J Korean Ophthalmol Soc.
2019 Apr;60(4):340-347. 10.3341/jkos.2019.60.4.340.
Long-term Clinical Outcome of Vitrectomy for the Treatment of Optic Disc Pit Maculopathy
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University Yangsan Hospital, Yangsan, Korea. isbyon@pusan.ac.kr
- 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 3Department of Ophthalmology, Pusan National University Hospital, Busan, Korea.
- 4Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- 5Department of Ophthalmology, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2443150
- DOI: http://doi.org/10.3341/jkos.2019.60.4.340
Abstract
- PURPOSE
To evaluate the long-term outcomes of optic disc pit maculopathy after vitrectomy.
METHODS
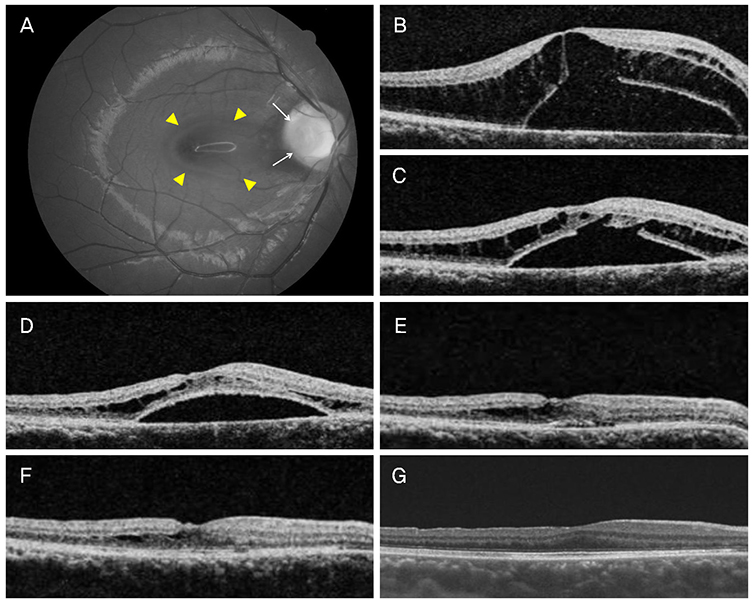
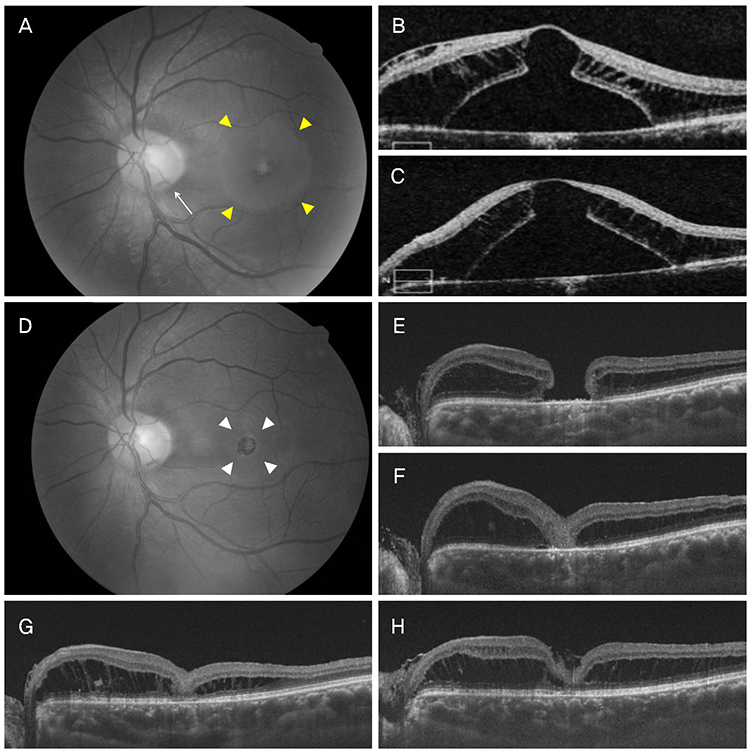
We evaluated retrospectively the medical records of eight patients with macular retinal detachment or retinoschisis who underwent vitrectomy due to optic disc pit maculopathy. The best-corrected visual acuity and optical coherence tomography findings were analyzed after surgery.
RESULTS
Eight eyes of eight patients (two male and six female) were enrolled. The mean best-corrected visual acuity was 0.76 log MAR, the mean age was 42.8, and the mean follow-up period was 56 months (range: 8-120 months). At baseline, retinoschisis was observed in all eight eyes. Six eyes had serous retinal detachment of the macula. Vitrectomy for a complete posterior vitreous detachment was performed. Additional internal limiting membrane peeling and tamponade were performed in six and four eyes, respectively. After surgery, serous retinal detachment was gone in all eyes (100%) at a mean of 22.8 months (range: 18 days-60 months). Three of eight eyes (37.5%) showed the disappearance of retinoschisis at a mean of 6.8 months (range: 1.7-21 months), but the remaining patients still had retinoschisis at the final visit. Ocular complications were full-thickness macular hole and iatrogenic retinal detachment in each case. The final corrected visual acuity improved to 0.29 logMAR.
