Ann Surg Treat Res.
2019 May;96(5):237-249. 10.4174/astr.2019.96.5.237.
Long-term clinical outcomes after endovascular management of ruptured pseudoaneurysm in patients undergoing pancreaticoduodenectomy
- Affiliations
-
- 1Department of Surgery, Konkuk University Chungju Hospital, Konkuk University School of Medicine, Chungju, Korea.
- 2Department of Surgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea. sh3468.choi@gmail.com
- 3Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Surgery, Chungnam National University Hospital, Daejeon, Korea.
- 5Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Department of Surgery, Chuncheon Sacred Heart Hospital, Chuncheon, Korea.
- KMID: 2443587
- DOI: http://doi.org/10.4174/astr.2019.96.5.237
Abstract
- PURPOSE
Recent studies have analyzed the short-term clinical outcomes of ndovascular management. However, the long-term outcomes are unknown. This study aimed to investigate clinical outcomes after endovascular management for ruptured pseudoaneurysm in patients after pancreaticoduodenectomy (PD).
METHODS
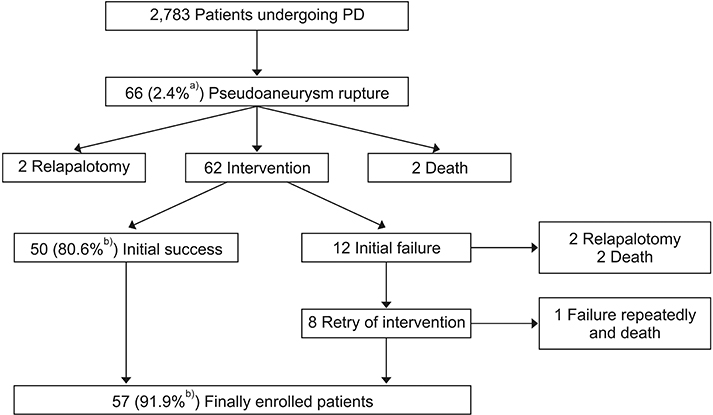
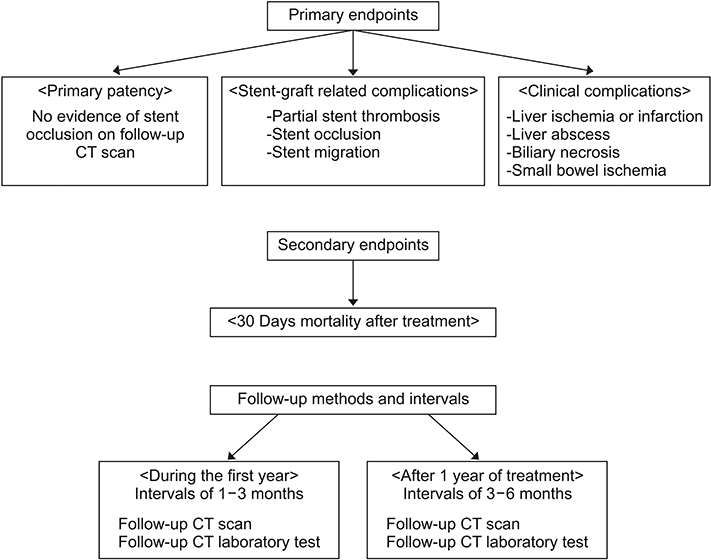
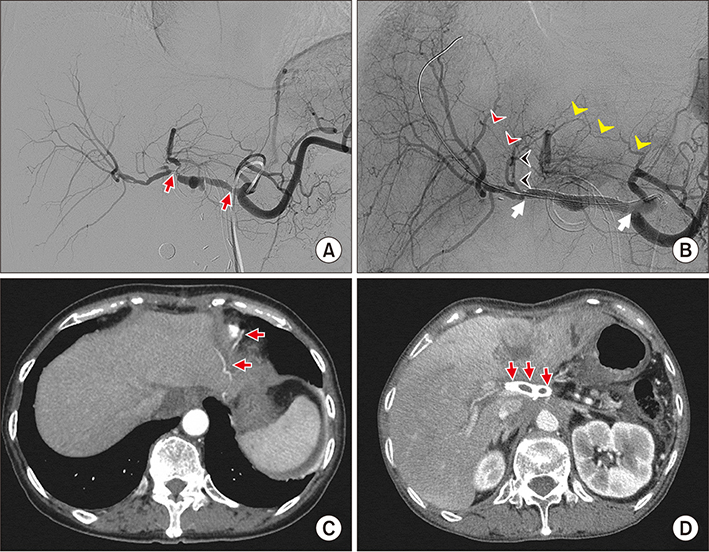
The medical records of 2,783 patients who underwent PD were retrospectively reviewed at a single center. Of 62 patients who received intervention after pseudonaeurysm rupture, 57 patients (91.9%) experienced eventual success of hemostasis. The patients were composed as follows: (embolization only [EMB], n = 30), (stent-graft placement only [STENT], n = 19) and (both embolization and stent-graft placement simultaneously or different times [EMB + STENT], n = 8). Long-term complications were defined as events that occur more than 30 days after the last successful endovascular treatment.
