Anat Cell Biol.
2019 Mar;52(1):57-68. 10.5115/acb.2019.52.1.57.
Effects of targeted remediation in anatomy for first year medical students
- Affiliations
-
- 1Department of Anatomy, St. John's Medical College, Bangalore, India. nachiket76@gmail.com
- 2Department of Psychiatry, Topiwala National Medical College & BYL Nair Charitable Hospital, Mumbai, India.
- KMID: 2442330
- DOI: http://doi.org/10.5115/acb.2019.52.1.57
Abstract
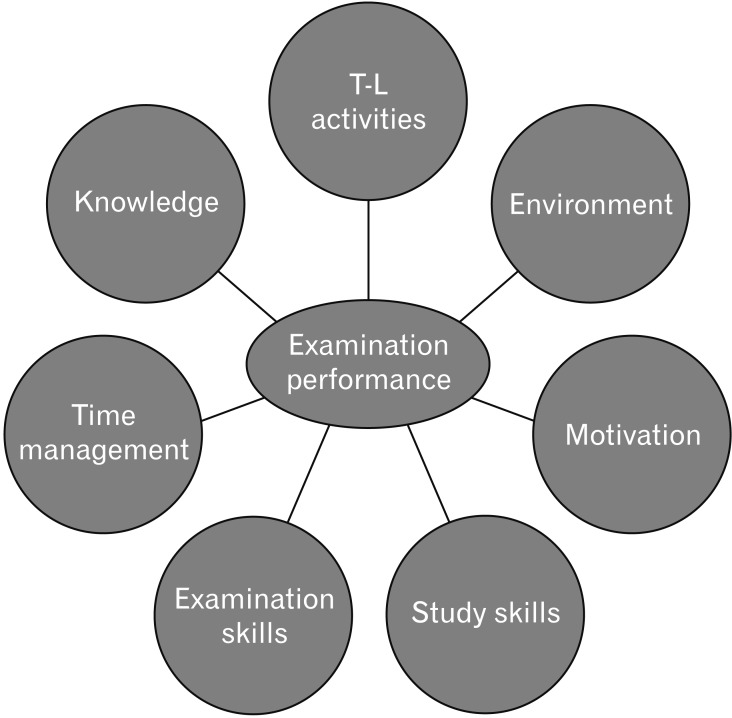
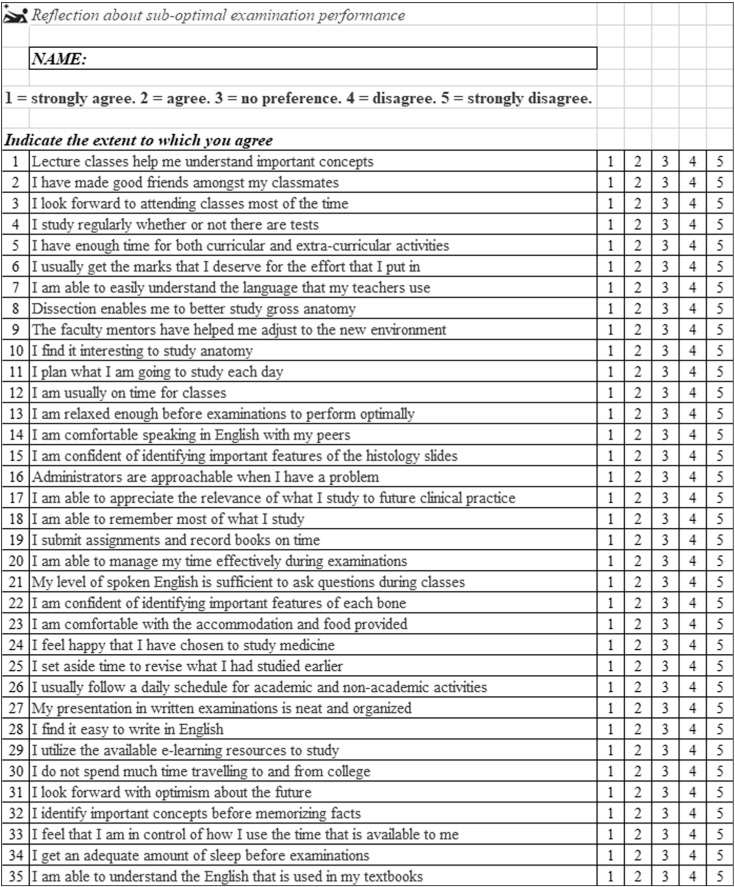
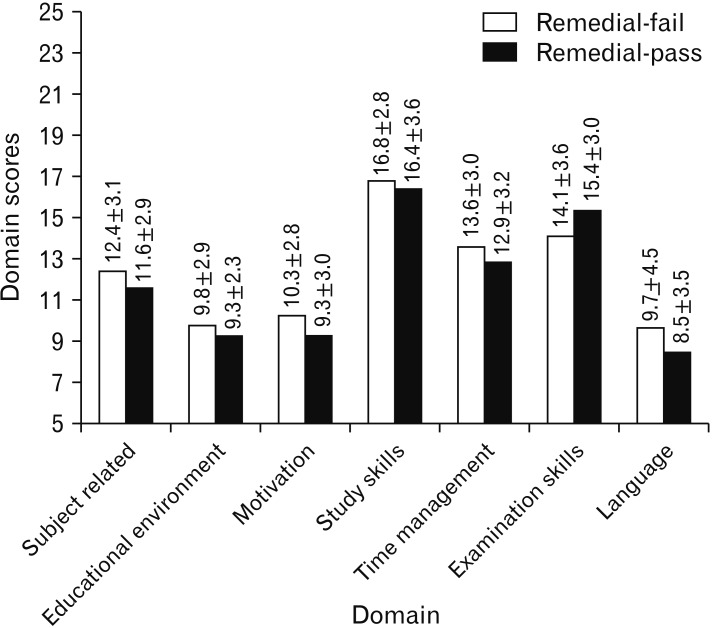
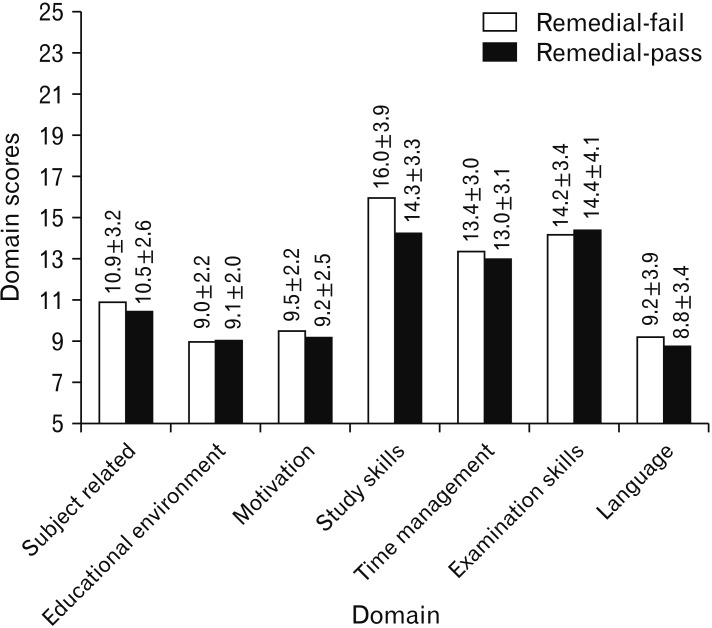
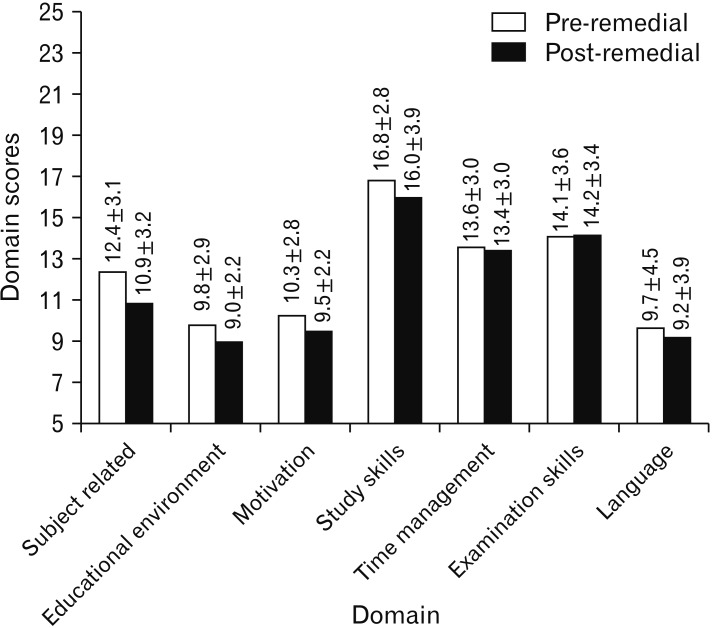
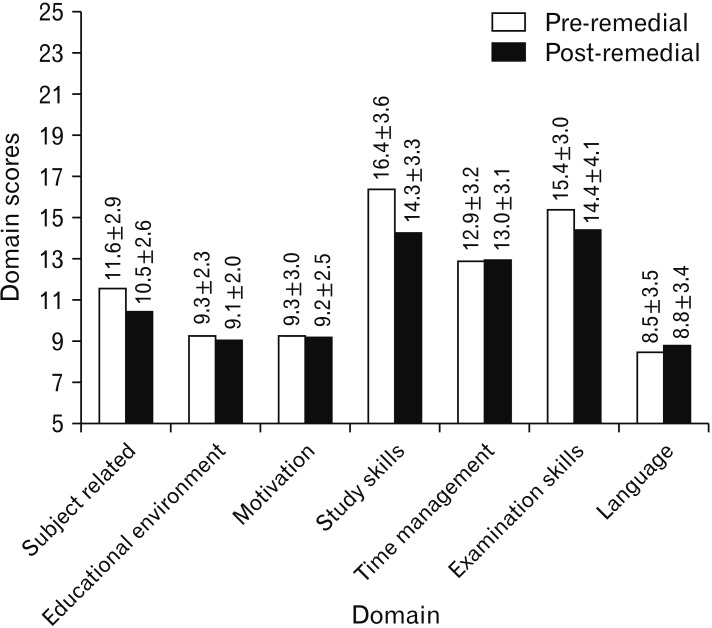
- The aim of this study was to assess the effectiveness of a questionnaire to guide targeted remediation among undergraduate medical students in anatomy. Seventy-five students from a medical college in South India who failed in the first internal theory examination were administered a validated 35-item questionnaire. The total and domain specific questionnaire scores were calculated. Specific weekly interventions for each student based on the questionnaire scores were conducted by appointed academic mentors for three months prior to the second internal examination. The dependent variable was performance in the second internal examination. The students were re-administered the questionnaire after the second internal examination. The independent variables were the marks obtained in the first internal examination, domain specific and total questionnaire scores, sex, and regularity of the student in attending the remedial sessions. Inferential statistical tests used were the chi-square test, independent sample t test, paired t test, multiple regression and binomial logistic regression. Of the 75 students who underwent remediation, 54 (72%) passed in the second internal examination. The scores in the second internal examination among these students was found to be significantly higher as compared to the first internal examination. The total, subject related and study skills questionnaire score were significantly lower after remediation. Students who were irregular had a significantly lower pass rate. The multivariate analysis showed that only the first internal marks added significantly to the prediction about second internal performance. This study provides evidence to show that struggling students perceive a benefit from targeted remediation.
