J Breast Cancer.
2019 Mar;22(1):67-76. 10.4048/jbc.2019.22.e8.
Determining Whether High Nodal Burden in Early Breast Cancer Patients Can Be Predicted Preoperatively to Avoid Sentinel Lymph Node Biopsy
- Affiliations
-
- 1Breast Department, KK Women's and Children's Hospital, Singapore. ghlimsg@yahoo.com.sg
- 2Duke-NUS Medical School, Singapore.
- 3Department of Diagnostic & Interventional Imaging, KK Women's and Children's Hospital, Singapore.
- 4Centre for Quantitative Medicine, Duke NUS Medical School, Singapore.
- 5Department of Diagnostic Radiology, Singapore General Hospital, Singapore.
- KMID: 2441852
- DOI: http://doi.org/10.4048/jbc.2019.22.e8
Abstract
- PURPOSE
The Z0011 trial showed that axillary lymph node dissection (ALND) can be safely avoided in breast cancer patients with low nodal burden (LNB). ALND can be performed in patients with high nodal burden (HNB). We aimed to determine whether HNB in early breast cancer patients can be predicted preoperatively to avoid sentinel lymph node biopsy (SLNB).
METHODS
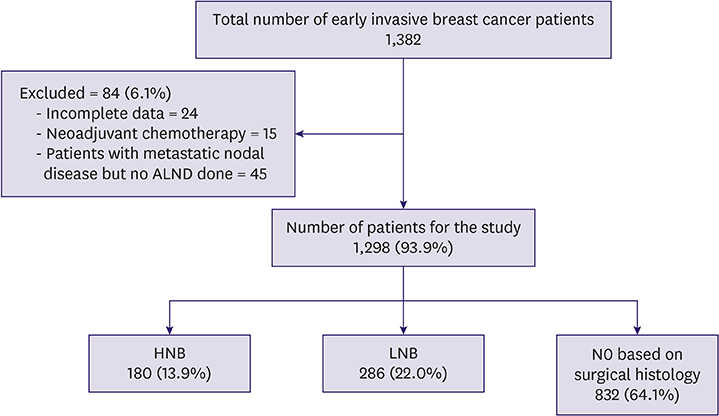
Early invasive breast cancer patients (cT1-2cN0) were retrospectively reviewed. We excluded patients with neoadjuvant chemotherapy and incomplete data. The patients were divided into the following groups based on surgical histology: no positive (N0), LNB, and HNB, defined as 0, 1-2, and ≥ 3 metastatic lymph nodes (LNs), respectively. Of the patients with metastatic nodal disease, only those with ALND were included in the analysis. Clinical, radiological, and histological parameters were evaluated using logistic regression analysis as predictors of HNB versus LNB and N0 combined.
RESULTS
Of the 1,298 included patients, 832 (64.1%), 286 (22.0%), and 180 (13.9%) had N0, LNB, and HNB, respectively. Univariate logistic regression analysis revealed that sonographic features of breast tumor size (p < 0.0001), number of abnormal LNs (p < 0.0001), cortical thickness (p = 0.0002), effacement of the fatty hilum (p < 0.0001), and needle biopsy being performed (p < 0.0001) were indicators of HNB. Breast tumor grade (p = 0.0001) and human epidermal growth factor receptor 2 status (p = 0.0262) were also statistically significant. Among these significant features, multivariable stepwise logistic regression showed that the number of abnormal LNs is the sole independent predictor of HNB (p < 0.0001, area under the curve = 0.774). The positive predictive value of HNB in patients with ≥ 4 abnormal LNs was 92.9%.
CONCLUSION
The detection of ≥ 4 abnormal LNs on ultrasound can help to identify HNB patients who require upfront ALND and thus avoid SLNB.
MeSH Terms
Figure
Reference
-
1. Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (alliance) randomized clinical trial. JAMA. 2017; 318:918–926.
Article2. Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011; 305:569–575.
Article3. Bailey A, Layne G, Shahan C, Zhang J, Wen S, Radis S, et al. Comparison between ultrasound and pathologic status of axillary lymph nodes in clinically node-negative breast cancer patients. Am Surg. 2015; 81:865–869.
Article4. Pilewskie M, Morrow M. Reply to “implications of abnormal preoperative axillary imaging in the post Z011 era”. Gland Surg. 2016; 5:453–454.
Article5. Synnestvedt M, Borgen E, Russnes HG, Kumar NT, Schlichting E, Giercksky KE, et al. Combined analysis of vascular invasion, grade, HER2 and Ki67 expression identifies early breast cancer patients with questionable benefit of systemic adjuvant therapy. Acta Oncol. 2013; 52:91–101.
