Korean J Radiol.
2019 May;20(5):812-822. 10.3348/kjr.2018.0545.
MRI Evaluation of Suspected Pathologic Fracture at the Extremities from Metastasis: Diagnostic Value of Added Diffusion-Weighted Imaging
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. mhlee625@gmail.com
- 2Department of Radiology, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 3Department of Radiology, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- KMID: 2442715
- DOI: http://doi.org/10.3348/kjr.2018.0545
Abstract
OBJECTIVE
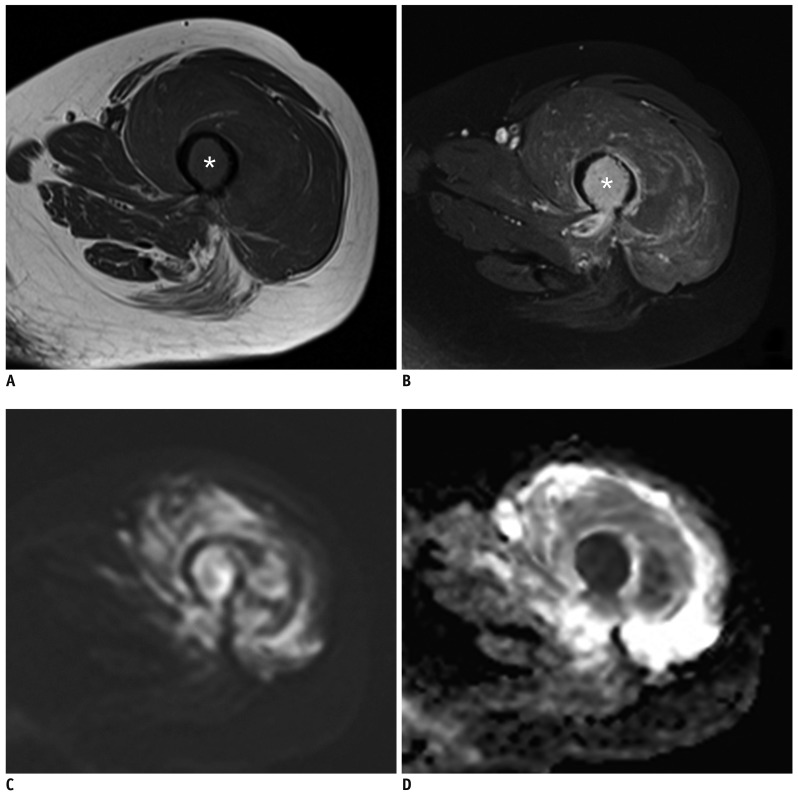
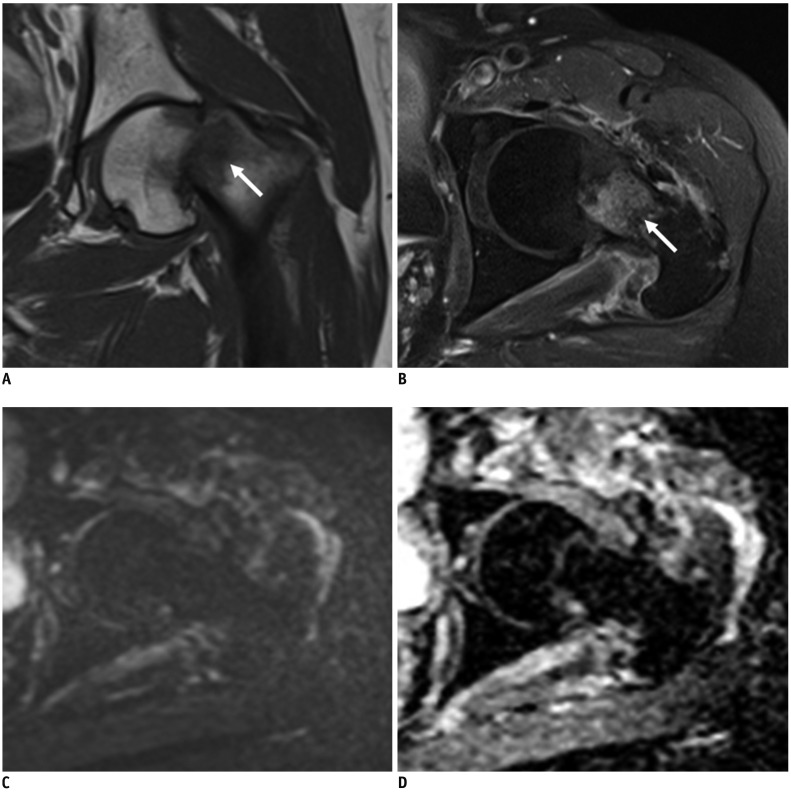
To assess the diagnostic value of combining diffusion-weighted imaging (DWI) with conventional magnetic resonance imaging (MRI) for differentiating between pathologic and traumatic fractures at extremities from metastasis.
