J Korean Orthop Assoc.
2019 Apr;54(2):110-119. 10.4055/jkoa.2019.54.2.110.
Shoulder Replacement Arthroplasty after Failed Proximal Humerus Fracture
- Affiliations
-
- 1Center for Shoulder, Elbow and Sports Medicine, Neon Orthopaedic Clinic, Seoul, Korea. ez2chanz@naver.com
- 2Department of Orthopedic Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2444775
- DOI: http://doi.org/10.4055/jkoa.2019.54.2.110
Abstract
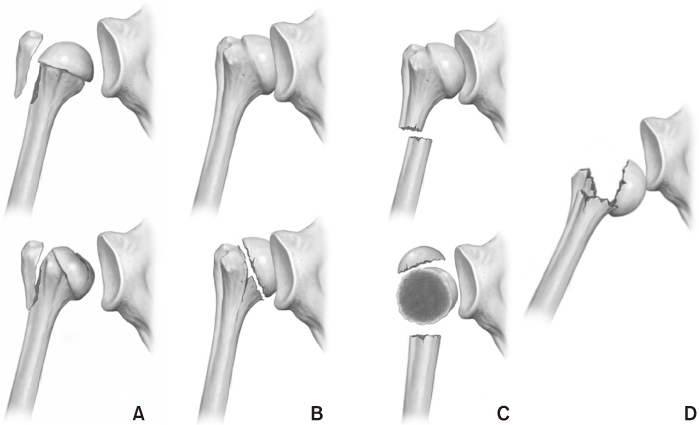
- Proximal humerus fracture can be defined as a fracture that occurs in the surgical neck or proximal part of the humerus. Despite the appropriate treatment, however, various complications and sequelae can occur, and the treatment is quite difficult often requiring surgical treatment, such as a shoulder replacement. The classification of sequelae after a proximal humerus fracture is most commonly used by Boileau and can be divided into two categories and four types. Category I is an intracapsular impacted fracture that is not accompanied by important distortions between the tuberosities and humeral head. An anatomic prosthesis can be used without greater tuberosity osteotomy. In category I, there are type 1 with cephalic collapse or necrosis with minimal tuberosity malunion and type 2 related to locked dislocation or fracture-dislocation. Category II is an extracapsular dis-impacted fracture with gross distortion between the tuberosities and the humeral head. To perform an anatomic prosthesis, a tuberosity osteotomy should be performed. In category II, there are type 3 with nonunion of the surgical neck and type 4 with severe tuberosity malunion. In type 1, non-constrained arthroplasty (NCA) without a tuberosity osteotomy should be considered as a treatment. On the other hand, reverse shoulder arthroplasty (RSA) should be considered if types 1C or 1D accompanied by valgus or varus deformity or severe fatty degeneration of the rotator cuff. In general, the results are satisfactory when NCA is performed in type 2 sequelae. On the other hand, RSA can be considered as an option when there is no bony defect of the glenoid and a defect of the rotator cuff is accompanied. In type 3, it would be effective to perform internal fixation with a bone wedge graft rather than shoulder replacement arthroplasty. Recent reports on the results of RSA are also increasing. On the other hand, recent reports suggest that good results are obtained with RSA in type 3. In type 4, RSA should be considered as a first option.
MeSH Terms
Figure
Reference
-
1. Rose SH, Melton LJ 3rd, Morrey BF, Ilstrup DM, Riggs BL. Epidemiologic features of humeral fractures. Clin Orthop Relat Res. 1982; (168):24–30.
Article2. Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001; 72:365–371.
Article3. Gaebler C, McQueen MM, Court-Brown CM. Minimally displaced proximal humeral fractures: epidemiology and outcome in 507 cases. Acta Orthop Scand. 2003; 74:580–585.4. Neer CS 2nd. Displaced proximal humeral fractures. Part I. Classification and evaluation. By Charles S. Neer, I, 1970. Clin Orthop Relat Res. 1987; (223):3–10.5. Young TB, Wallace WA. Conservative treatment of fractures and fracture-dislocations of the upper end of the humerus. J Bone Joint Surg Br. 1985; 67:373–377.
Article6. Cofield RH. Comminuted fractures of the proximal humerus. Clin Orthop Relat Res. 1988; 230:49–57.
Article7. Hawkins RJ, Angelo RL. Displaced proximal humeral fractures. Selecting treatment, avoiding pitfalls. Orthop Clin North Am. 1987; 18:421–431.
