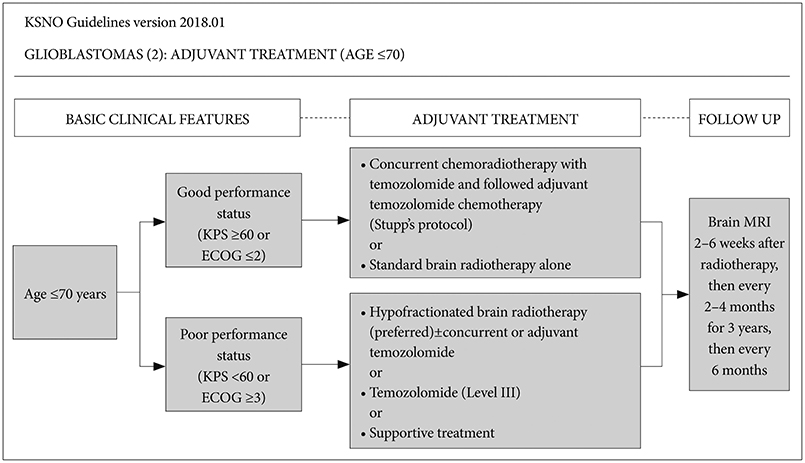
First, the maximal safe resection if feasible is recommended. After the diagnosis of a glioblastoma with neurosurgical intervention, patients aged ≤70 years with good performance should be treated by concurrent chemoradiotherapy with temozolomide followed by adjuvant temozolomide chemotherapy (Stupp's protocol) or standard brain radiotherapy alone. However, those with poor performance should be treated by hypofractionated brain radiotherapy (preferred)±concurrent or adjuvant temozolomide, temozolomide alone (Level III), or supportive treatment. Alternatively, patients aged >70 years with good performance should be treated by hypofractionated brain radiotherapy+concurrent and adjuvant temozolomide or Stupp's protocol or hypofractionated brain radiotherapy alone, while those with poor performance should be treated by hypofractionated brain radiotherapy alone or temozolomide chemotherapy if the patient has methylated MGMT gene promoter (Level III), or supportive treatment.
CONCLUSION
The KSNO's guideline recommends that glioblastomas should be treated by maximal safe resection, if feasible, followed by radiotherapy and/or chemotherapy according to the individual comprehensive condition of the patient.
MeSH Terms
Figure
Cited by 4 articles
-
The Korean Society for Neuro-Oncology (KSNO) Guideline for WHO Grade III Cerebral Gliomas in Adults: Version 2019.01
Young Zoon Kim, Chae-Yong Kim, Jaejoon Lim, Kyoung Su Sung, Jihae Lee, Hyuk-Jin Oh, Seok-Gu Kang, Shin-Hyuk Kang, Doo-Sik Kong, Sung Hwan Kim, Se-Hyuk Kim, Se Hoon Kim, Yu Jung Kim, Eui Hyun Kim, In Ah Kim, Ho Sung Kim, Tae Hoon Roh, Jae-Sung Park, Hyun Jin Park, Sang Woo Song, Seung Ho Yang, Wan-Soo Yoon, Hong In Yoon, Soon-Tae Lee, Sea-Won Lee, Youn Soo Lee, Chan Woo Wee, Jong Hee Chang, Tae-Young Jung, Hye Lim Jung, Jae Ho Cho, Seung Hong Choi, Hyoung Soo Choi, Je Beom Hong, Do Hoon Lim, Dong-Sup Chung,
Brain Tumor Res Treat. 2019;7(2):63-73. doi: 10.14791/btrt.2019.7.e42.The Korean Society for Neuro-Oncology (KSNO) Guideline for WHO Grade II Cerebral Gliomas in Adults: Version 2019.01
Young Zoon Kim, Chae-Yong Kim, Chan Woo Wee, Tae Hoon Roh, Je Beom Hong, Hyuk-Jin Oh, Seok-Gu Kang, Shin-Hyuk Kang, Doo-Sik Kong, Sung Hwan Kim, Se-Hyuk Kim, Se Hoon Kim, Yu Jung Kim, Eui Hyun Kim, In Ah Kim, Ho Sung Kim, Jae-Sung Park, Hyun Jin Park, Sang Woo Song, Kyoung Su Sung, Seung Ho Yang, Wan-Soo Yoon, Hong In Yoon, Jihae Lee, Soon-Tae Lee, Sea-Won Lee, Youn Soo Lee, Jaejoon Lim, Jong Hee Chang, Tae-Young Jung, Hye Lim Jung, Jae Ho Cho, Seung Hong Choi, Hyoung Soo Choi, Do Hoon Lim, Dong-Sup Chung,
Brain Tumor Res Treat. 2019;7(2):74-84. doi: 10.14791/btrt.2019.7.e43.Radiotherapy for Newly Diagnosed Glioblastoma in the Elderly: What Is the Standard?
