J Korean Soc Radiol.
2019 Jan;80(1):98-104. 10.3348/jksr.2019.80.1.98.
The Effectiveness of Pelvic Arterial Embolization for Intractable Postpartum Hemorrhage after Hysterectomy
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Hospital, Bucheon, Korea. jspark@schmc.ac.kr
- KMID: 2442468
- DOI: http://doi.org/10.3348/jksr.2019.80.1.98
Abstract
- PURPOSE
To evaluate the effectiveness of pelvic arterial embolization (PAE) for intractable postpartum hemorrhage (PPH) after hysterectomy.
MATERIALS AND METHODS
From March 2011 to December 2017, 14 patients who received PAE for PPH that persisted after total abdominal hysterectomy were included (mean age, 33.6 years; range, 26-37 years). The delivery type, cause of PPH, and angiographic findings were investigated. The technical and clinical success rates and clinical outcomes were evaluated.
RESULTS
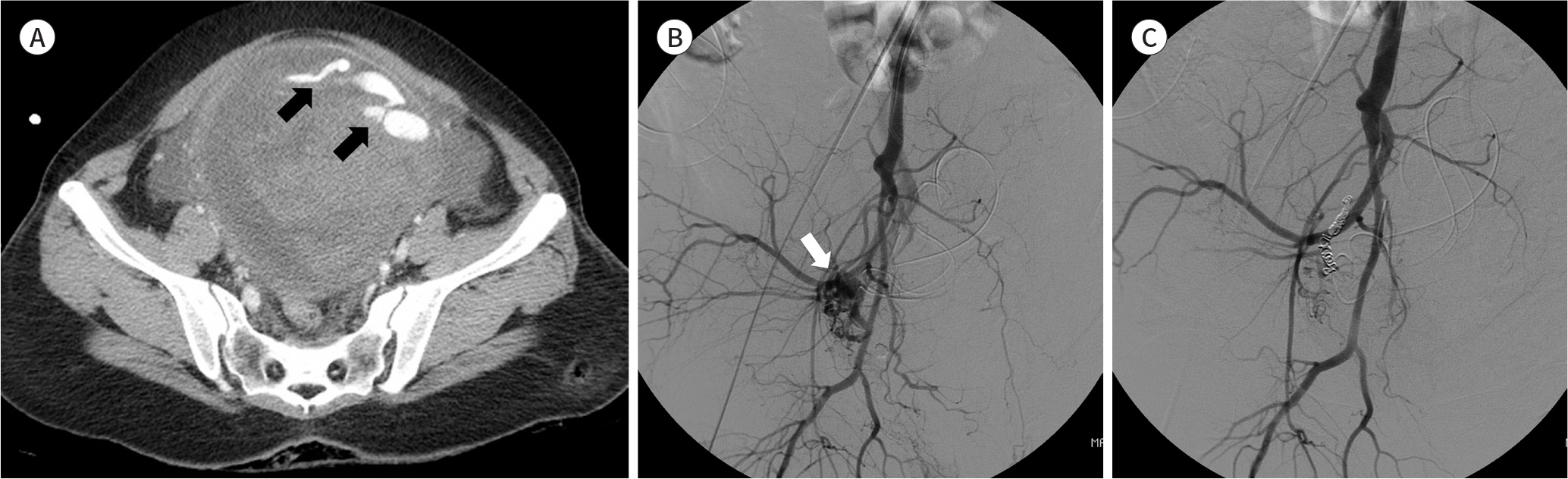
Of 14 patients, 8 patients (57%) had positive angiographic findings for bleeding; contrast extravasation (n = 6), and pseudoaneurysm (n = 2). Remnant uterine artery (UA) was the most common bleeding focus (n = 4), followed by vaginal artery (n = 2), left lateral sacral artery (n = 1), and left internal pudendal artery (n = 1). Technical and clinical success rates were 100% and 93% (13/14), respectively. In 1 patient, bleeding was not controlled after initial selective embolization and the entire anterior divisions of both internal iliac arteries were embolized with gelfoam.