CONCLUSIONS
Vitrectomy is an effective treatment for patients with optic disc pit maculopathy. It achieved anatomical and visual improvements over a long period of time. However, retinoschisis due to inner retinal fluid remained in many patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Halbertsma KT. Crater-like hole and coloboma of the disc associated with changes at the macula. Br J Ophthalmol. 1927; 11:11–17.
Article2. Brown GC, Shields JA, Goldberg RE. Congenital pits of the optic nerve head. II. Clinical studies in humans. Ophthalmology. 1980; 87:51–65.3. Johnson TM, Johnson MW. Pathogenic implications of subretinal gas migration through pits and atypical colobomas of the optic nerve. Arch Ophthalmol. 2004; 122:1793–1800.4. Jain N, Johnson MW. Pathogenesis and treatment of maculopathy associated with cavitary optic disc anomalies. Am J Ophthalmol. 2014; 158:423–435.
Article5. Hirakata A, Okada AA, Hida T. Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology. 2005; 112:1430–1435.
Article6. Theodossiadis PG, Grigoropoulos VG, Emfietzoglou J, Theodossiadis GP. Vitreous findings in optic disc pit maculopathy based on optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2007; 245:1311–1318.
Article7. Hirakata A, Inoue M, Hiraoka T, McCuen BW 2nd. Vitrectomy without laser treatment or gas tamponade for macular detachment associated with an optic disc pit. Ophthalmology. 2012; 119:810–818.
Article8. Shukla D, Kalliath J, Tandon M, Vijayakumar B. Vitrectomy for optic disk pit with macular schisis and outer retinal dehiscence. Retina. 2012; 32:1337–1342.
Article9. Bottoni F, Cereda M, Secondi R, et al. Vitrectomy for optic disc pit maculopathy: a long-term follow-up study. Graefes Arch Clin Exp Ophthalmol. 2018; 256:675–682.
Article10. Dai S, Polkinghorne P. Peeling the internal limiting membrane in serous macular detachment associated with congenital optic disc pit. Clin Exp Ophthalmol. 2003; 31:272–275.
Article11. Georgalas I, Petrou P, Koutsandrea C, et al. Optic disc pit maculopathy treated with vitrectomy, internal limiting membrane peeling, and gas tamponade: a report of two cases. Eur J Ophthalmol. 2009; 19:324–326.
Article12. Ishikawa K, Terasaki H, Mori M, et al. Optical coherence tomography before and after vitrectomy with internal limiting membrane removal in a child with optic disc pit maculopathy. Jpn J Ophthalmol. 2005; 49:411–413.
Article13. Seo JW, Nam DH, Lee DY. Case of macular hole after surgery in macular detachment with optic disc pit in a child. J Korean Ophthalmol Soc. 2013; 54:1135–1138.
Article14. Sobol WM, Blodi CF, Folk JC, Weingeist TA. Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology. 1990; 97:1539–1542.
Article15. Theodossiadis PG, Grigoropoulos VG, Emfietzoglou J, et al. Optical coherence tomography study of vitreoretinal interface in full thickness macular hole associated with optic disk pit maculopathy. Eur J Ophthalmol. 2007; 17:272–276.
Article16. Fantaguzzi P, Vasco A. Vitrectomy and silicone oil tamponade for serous macular detachment associated with an optic disk pit. Eur J Ophthalmol. 2006; 16:330–334.
Article17. Kiang L, Johnson MW. Formation of an intraretinal fluid barrier in cavitary optic disc maculopathy. Am J Ophthalmol. 2017; 173:34–44.
Article18. Gass JD. Serous detachment of the macula. Secondary to congenital pit of the optic nervehead. Am J Ophthalmol. 1969; 67:821–841.19. Monin C, Le Guen Y, Morel C, Haut J. Treatment of coloboma pits of the optic nerve complicated by serous detachment of the neuroepithelium. J Fr Ophtalmol. 1994; 17:574–579.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Optic Pit Maculopathy Treated with Fovea-sparing and an Inverted Flap Technique
- A Case of Vitrectomy without Laser for Serous Macular Detachment Associated with Optic Disc Pit
- A Case of Optic Disc Pit
- A Case of Serous Macular Detachment Associated with Tractional Fibrous Tissue in an Optic Pit Patient
- A Case of Surgically Treated Serous Macular Detachment Associated With Optic Disc Pit