RESULTS
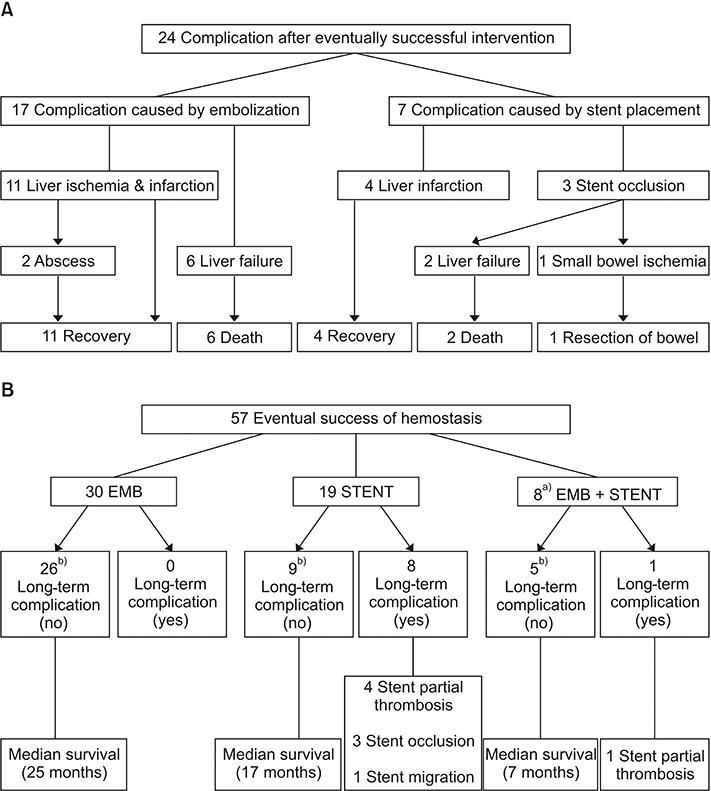
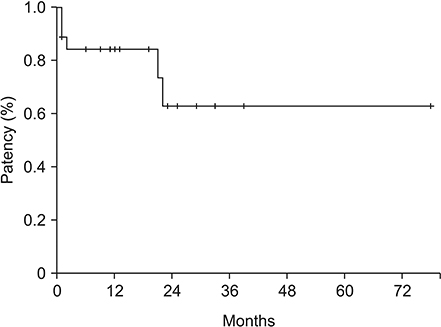
Among 57 patients, short-term stent-graft related complications developed in 3 patients (5.3%) and clinical complication developed in 18 patients (31.5%). Nine (15.8%) had long-term stent-graft related complications, which involved partial thrombosis in 5 cases, occlusion in 3 cases and migration in 1 case. Except for 1 death, the remaining 8 cases did not experience clinical complications. The stent graft primary patency rate was 88.9% after 1 month, 84.2% after 1 year, and 63.2% after 2 years. Of 57 patients, 30 days mortality occurred in 8 patients (14.0%).
CONCLUSION
After recovery from initial complication, most of patients did not experience fatal clinical complication during long-term follow-up. Endovascular management is an effective and safe management of pseudoaneurysm rupture after PD in terms of long-term safety.
MeSH Terms
Figure
Reference
-
1. Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de Wit LT, Busch OR, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 2000; 232:786–795.
Article2. Choi SH, Moon HJ, Heo JS, Joh JW, Kim YI. Delayed hemorrhage after pancreaticoduodenectomy. J Am Coll Surg. 2004; 199:186–191.3. de Castro SM, Kuhlmann KF, Busch OR, van Delden OM, Lameris JS, van Gulik TM, et al. Delayed massive hemorrhage after pancreatic and biliary surgery: embolization or surgery? Ann Surg. 2005; 241:85–91.
Article4. Lee HG, Heo JS, Choi SH, Choi DW. Management of bleeding from pseudoaneurysms following pancreaticoduodenectomy. World J Gastroenterol. 2010; 16:1239–1244.
Article5. Tien YW, Lee PH, Yang CY, Ho MC, Chiu YF. Risk factors of massive bleeding related to pancreatic leak after pancreaticoduodenectomy. J Am Coll Surg. 2005; 201:554–559.
Article6. Ding X, Zhu J, Zhu M, Li C, Jian W, Jiang J, et al. Therapeutic management of hemorrhage from visceral artery pseudoaneurysms after pancreatic surgery. J Gastrointest Surg. 2011; 15:1417–1425.
Article7. Puppala S, Patel J, McPherson S, Nicholson A, Kessel D. Hemorrhagic complications after Whipple surgery: imaging and radiologic intervention. AJR Am J Roentgenol. 2011; 196:192–197.