Chan Woo Wee
Brain Tumor Res Treat. 2022;10(1):12-21. doi: 10.14791/btrt.2022.10.e34.Korean Brain Tumor Society Consensus Review for the Practical Recommendations on Glioma Management in Korea
Chul-Kee Park, Jong Hee Chang
J Korean Neurosurg Soc. 2023;66(3):308-315. doi: 10.3340/jkns.2023.0046.
Reference
-
1. Ostrom QT, Gittleman H, Truitt G, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2011-2015. Neuro Oncol. 2018; 20:Suppl 4. iv1–iv86.2. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Ellison DW, Figarella-Branger D. Glioblastoma, IDH-wild-types. In : Louise DN, Brate DJ, Ohgaki H, editors. WHO Classification of Tumours of the Central Nervous System. Rev 4th ed. Lyon: IARC Press;2016. p. 28–45.3. Dho YS, Jung KW, Ha J, et al. An updated nationwide epidemiology of primary brain tumors in Republic of Korea, 2013. Brain Tumor Res Treat. 2017; 5:16–23.
Article4. Hegi ME, Diserens AC, Gorlia T, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005; 352:997–1003.
Article5. Stupp R, Hegi ME, Mason WP, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009; 10:459–466.6. Stupp R, Wong ET, Kanner AA, et al. NovoTTF-100A versus physician's choice chemotherapy in recurrent glioblastoma: a randomised phase III trial of a novel treatment modality. Eur J Cancer. 2012; 48:2192–2202.
Article7. Maxwell R, Jackson CM, Lim M. Clinical trials investigating immune checkpoint blockade in glioblastoma. Curr Treat Options Oncol. 2017; 18:51.
Article8. Nabors LB, Portnow J, Ammirati M, et al. Central nervous system cancers, version 1.2015. J Natl Compr Canc Netw. 2015; 13:1191–1202.
Article9. Nabors LB, Portnow J, Ammirati M, et al. NCCN guidelines insights: central nervous system cancers, version 1.2017. J Natl Compr Canc Netw. 2017; 15:1331–1345.
Article10. Weller M, van den Bent M, Hopkins K, et al. EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol. 2014; 15:e395–e403.
Article11. Roh TH, Park HH, Kang SG, et al. Long-term outcomes of concomitant chemoradiotherapy with temozolomide for newly diagnosed glioblastoma patients: a single-center analysis. Medicine (Baltimore). 2017; 96:e7422.12. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–820.
Article13. Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005; 352:987–996.
Article14. Reuss DE, Sahm F, Schrimpf D, et al. ATRX and IDH1-R132H immunohistochemistry with subsequent copy number analysis and IDH sequencing as a basis for an “integrated” diagnostic approach for adult astrocytoma, oligodendroglioma and glioblastoma. Acta Neuropathol. 2015; 129:133–146.
Article15. Killela PJ, Reitman ZJ, Jiao Y, et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc Natl Acad Sci U S A. 2013; 110:6021–6026.
Article16. Arita H, Yamasaki K, Matsushita Y, et al. A combination of TERT promoter mutation and MGMT methylation status predicts clinically relevant subgroups of newly diagnosed glioblastomas. Acta Neuropathol Commun. 2016; 4:79.
Article17. Meyronet D, Esteban-Mader M, Bonnet C, et al. Characteristics of H3 K27M-mutant gliomas in adults. Neuro Oncol. 2017; 19:1127–1134.
Article18. Louis DN, Aldape K, Brat DJ, et al. Announcing cIMPACT-NOW: the consortium to inform molecular and practical approaches to CNS tumor taxonomy. Acta Neuropathol. 2017; 133:1–3.
Article19. Brat DJ, Aldape K, Colman H, et al. cIMPACT-NOW update 3: recommended diagnostic criteria for “Diffuse astrocytic glioma, IDH-wildtype, with molecular features of glioblastoma, WHO grade IV”. Acta Neuropathol. 2018; 136:805–810.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Overview of Practical Guidelines for Gliomas by KSNO, NCCN, and EANO
- Yesterdays, Todays, and Tomorrows—Korean Society for Pediatric Neuro-Oncology*
- The Korean Society for Neuro-Oncology (KSNO) Guideline for the Management of Brain Tumor Patients During the Crisis Period: A Consensus Recommendation Using the Delphi Method (Version 2023.1)
- The Korean Society for Neuro-Oncology (KSNO) Guideline for WHO Grade III Cerebral Gliomas in Adults: Version 2019.01
- The Korean Society for Neuro-Oncology (KSNO) Guideline for WHO Grade II Cerebral Gliomas in Adults: Version 2019.01