Article8. Kristiansen B, Christensen SW. Proximal humeral fractures. Late results in relation to classification and treatment. Acta Orthop Scand. 1987; 58:124–127.
Article9. Court-Brown CM, Cattermole H, McQueen MM. Impacted valgus fractures (B1.1) of the proximal humerus. The results of non-operative treatment. J Bone Joint Surg Br. 2002; 84:504–508.10. Murray IR, Amin AK, White TO, Robinson CM. Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Joint Surg Br. 2011; 93:1–11.11. Yin B, Moen TC, Thompson SA, Bigliani LU, Ahmad CS, Levine WN. Operative treatment of isolated greater tuberosity fractures: retrospective review of clinical and functional outcomes. Orthopedics. 2012; 35:e807–e814.
Article12. Gardner MJ, Boraiah S, Helfet DL, Lorich DG. The anterolateral acromial approach for fractures of the proximal humerus. J Orthop Trauma. 2008; 22:132–137.
Article13. Green DP, Rockwood CA Jr, Bucholz RW. Rockwood and Green's fractures in adults. Philadelphia: Lippincott Williams & Wilkins;2010.14. Fjalestad T, Hole MØ, Hovden IA, Blücher J, Strømsøe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma. 2012; 26:98–106.
Article15. Hodgson SA, Mawson SJ, Stanley D. Rehabilitation after twopart fractures of the neck of the humerus. J Bone Joint Surg Br. 2003; 85:419–422.
Article16. Koval KJ, Gallagher MA, Marsicano JG, Cuomo F, McShinawy A, Zuckerman JD. Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am. 1997; 79:203–207.
Article17. Agudelo J, Schürmann M, Stahel P, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007; 21:676–681.
Article18. Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF. Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg. 2010; 19:489–494.
Article19. Hussey MM, Hussey SE, Mighell MA. Reverse shoulder arthroplasty as a salvage procedure after failed internal fixation of fractures of the proximal humerus: outcomes and complications. Bone Joint J. 2015; 97:967–972.20. Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013; 22:542–549.
Article21. Moineau G, McClelland WB Jr, Trojani C, Rumian A, Walch G, Boileau P. Prognostic factors and limitations of anatomic shoulder arthroplasty for the treatment of posttraumatic cephalic collapse or necrosis (type-1 proximal humeral fracture sequelae). J Bone Joint Surg Am. 2012; 94:2186–2194.
Article22. Mansat P, Bonnevialle N. Treatment of fracture sequelae of the proximal humerus: anatomical vs reverse shoulder prosthesis. Int Orthop. 2015; 39:349–354.
Article23. Neer CS 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982; 64:319–337.
Article24. Neer CS. Shoulder reconstruction. Philadelphia: Saunders;1990. p. 273–362.25. Neer CI. Nonunion of the surgical neck of the humerus. Orthop Trans. 1983; 7:389.26. Boileau P, Trojani C, Walch G, Krishnan SG, Romeo A, Sinnerton R. Shoulder arthroplasty for the treatment of the sequelae of fractures of the proximal humerus. J Shoulder Elbow Surg. 2001; 10:299–308.
Article27. Boileau P, Chuinard C, Le Huec JC, Walch G, Trojani C. Proximal humerus fracture sequelae: impact of a new radiographic classification on arthroplasty. Clin Orthop Relat Res. 2006; 442:121–130.28. Boileau P, Walch G, Trojani C, Sinnerton R, Romeo AA, Veneau B. Sequelae of fractures of the proximal humerus: surgical classification and limits of shoulder arthroplasty. Berlin: Springer;1999. p. 349–358.29. Raiss P, Edwards TB, Collin P, et al. Reverse shoulder arthroplasty for malunions of the proximal part of the humerus (type-4 fracture sequelae). J Bone Joint Surg Am. 2016; 98:893–899.
Article30. Raiss P, Edwards TB, da Silva MR, Bruckner T, Loew M, Walch G. Reverse shoulder arthroplasty for the treatment of nonunions of the surgical neck of the proximal part of the humerus (type-3 fracture sequelae). J Bone Joint Surg Am. 2014; 96:2070–2076.