MeSH Terms
Figure
Reference
-
1. Yates J, James D. Predicting the “strugglers”: a case-control study of students at Nottingham University Medical School. BMJ. 2006; 332:1009–1013. PMID: 16543299.2. Yates J. Development of a ‘toolkit’ to identify medical students at risk of failure to thrive on the course: an exploratory retrospective case study. BMC Med Educ. 2011; 11:95. PMID: 22098629.3. Cleland J, Leggett H, Sandars J, Costa MJ, Patel R, Moffat M. The remediation challenge: theoretical and methodological insights from a systematic review. Med Educ. 2013; 47:242–251. PMID: 23398010.4. Szumacher E, Catton P, Jones GA, Bradley R, Kwan J, Cherryman F, Palmer C, Nyhof-Young J. Helping learners in difficulty--the incidence and effectiveness of remedial programmes of the Medical Radiation Sciences Programme at University of Toronto and the Michener Institute for Applied Sciences, Toronto, Ontario, Canada. Ann Acad Med Singapore. 2007; 36:725–734. PMID: 17925980.5. James D, Yates J, Ferguson E. Can the 12-item General Health Questionnaire be used to identify medical students who might ‘struggle’ on the medical course? A prospective study on two cohorts. BMC Med Educ. 2013; 13:48. PMID: 23548161.6. Ranasinghe P, Ellawela A, Gunatilake SB. Non-cognitive characteristics predicting academic success among medical students in Sri Lanka. BMC Med Educ. 2012; 12:66. PMID: 22863153.7. Boyles L. Exploration of a retention model for community college students. Greensboro, NC: The University of North Carolina;2000.8. Seidman A. College student retention: formula for student success. Westport, CT: Praeger;2005. p. 295–316.9. Maher BM, Hynes H, Sweeney C, Khashan AS, O'Rourke M, Doran K, Harris A, Flynn SO. Medical school attrition-beyond the statistics a ten year retrospective study. BMC Med Educ. 2013; 13:13. PMID: 23363547.10. Boyd H, Westfall R. Marketing research: text and cases. Homewood, IL: R.D. Irwin Inc.;1972.11. Boileau E, St-Onge C, Audétat MC. Is there a way for clinical teachers to assist struggling learners? A synthetic review of the literature. Adv Med Educ Pract. 2017; 8:89–97. PMID: 28176916.12. Maize DF, Fuller SH, Hritcko PM, Matsumoto RR, Soltis DA, Taheri RR, Duncan W. A review of remediation programs in pharmacy and other health professions. Am J Pharm Educ. 2010; 74:25. PMID: 20414438.13. Smith JL, Lypson M, Silverberg M, Weizberg M, Murano T, Lukela M, Santen SA. Defining uniform processes for remediation, probation and termination in residency training. West J Emerg Med. 2017; 18:110–113. PMID: 28116019.14. Egwu OA, Anyanwu GE. Five-year survey of medical student attrition in a medical school in Nigeria: a pilot study. Adv Med Educ Pract. 2010; 1:53–57. PMID: 23745063.15. Cleland J, Arnold R, Chesser A. Failing finals is often a surprise for the student but not the teacher: identifying difficulties and supporting students with academic difficulties. Med Teach. 2005; 27:504–508. PMID: 16199356.16. Singh T. Commercialisation of medical education: a review of capitation fee colleges. J Indian Med Assoc. 1994; 92:301–303. PMID: 7814906.17. Batmanabane G. When angels fall...are we lowering the standards of medical education in India? J Pharmacol Pharmacother. 2013; 4:1–3. PMID: 23662016.18. Baars GJ, Stijnen T, Splinter TA. A model to predict student failure in the first year of the undergraduate medical curriculum. Health Prof Educ. 2017; 3:5–14.19. Denison AR, Currie AE, Laing MR, Heys SD. Good for them or good for us? The role of academic guidance interviews. Med Educ. 2006; 40:1188–1191. PMID: 17118112.20. McLaughlin K, Veale P, McIlwrick J, de Groot J, Wright B. A practical approach to mentoring students with repeated performance deficiencies. BMC Med Educ. 2013; 13:56. PMID: 23597111.21. Bierer SB, Dannefer EF, Tetzlaff JE. Time to loosen the apron strings: cohort-based evaluation of a learner-driven remediation model at one medical school. J Gen Intern Med. 2015; 