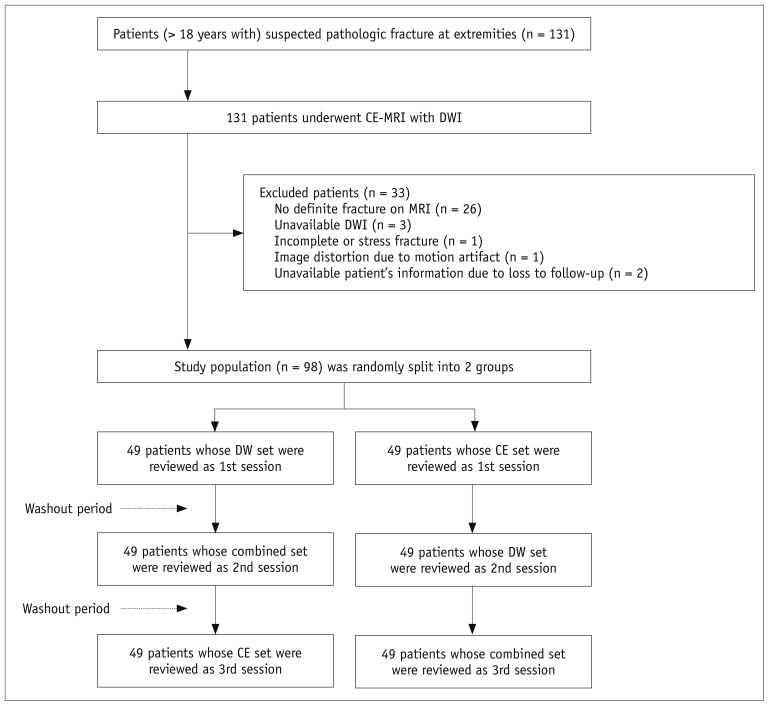
MATERIALS AND METHODS
Institutional Review Board approved this retrospective study and informed consent was waived. This study included 49 patients each with pathologic and traumatic fractures at extremities. The patients underwent conventional MRI combined with DWI. For qualitative analysis, two radiologists (R1 and R2) independently reviewed three imaging sets with a crossover design using a 5-point scale and a 3-scale confidence level: DWI plus non-enhanced MRI (NEMR; DW set), NEMR plus contrast-enhanced fat-saturated T1-weighted imaging (CEFST1; CE set), and DWI plus NEMR plus CEFST1 (combined set). McNemar's test was used to compare the diagnostic performances among three sets and perform subgroup analyses (single vs. multiple bone abnormality, absence/presence of extra-osseous mass, and bone enhancement at fracture margin).
RESULTS
Compared to the CE set, the combined set showed improved diagnostic accuracy (R1, 84.7 vs. 95.9%; R2, 91.8 vs. 95.9%, p < 0.05) and specificity (R1, 71.4% vs. 93.9%, p < 0.005; R2, 85.7% vs. 98%, p = 0.07), with no difference in sensitivities (p > 0.05). In cases of absent extra-osseous soft tissue mass and present fracture site enhancement, the combined set showed improved accuracy (R1, 82.9-84.4% vs. 95.6-96.3%, p < 0.05; R2, 90.2-91.1% vs. 95.1-95.6%, p < 0.05) and specificity (R1, 68.3-72.9% vs. 92.7-95.8%, p < 0.005; R2, 83.0-85.4% vs. 97.6-98.0%, p = 0.07).
CONCLUSION
Combining DWI with conventional MRI improved the diagnostic accuracy and specificity while retaining sensitivity for differentiating between pathologic and traumatic fractures from metastasis at extremities.
Keyword
MeSH Terms
Figure
Reference
-
1. Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer. 2007; 110:1860–1867. PMID: 17763372.
Article2. Ward WG, Spang J, Howe D. Metastatic disease of the femur. Surgical management. Orthop Clin North Am. 2000; 31:633–645. PMID: 11043102.3. Bae JH, Lee IS, Song YS, Kim JI, Cho KH, Lee SM, et al. Bone tumors with an associated pathologic fracture: differentiation between benign and malignant status using radiologic findings. J Korean Soc Radiol. 2015; 73:240–248.
Article4. Jung HS, Jee WH, McCauley TR, Ha KY, Choi KH. Discrimination of metastatic from acute osteoporotic compression spinal fractures with MR imaging. Radiographics. 2003; 23:179–187. PMID: 12533652.5. Baur A, Dietrich O, Reiser M. Diffusion-weighted imaging of bone marrow: current status. Eur Radiol. 2003; 13:1699–1708. PMID: 12759770.
Article6. Padhani AR, van Ree K, Collins DJ, D'Sa S, Makris A. Assessing the relation between bone marrow signal intensity and apparent diffusion coefficient in diffusion-weighted MRI. AJR Am J Roentgenol. 2013; 200:163–170. PMID: 23255758.
