J Breast Cancer.
2019 Mar;22(1):120-130. 10.4048/jbc.2019.22.e1.
Central Nervous System Failure in Korean Breast Cancer Patients with HER2-Enriched Subtype: Korean Radiation Oncology Group 16-15 Multicenter Retrospective Study
- Affiliations
-
- 1Department of Radiation Oncology, Ewha Womans University College of Medicine, Seoul, Korea.
- 2Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. inah228@snu.ac.kr
- 3Department of Radiation Oncology, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Radiation Oncology, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Radiation Oncology, Gachon University Gil Medical Center, Incheon, Korea.
- 6Department of Radiation Oncology, Keimyung University College of Medicine, Daegu, Korea.
- 7Department of Radiation Oncology, Presbyterian Medical Center, Jeonju, Korea.
- 8Department of Radiation Oncology, Chonbuk National University Hospital, Jeonju, Korea.
- 9Department of Radiation Oncology, Chung-Ang University Hospital, Seoul, Korea.
- KMID: 2441857
- DOI: http://doi.org/10.4048/jbc.2019.22.e1
Abstract
- PURPOSE
The purpose of this study was to evaluate the risk of central nervous system (CNS) failure in Korean patients with human epidermal growth factor receptor 2 (HER2)-enriched breast cancer treated with surgery followed by postoperative radiotherapy (RT).
METHODS
A total of 749 patients from eight institutions were enrolled in this study. All of them underwent surgery followed by postoperative RT from 2003 to 2011; 246 (32.8%) received neoadjuvant chemotherapy and 649 (81.7%) received adjuvant chemotherapy. Adjuvant trastuzumab was administered to 386 patients (48.6%).
RESULTS
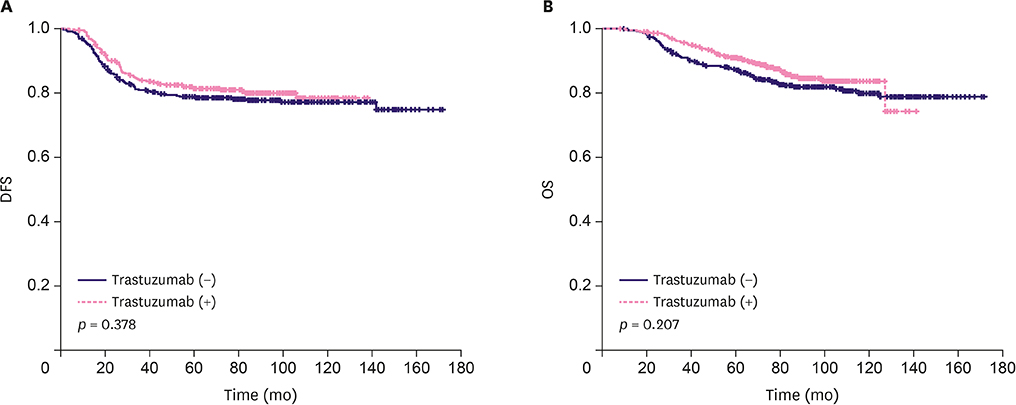
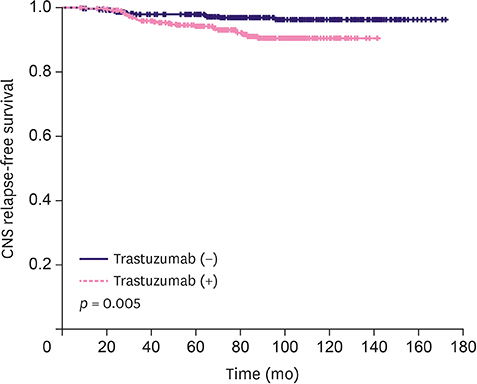
The median follow-up duration was 84 (range, 8-171) months. The 7-year disease-free and overall survival rates were 79.0% and 84.2%, respectively. On multivariate analysis, mastectomy, nodal involvement, and presence of lymphatic invasion were correlated with poor overall survival (p = 0.004, 0.022, and 0.011, respectively), whereas T stage and lymphatic invasion were associated with disease-free survival (p = 0.018 and 0.005, respectively). Regarding CNS failures, 30 brain metastases, 2 leptomeningeal metastases, and 8 brain and leptomeningeal metastases were noted. The 7-year CNS relapse-free survival rates in patients receiving and not receiving trastuzumab were 91.2% and 96.9%, respectively (p = 0.005). On multivariate analysis, the administration of adjuvant trastuzumab was the only prognostic factor in predicting a higher CNS failure rate (hazard ratio, 2.260; 95% confidence interval, 1.076-4.746; p = 0.031).
CONCLUSION
Adjuvant trastuzumab was associated with higher CNS failure rate in Korean patients with HER2-enriched breast cancer. Close monitoring and reasonable approaches such as CNS penetrating HER2 blockades combined with the current standard therapy could contribute to improving intracranial tumor control and quality of life in patients with CNS metastasis from HER2-enriched breast cancer.
Keyword
MeSH Terms
-
Brain
Breast Neoplasms*
Breast*
Central Nervous System Neoplasms
Central Nervous System*
Chemotherapy, Adjuvant
Disease-Free Survival
Drug Therapy
Follow-Up Studies
Humans
Mastectomy
Multivariate Analysis
Neoplasm Metastasis
Quality of Life
Radiation Oncology*
Radiotherapy
Receptor, Epidermal Growth Factor
Retrospective Studies*
Survival Rate
Trastuzumab
Receptor, Epidermal Growth Factor
Trastuzumab
Figure
Reference
-
1. Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987; 235:177–182.
