J Korean Diabetes.
2019 Mar;20(1):57-61. 10.4093/jkd.2019.20.1.57.
An Unusual Case of Bilateral Peripheral Edema in a Male with Undiagnosed Type 2 Diabetes Mellitus
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Presbyterian Medical Center, Jeonju, Korea. wisdom0165@gmail.com
- KMID: 2442355
- DOI: http://doi.org/10.4093/jkd.2019.20.1.57
Abstract
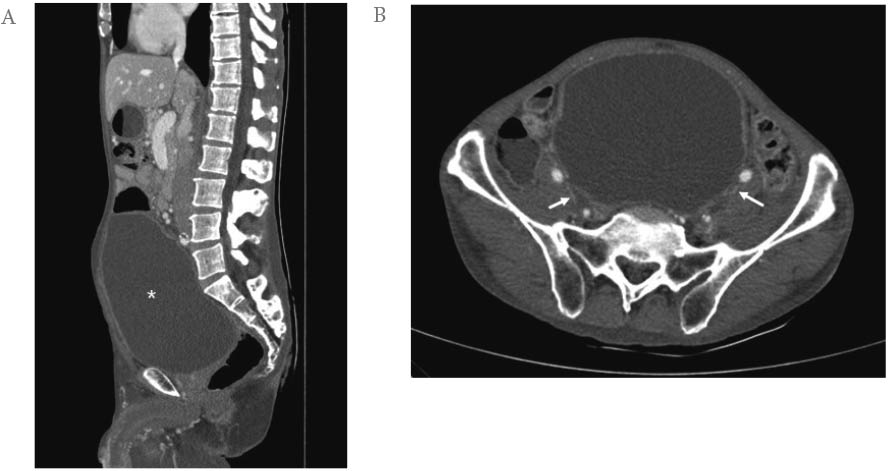
- The present article demonstrates an unusual case of bilateral lower extremity edema caused by neurogenic areflexic bladder as the first physical symptom of diabetes. A 52-year-old man presented to the emergency department because of massive edema of his lower limbs. The edema had been present for 2 weeks, was symmetrical, and was progressively covering the lower limbs up to the inguinal area, scrotal bag, and penis and was accompanied by dysuria and an interrupted urine stream. Laboratory findings revealed a serum glucose level of 657 mg/dL and glycated hemoglobin (HbA1c) level of 15.6%. Computed tomography (CT) of the abdomen and pelvis revealed marked enlargement of the bladder with bilateral hydronephrosis and hydroureter. In addition, CT demonstrated bilateral compression of the iliac veins caused by the enlarged bladder. This case highlights the importance of a broad differential diagnosis for patients with diabetes and extensive peripheral edema. Neurogenic bladder should be considered in the differential diagnosis, even in newly diagnosed diabetic patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Spijkerman AM, Dekker JM, Nijpels G, Adriaanse MC, Kostense PJ, Ruwaard D, Stehouwer CD, Bouter LM, Heine RJ. Microvascular complications at time of diagnosis of type 2 diabetes are similar among diabetic patients detected by targeted screening and patients newly diagnosed in general practice: the hoorn screening study. Diabetes Care. 2003; 26:2604–2608.
Article2. Chudzik W, Kaczorowska B, Przybyla M, Chudzik B, Galka M. [Diabetic neuropathy]. Pol Merkur Lekarski. 2007; 22:66–69. Polish.3. Ely JW, Osheroff JA, Chambliss ML, Ebell MH. Approach to leg edema of unclear etiology. J Am Board Fam Med. 2006; 19:148–160.
Article4. Carlsson E, Garsten P. Compression of the common iliac vessels by dilatation of the bladder. Report of a case. Acta radiol. 1960; 53:449–453.
Article5. Palma L, Peterson MC, Ingebretsen R. Iliac vein compression syndrome from urinary bladder distension due to prostatism. South Med J. 1995; 88:959–960.
Article6. Evans JM, Owens TP Jr, Zerbe DM, Rohren CH. Venous obstruction due to a distended urinary bladder. Mayo Clin Proc. 1995; 70:1077–1079.
Article7. Kebapci N, Yenilmez A, Efe B, Entok E, Demirustu C. Bladder dysfunction in type 2 diabetic patients. Neurourol Urodyn. 2007; 26:814–819.
Article8. Golbidi S, Laher I. Bladder dysfunction in diabetes mellitus. Front Pharmacol. 2010; 1:136.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter: The Necessity of the Simple Tests for Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus Patients without Neuropathic Symptoms in Clinical Practice (Diabetes Metab J 2018;42:442-6)
- Response: The Necessity of the Simple Tests for Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus Patients without Neuropathic Symptoms in Clinical Practice (Diabetes Metab J 2018;42:442–6)
- A Case of Bilateral Bell's Palsy with Uncontrolled Diabetes Mellitus
- Response: The Prevalence of Peripheral Arterial Disease in Korean Patients with Type 2 Diabetes Mellitus Attending a University Hospital (Diabetes Metab J 2011;35:543-50)
- Peripheral Arterial Disease in Patients with Type 2 Diabetes Mellitus