30:1339–1343. PMID: 26173525.22. Artino AR Jr, Hemmer PA, Durning SJ. Using self-regulated learning theory to understand the beliefs, emotions, and behaviors of struggling medical students. Acad Med. 2011; 86(10 Suppl):S35–S38. PMID: 21955765.23. Dattathreya P, Shillingford S. Identifying the ineffective study strategies of first year medical school students. Med Sci Educ. 2017; 27:295–307.24. Bickerdike A, O'Deasmhunaigh C, O'Flynn S, O'Tuathaigh C. Learning strategies, study habits and social networking activity of undergraduate medical students. Int J Med Educ. 2016; 7:230–236. PMID: 27424041.25. Das M, Maity S, Gupta S, Mondal A, Dolui SK, Banerjee P, Roy RK. Performance improvement in examination by re-teaching the underperforming undergraduate medical students. Int J Pharm Med Res. 2015; 3:242–245.26. Guerrasio J, Garrity MJ, Aagaard EM. Learner deficits and academic outcomes of medical students, residents, fellows, and attending physicians referred to a remediation program, 2006-2012. Acad Med. 2014; 89:352–358. PMID: 24362382.27. Hortsch M, Mangrulkar RS. When students struggle with gross anatomy and histology: a strategy for monitoring, reviewing, and promoting student academic success in an integrated preclinical medical curriculum. Anat Sci Educ. 2015; 8:478–483. PMID: 25641923.28. Winston KA, Van Der Vleuten CP, Scherpbier AJ. At-risk medical students: implications of students' voice for the theory and practice of remediation. Med Educ. 2010; 44:1038–1047. PMID: 20880373.29. Winston KA, Van Der Vleuten CP, Scherpbier AJ. Remediation of at-risk medical students: theory in action. BMC Med Educ. 2013; 13:132. PMID: 24070196.30. Walke YS, Samuel LJ, Rataboli PV. The prospective assessment of remedial intervention on improvement of academic performance of at risk second year medical students in pharmacology. Int J Curr Res Acad Rev. 2017; 3:86–91.31. Meinel FG, Dimitriadis K, von der Borch P, Störmann S, Niedermaier S, Fischer MR. More mentoring needed? A cross-sectional study of mentoring programs for medical students in Germany. BMC Med Educ. 2011; 11:68. PMID: 21943281.32. Winston KA, Van der Vleuten CP, Scherpbier AJ. An investigation into the design and effectiveness of a mandatory cognitive skills programme for at-risk medical students. Med Teach. 2010; 32:236–243. PMID: 20218839.33. Stegers-Jager KM, Cohen-Schotanus J, Themmen AP. The effect of a short integrated study skills programme for first-year medical students at risk of failure: a randomised controlled trial. Med Teach. 2013; 35:120–126. PMID: 23110355.34. Guerrasio J, Aagaard EM. Methods and outcomes for the remediation of clinical reasoning. J Gen Intern Med. 2014; 29:1607–1614. PMID: 25092006.35. Nixon LJ, Gladding SP, Duffy BL. Describing failure in a clinical clerkship: implications for identification, assessment and remediation for struggling learners. J Gen Intern Med. 2016; 31:1172–1179. PMID: 27271729.36. Schutte AF. Who is repeating anatomy? Trends in an undergraduate anatomy course. Anat Sci Educ. 2016; 9:171–178. PMID: 26179910.37. Patel RS, Tarrant C, Bonas S, Shaw RL. Medical students' personal experience of high-stakes failure: case studies using interpretative phenomenological analysis. BMC Med Educ. 2015; 15:86. PMID: 25964102.38. Garrud P, Yates J. Profiling strugglers in a graduate-entry medicine course at Nottingham: a retrospective case study. BMC Med Educ. 2012; 12:124. PMID: 23249471.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is remediation program using team-based learning effective for at-risk medical students?
- Clinical-Performance Remediation Program for Dyscompetent Medical Students
- Deliberate Practice as an Effective Remediation Strategy for Underperforming Medical Students Focused on Clinical Skills: a Prospective Longitudinal Study
- “Food for Thought”: Improving Cognition in People With Schizophrenia
- “Food for Thought”: Improving Cognition in People With Schizophrenia