Article2. Cameron D, Piccart-Gebhart MJ, Gelber RD, Procter M, Goldhirsch A, de Azambuja E, et al. 11 years' follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin Adjuvant (HERA) trial. Lancet. 2017; 389:1195–1205.
Article3. Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE Jr, Davidson NE, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005; 353:1673–1684.
Article4. Vogel CL, Cobleigh MA, Tripathy D, Gutheil JC, Harris LN, Fehrenbacher L, et al. Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol. 2002; 20:719–726.
Article5. National Comprehensive Cancer Network. Breast cancer (version 1.2018). Accessed May 1st, 2018. https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf.6. Kallioniemi OP, Holli K, Visakorpi T, Koivula T, Helin HH, Isola JJ. Association of c-erbB-2 protein over-expression with high rate of cell proliferation, increased risk of visceral metastasis and poor long-term survival in breast cancer. Int J Cancer. 1991; 49:650–655.
Article7. Aragon-Ching JB, Zujewski JA. CNS metastasis: an old problem in a new guise. Clin Cancer Res. 2007; 13:1644–1647.
Article8. Pestalozzi BC, Zahrieh D, Price KN, Holmberg SB, Lindtner J, Collins J, et al. Identifying breast cancer patients at risk for Central Nervous System (CNS) metastases in trials of the International Breast Cancer Study Group (IBCSG). Ann Oncol. 2006; 17:935–944.
Article9. Bendell JC, Domchek SM, Burstein HJ, Harris L, Younger J, Kuter I, et al. Central nervous system metastases in women who receive trastuzumab-based therapy for metastatic breast carcinoma. Cancer. 2003; 97:2972–2977.
Article10. Clayton AJ, Danson S, Jolly S, Ryder WD, Burt PA, Stewart AL, et al. Incidence of cerebral metastases in patients treated with trastuzumab for metastatic breast cancer. Br J Cancer. 2004; 91:639–643.
Article11. Bria E, Cuppone F, Fornier M, Nisticò C, Carlini P, Milella M, et al. Cardiotoxicity and incidence of brain metastases after adjuvant trastuzumab for early breast cancer: the dark side of the moon? A meta-analysis of the randomized trials. Breast Cancer Res Treat. 2008; 109:231–239.
Article12. Musolino A, Ciccolallo L, Panebianco M, Fontana E, Zanoni D, Bozzetti C, et al. Multifactorial central nervous system recurrence susceptibility in patients with HER2-positive breast cancer: epidemiological and clinical data from a population-based cancer registry study. Cancer. 2011; 117:1837–1846.
Article13. Pestalozzi BC, Holmes E, de Azambuja E, Metzger-Filho O, Hogge L, Scullion M, et al. CNS relapses in patients with HER2-positive early breast cancer who have and have not received adjuvant trastuzumab: a retrospective substudy of the HERA trial (BIG 1-01). Lancet Oncol. 2013; 14:244–248.
Article14. Lim YJ, Lee SW, Choi N, Kwon J, Eom KY, Kang E, et al. Failure patterns according to molecular subtype in patients with invasive breast cancer following postoperative adjuvant radiotherapy: long-term outcomes in contemporary clinical practice. Breast Cancer Res Treat. 2017; 163:555–563.
Article15. Escrivá-de-Romaní S, Arumí M, Bellet M, Saura C. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Breast. 2018; 39:80–88.16. Burstein HJ, Lieberman G, Slamon DJ, Winer EP, Klein P. Isolated central nervous system metastases in patients with HER2-overexpressing advanced breast cancer treated with first-line trastuzumab-based therapy. Ann Oncol. 2005; 16:1772–1777.
Article17. Gori S, Rimondini S, De Angelis V, Colozza M, Bisagni G, Moretti G, et al. Central nervous system metastases in HER-2 positive metastatic breast cancer patients treated with trastuzumab: incidence, survival, and risk factors. Oncologist. 2007; 12:766–773.
Article18. Patanaphan V, Salazar OM, Risco R. Breast cancer: metastatic patterns and their prognosis. South Med J. 1988; 81:1109–1112.19. Tsukada Y, Fouad A, Pickren JW, Lane WW. Central nervous system metastasis from breast carcinoma. Autopsy study. Cancer. 1983; 52:2349–2354.
Article20. Koo T, Kim IA. Brain metastasis in human epidermal growth factor receptor 2-positive breast cancer: from biology to treatment. Radiat Oncol J. 2016; 34:1–9.
Article21. Hamy AS, Lam GT, Laas E, Darrigues L, Balezeau T, Guerin J, et al. Lymphovascular invasion after neoadjuvant chemotherapy is strongly associated with poor prognosis in breast carcinoma. Breast Cancer Res Treat. 2018; 169:295–304.
Article22. Kim YJ, Kim JS, Kim IA. Molecular subtype predicts incidence and prognosis of brain metastasis from breast cancer in SEER database. J Cancer Res Clin Oncol. 2018; 144:1803–1816.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The current status of cancer survivorship care and a consideration of appropriate care model in Korea
- Effective Treatment of Solitary Pituitary Metastasis with Panhypopituitarism in HER2-Positive Breast Cancer by Lapatinib
- Clinical Differences in Triple-Positive Operable Breast Cancer Subtypes in Korean Patients: An Analysis of Korean Breast Cancer Registry Data
- Predictive Value of Molecular Subtyping for Locoregional Recurrence in Early-Stage Breast Cancer with N1 without Postmastectomy Radiotherapy
- Molecular subtypes and imaging phenotypes of breast cancer