CONCLUSION
PAE for persistent PPH after hysterectomy is a safe and effective treatment. Remnant UA was the most common bleeding site and all patients recovered without any significant sequelae after embolization.
MeSH Terms
Figure
Reference
-
References
1. Al-Zirqi I, Vangen S, Forsen L, Stray-Pedersen B. Prevalence and risk factors of severe obstetric haemorrhage. BJOG. 2008; 115:1265–1272.
Article2. Lee HY, Shin JH, Kim J, Yoon HK, Ko GY, Won HS, et al. Primary postpartum hemorrhage: outcome of pelvic arterial embolization in 251 patients at a single institution. Radiology. 2012; 264:903–909.
Article3. Soyer P, Dohan A, Dautry R, Guerrache Y, Ricbourg A, Gayat E, et al. Transcatheter arterial embolization for postpartum hemorrhage: indications, technique, results, and complications. Cardiovasc Intervent Radiol. 2015; 38:1068–1081.
Article4. Gonsalves M, Belli A. The role of interventional radiology in obstetric hemorrhage.Cardiovasc Intervent Radiol. 2010; 33:887–895.5. Deux JF, Bazot M, Le Blanche AF, Tassart M, Khalil A, Berkane N, et al. Is selective embolization of uterine arteries a safe alternative to hysterectomy in patients with postpartum hemorrhage? AJR Am J Roentgenol. 2001; 177:145–149.
Article6. Dahlke JD, Mendez-Figueroa H, Maggio L, Hauspurg AK, Sperling JD, Chauhan SP, et al. Prevention and management of postpartum hemorrhage: a comparison of 4 national guidelines.Am J Obstet Gynecol. 2015; 213:76.e1–76. .e10.7. Oei PL, Chua S, Tan L, Ratnam SS, Arulkumaran S. Arterial embolization for bleeding following hysterectomy for intractable postpartum hemorrhage. Int J Gynaecol Obstet. 1998; 62:83–86.
Article8. Collins CD, Jackson JE. Pelvic arterial embolization following hysterectomy and bilateral internal iliac artery ligation for intractable primary post partum haemorrhage. Clin Radiol. 1995; 50:710–713. ; discussion 713–714.
Article9. Naydich M, Friedman A, Aaron G, Silberzweig J. Arterial embolization of vaginal arterial branches for severe postpartum hemorrhage despite hysterectomy. J Vasc Interv Radiol. 2007; 18:1047–1050.
Article10. Sentilhes L, Gromez A, Clavier E, Resch B, Verspyck E, Marpeau L. Predictors of failed pelvic arterial embolization for severe postpartum hemorrhage. Obstet Gynecol. 2009; 113:992–999.
Article11. Touboul C, Badiou W, Saada J, Pelage JP, Payen D, Vicaut E, et al. Efficacy of selective arterial embolisation for the treatment of life-threatening postpartum haemorrhage in a large population.PLoS One. 2008; 3:e3819.12. Committee on Practice Bulletins-Obstetrics. Practice bulletin no. 183: postpartum hemorrhage. Obstet Gynecol. 2017; 130:e168–e186.13. Fargeaudou Y, Morel O, Soyer P, Gayat E, Sirol M, Boudiaf M, et al. Persistent postpartum haemorrhage after failed arterial ligation: value of pelvic embolisation. Eur Radiol. 2010; 20:1777–1785.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of failed arterial embolization for postpartum hemorrhage
- The indications, effectiveness and complications of the selective arterial embolization in the management of obstetrical hemorrhage
- Inferior Mesenteric Artery Embolization with N-Butyl Cyanoacrylate for Life-Threatening Postpartum Hemorrhage: A Report of Two Cases and Literature Review
- A Case of Successful Percutaneous Transarterial Embolization to Injured Pelvic Artery after Vaginal Delivery
- Recent Trends in the Management of Postpartum Hemorrhage