Article8. Roulin D, Cerantola Y, Demartines N, Schafer M. Systematic review of delayed postoperative hemorrhage after pancreatic resection. J Gastrointest Surg. 2011; 15:1055–1062.
Article9. Ellison EC. Evidence-based management of hemorrhage after pancreaticoduodenectomy. Am J Surg. 2007; 194:10–12.
Article10. Asai K, Watanabe M, Kusachi S, Matsukiyo H, Saito T, Kodama H, et al. Successful treatment of a common hepatic artery pseudoaneurysm using a coronary covered stent following pancreatoduodenectomy: report of a case. Surg Today. 2014; 44:160–165.
Article11. Fujioka S, Suzuki F, Funamizu N, Okamoto T, Munakata K, Ashida H, et al. Stent graft placement and balloon dilation for pseudoaneurysm complicated by distal arterial stenosis of the hepatic artery after pancreaticoduodenectomy. Surg Case Rep. 2015; 1:60.
Article12. Gaudon C, Soussan J, Louis G, Moutardier V, Gregoire E, Vidal V. Late postpancreatectomy hemorrhage: Predictive factors of morbidity and mortality after percutaneous endovascular treatment. Diagn Interv Imaging. 2016; 97:1071–1077.
Article13. Gwon DI, Ko GY, Sung KB, Shin JH, Kim JH, Yoon HK. Endovascular management of extrahepatic artery hemorrhage after pancreatobiliary surgery: clinical features and outcomes of transcatheter arterial embolization and stent-graft placement. AJR Am J Roentgenol. 2011; 196:W627–W634.
Article14. Hur S, Yoon CJ, Kang SG, Dixon R, Han HS, Yoon YS, et al. Transcatheter arterial embolization of gastroduodenal artery stump pseudoaneurysms after pancreaticoduodenectomy: safety and efficacy of two embolization techniques. J Vasc Interv Radiol. 2011; 22:294–301.
Article15. Miura F, Asano T, Amano H, Yoshida M, Toyota N, Wada K, et al. Management of postoperative arterial hemorrhage after pancreato-biliary surgery according to the site of bleeding: re-laparotomy or interventional radiology. J Hepatobiliary Pancreat Surg. 2009; 16:56–63.
Article16. Okuno A, Miyazaki M, Ito H, Ambiru S, Yoshidome H, Shimizu H, et al. Nonsurgical management of ruptured pseudoaneurysm in patients with hepatobiliary pancreatic diseases. Am J Gastroenterol. 2001; 96:1067–1071.
Article17. Pedersoli F, Isfort P, Keil S, Goerg F, Zimmermann M, Liebl M, et al. Stentgraft implantation for the treatment of postoperative hepatic artery pseudoaneurysm. Cardiovasc Intervent Radiol. 2016; 39:575–581.
Article18. Wang MQ, Liu FY, Duan F, Wang ZJ, Song P, Fan QS. Stent-grafts placement for treatment of massive hemorrhage from ruptured hepatic artery after pancreaticoduodenectomy. World J Gastroenterol. 2010; 16:3716–3722.
Article19. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13.
Article20. Beyer L, Bonmardion R, Marciano S, Hartung O, Ramis O, Chabert L, et al. Results of non-operative therapy for delayed hemorrhage after pancreaticoduodenectomy. J Gastrointest Surg. 2009; 13:922–928.
Article21. Lim SJ, Park KB, Hyun DH, Do YS, Park HS, Shin SW, et al. Stent graft placement for postsurgical hemorrhage from the hepatic artery: clinical outcome and CT findings. J Vasc Interv Radiol. 2014; 25:1539–1548.
Article22. Mansueto G, D'Onofrio M, Iacono C, Rozzanigo U, Serio G, Procacci C. Gastroduodenal artery stump haemorrhage following pylorus-sparing Whipple procedure: treatment with covered stents. Dig Surg. 2002; 19:237–240.
Article23. Sasaki K, Ueda K, Nishiyama A, Yoshida K, Sako A, Sato M, et al. Successful utilization of coronary covered stents to treat a common hepatic artery pseudoaneurysm secondary to pancreatic fistula after Whipple’s procedure: report of a case. Surg Today. 2009; 39:68–71.
Article24. Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2016; 68:1082–1115.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Miscellaneous Endovascular Treatment of Ruptured Hepatic Artery Pseudoaneurysms after Pylorus Preserving Pancreaticoduodenectomy
- Rupture of a Gastroduodenal Artery Pseudoaneurysm Revealed by Non-traumatic Hemoperitoneum: Report on a Case
- A Pseudoaneurysm Associated with a Ruptured Cerebral Aneurysm: Hypothesis on the Formation of the PA and Feasibility of Endovascular Treatment
- Jejunal Migration of the Stent-Graft Used for Common Hepatic Artery Pseudoaneurysm
- Conjoined Stent Technique for Radiation Induced Long Segment Carotid Stenosis and Pseudoaneurysm