Article7. Lee SY, Jee WH, Jung JY, Park MY, Kim SK, Jung CK, et al. Differentiation of malignant from benign soft tissue tumours: use of additive qualitative and quantitative diffusion-weighted MR imaging to standard MR imaging at 3.0 T. Eur Radiol. 2016; 26:743–754. PMID: 26080796.
Article8. Zhou XJ, Leeds NE, McKinnon GC, Kumar AJ. Characterization of benign and metastatic vertebral compression fractures with quantitative diffusion MR imaging. AJNR Am J Neuroradiol. 2002; 23:165–170. PMID: 11827890.9. Geith T, Schmidt G, Biffar A, Dietrich O, Durr HR, Reiser M, et al. Comparison of qualitative and quantitative evaluation of diffusion-weighted MRI and chemical-shift imaging in the differentiation of benign and malignant vertebral body fractures. AJR Am J Roentgenol. 2012; 199:1083–1092. PMID: 23096183.
Article10. Sung JK, Jee WH, Jung JY, Choi M, Lee SY, Kim YH, et al. Differentiation of acute osteoporotic and malignant compression fractures of the spine: use of additive qualitative and quantitative axial diffusion-weighted MR imaging to conventional MR imaging at 3.0 T. Radiology. 2014; 271:488–449. PMID: 24484060.
Article11. Hamimi A, Kassab F, Kazkaz G. Osteoporotic or malignant vertebral fracture? This is the question. What can we do about it? The Egyptian Journal of Radiology and Nuclear Medicine. 2015; 46:97–103.
Article12. Bhugaloo A, Abdullah B, Siow Y, Ng K. Diffusion weighted MR imaging in acute vertebral compression fractures: differentiation between malignant and benign causes. Biomed Imaging Interv J. 2006; 2:e12. PMID: 21614224.
Article13. Abowarda MH, Abdel-Rahman HM, Taha MM. Differentiation of acute osteoporotic from malignant vertebral compression fractures with conventional MRI and diffusion MR imaging. The Egyptian Journal of Radiology and Nuclear Medicine. 2017; 48:207–213.
Article14. Del Grande F, Subhawong T, Weber K, Aro M, Mugera C, Fayad LM. Detection of soft-tissue sarcoma recurrence: added value of functional MR imaging techniques at 3.0 T. Radiology. 2014; 271:499–451. PMID: 24495264.
Article15. Kim SH, Lee JM, Hong SH, Kim GH, Lee JY, Han JK, et al. Locally advanced rectal cancer: added value of diffusion-weighted MR imaging in the evaluation of tumor response to neoadjuvant chemo- and radiation therapy. Radiology. 2009; 253:116–125. PMID: 19789256.
Article16. Park HJ, Lee SY, Rho MH, Chung EC, Kim MS, Kwon HJ, et al. Single-shot echo-planar diffusion-weighted MR imaging at 3T and 1.5T for differentiation of benign vertebral fracture edema and tumor infiltration. Korean J Radiol. 2016; 17:590–597. PMID: 27587948.
Article17. Kivrak AS, Paksoy Y, Erol C, Koplay M, Özbek S, Kara F. Comparison of apparent diffusion coefficient values among different MRI platforms: a multicenter phantom study. Diagn Interv Radiol. 2013; 19:433–437. PMID: 24004973.
Article18. Sasaki M, Yamada K, Watanabe Y, Matsui M, Ida M, Fujiwara S, et al. Variability in absolute apparent diffusion coefficient values across different platforms may be substantial: a multivendor, multi-institutional comparison study. Radiology. 2008; 249:624–630. PMID: 18936317.
Article19. Blazic IM, Lilic GB, Gajic MM. Quantitative assessment of rectal cancer response to neoadjuvant combined chemotherapy and radiation therapy: comparison of three methods of positioning region of interest for ADC measurements at diffusion-weighted MR imaging. Radiology. 2017; 282:615.
Article20. Ahlawat S, Khandheria P, Del Grande F, Morelli J, Subhawong TK, Demehri S, et al. Interobserver variability of selective region-of-interest measurement protocols for quantitative diffusion weighted imaging in soft tissue masses: comparison with whole tumor volume measurements. J Magn Reson Imaging. 2016; 43:446–454. PMID: 26174705.
Article21. Braithwaite AC, Dale BM, Boll DT, Merkle EM. Short- and midterm reproducibility of apparent diffusion coefficient measurements at 3.0-T diffusion-weighted imaging of the abdomen. Radiology. 2009; 250:459–465. PMID: 19095786.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adnexal Masses: Clinical Application of Multiparametric MR Imaging & O-RADS MRI
- The Value of PROPELLER Diffusion-Weighted Image in the Detection of Cholesteatoma
- Evaluation of Treatment Response Using Diffusion-Weighted MRI in Metastatic Spines
- Single-Shot Echo-Planar Diffusion-Weighted MR Imaging at 3T and 1.5T for Differentiation of Benign Vertebral Fracture Edema and Tumor Infiltration
- Bilateral Medial Medullary Infarction Demonstrated by Diffusion-Weighted Imaging: Case Report