Article31. Boileau P, Neyton L. Reverse shoulder arthroplasty in proximal humerus fracture sequelae: constrained or nonconstrained prosthesis. In : Boileau P, editor. Shoulder concepts. Montpellier: Sauramps medical;2008. p. 265–269.32. Hattrup SJ, Waldrop R, Sanchez-Sotelo J. Reverse total shoulder arthroplasty for posttraumatic sequelae. J Orthop Trauma. 2016; 30:e41–e47.
Article33. Grubhofer F, Wieser K, Meyer DC, Catanzaro S, Schürholz K, Gerber C. Reverse total shoulder arthroplasty for failed open reduction and internal fixation of fractures of the proximal humerus. J Shoulder Elbow Surg. 2017; 26:92–100.
Article34. Schliemann B, Theisen C, Kösters C, Raschke MJ, Weimann A. Reverse total shoulder arthroplasty for type I fracture sequelae after internal fixation of proximal humerus fractures. Arch Orthop Trauma Surg. 2017; 137:1677–1683.
Article35. Matsoukis J, Tabib W, Guiffault P, et al. Primary unconstrained shoulder arthroplasty in patients with a fixed anterior glenohumeral dislocation. J Bone Joint Surg Am. 2006; 88:547–552.
Article36. Sperling JW, Pring M, Antuna SA, Cofield RH. Shoulder arthroplasty for locked posterior dislocation of the shoulder. J Shoulder Elbow Surg. 2004; 13:522–527.
Article37. Wall B, Nové-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007; 89:1476–1485.38. Nolan BM, Ankerson E, Wiater JM. Reverse total shoulder arthroplasty improves function in cuff tear arthropathy. Clin Orthop Relat Res. 2011; 469:2476–2482.
Article39. Werner BS, Böhm D, Abdelkawi A, Gohlke F. Glenoid bone grafting in reverse shoulder arthroplasty for long-standing anterior shoulder dislocation. J Shoulder Elbow Surg. 2014; 23:1655–1661.
Article40. Raiss P, Edwards TB, Bruckner T, Loew M, Zeifang F, Walch G. Reverse arthroplasty for patients with chronic locked dislocation of the shoulder (type 2 fracture sequela). J Shoulder Elbow Surg. 2017; 26:279–287.
Article41. Duquin TR, Jacobson JA, Sanchez-Sotelo J, Sperling JW, Cofield RH. Unconstrained shoulder arthroplasty for treatment of proximal humeral nonunions. J Bone Joint Surg Am. 2012; 94:1610–1617.
Article42. Boyle MJ, Youn SM, Frampton CM, Ball CM. Functional outcomes of reverse shoulder arthroplasty compared with hemiarthroplasty for acute proximal humeral fractures. J Shoulder Elbow Surg. 2013; 22:32–37.
Article43. Garrigues GE, Johnston PS, Pepe MD, Tucker BS, Ramsey ML, Austin LS. Hemiarthroplasty versus reverse total shoulder arthroplasty for acute proximal humerus fractures in elderly patients. Orthopedics. 2012; 35:e703–e708.
Article44. Martinez AA, Bejarano C, Carbonel I, Iglesias D, Gil-Albarova J, Herrera A. The treatment of proximal humerus nonunions in older patients with reverse shoulder arthroplasty. Injury. 2012; 43:Suppl 2. S3–S6.
Article45. Jacobson JA, Duquin TR, Sanchez-Sotelo J, Schleck CD, Sperling JW, Cofield RH. Anatomic shoulder arthroplasty for treatment of proximal humerus malunions. J Shoulder Elbow Surg. 2014; 23:1232–1239.
Article46. Gwinner C, Greiner S, Gerhardt C, Scheibel M. Reverse shoulder arthroplasty for fracture sequelae. Orthopade. 2013; 42:531–541.47. Kılıç M, Berth A, Blatter G, et al. Anatomic and reverse shoulder prostheses in fracture sequelae of the humeral head. Acta Orthop Traumatol Turc. 2010; 44:417–425.
Article48. Willis M, Min W, Brooks JP, et al. Proximal humeral malunion treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2012; 21:507–513.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arthroplasty for Fractures of the Proximal Part of the Humerus
- Reverse Shoulder Arthroplasty for Humeral Head Fracture with Massive Rotator Cuff Tear in Elderly Patient
- Current concept of shoulder replacement arthroplasty
- Recurrent Shoulder Dislocation and Proximal Humerus Fracture in Neurofibromatosis Type I: A Case Report
- A Operative treatment of the three-part, four-part Fracture and Fracture dislocation in proximal humerus