Article6. Dengel LT, Van Zee KJ, King TA, Stempel M, Cody HS, El-Tamer M, et al. Axillary dissection can be avoided in the majority of clinically node-negative patients undergoing breast-conserving therapy. Ann Surg Oncol. 2014; 21:22–27.
Article7. Sharifi S, Peterson MK, Baum JK, Raza S, Schnitt SJ. Assessment of pathologic prognostic factors in breast core needle biopsies. Mod Pathol. 1999; 12:941–945.8. Pilewskie M, Mautner SK, Stempel M, Eaton A, Morrow M. Does a positive axillary lymph node needle biopsy result predict the need for an axillary lymph node dissection in clinically node-negative breast cancer patients in the ACOSOG Z0011 era? Ann Surg Oncol. 2016; 23:1123–1128.
Article9. Humphrey KL, Saksena MA, Freer PE, Smith BL, Rafferty EA. To do or not to do: axillary nodal evaluation after ACOSOG Z0011 trial. Radiographics. 2014; 34:1807–1816.
Article10. Boland MR, Prichard RS, Daskalova I, Lowery AJ, Evoy D, Geraghty J, et al. Axillary nodal burden in primary breast cancer patients with positive pre-operative ultrasound guided fine needle aspiration cytology: management in the era of ACOSOG Z011. Eur J Surg Oncol. 2015; 41:559–565.
Article11. Lim GH, Upadhyaya VS, Acosta HA, Lim JM, Allen JC Jr, Leong LC. Preoperative predictors of high and low axillary nodal burden in Z0011 eligible breast cancer patients with a positive lymph node needle biopsy result. Eur J Surg Oncol. 2018; 44:945–950.
Article12. Gentilini O, Veronesi U. Abandoning sentinel lymph node biopsy in early breast cancer? A new trial in progress at the European Institute of Oncology of Milan (SOUND: Sentinel node vs Observation after axillary UltraSouND). Breast. 2012; 21:678–681.
Article13. Morrow M, Van Zee KJ, Patil S, Petruolo O, Mamtani A, Barrio AV, et al. Axillary dissection and nodal irradiation can be avoided for most node-positive Z0011-eligible breast cancers: a prospective validation study of 793 patients. Ann Surg. 2017; 266:457–462.
Article14. Wang L, Yu JM, Wang YS, Zuo WS, Gao Y, Fan J, et al. Preoperative lymphoscintigraphy predicts the successful identification but is not necessary in sentinel lymph nodes biopsy in breast cancer. Ann Surg Oncol. 2007; 14:2215–2220.
Article15. Bézu C, Coutant C, Salengro A, Daraï E, Rouzier R, Uzan S. Anaphylactic response to blue dye during sentinel lymph node biopsy. Surg Oncol. 2011; 20:e55–9.
Article16. Bishop JA, Sun J, Ajkay N, Sanders MA. Decline in frozen section diagnosis for axillary sentinel lymph nodes as a result of the American College of Surgeons Oncology Group Z0011 trial. Arch Pathol Lab Med. 2016; 140:830–835.
Article17. del Riego J, Diaz-Ruiz MJ, Teixidó M, Ribé J, Vilagran M, Canales L, et al. The impact of preoperative axillary ultrasonography in T1 breast tumours. Eur Radiol. 2016; 26:1073–1081.
Article18. Cools-Lartigue J, Sinclair A, Trabulsi N, Meguerditchian A, Mesurolle B, Fuhrer R, et al. Preoperative axillary ultrasound and fine-needle aspiration biopsy in the diagnosis of axillary metastases in patients with breast cancer: predictors of accuracy and future implications. Ann Surg Oncol. 2013; 20:819–827.
Article19. Farshid G, Kollias J, Grantley Gill P. The clinical utility of assessment of the axilla in women with suspicious screen detected breast lesions in the post Z0011 era. Breast Cancer Res Treat. 2015; 151:347–355.
Article20. Olaya W, Wong J, Wong J, Morgan J, Kazanjian K, Lum S. When is a lymph node dissection a lymph node dissection? The number of lymph nodes resected in sentinel and axillary lymph node dissections. Ann Surg Oncol. 2013; 20:627–632.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Number of Removed Lymph Nodes for an Acceptable False Negative Rate in Sentinel Lymph Node Biopsy for Breast Cancer
- Optimized Criteria for Sentinel Lymph Node Biopsy in Patients with Clinically Node Negative Breast Cancer
- Sentinel Lymph Node Biopsy in Breast Cancer: A Clinical Review and Update
- Validation and Controversy of Sentinel Node Biopsy for Breast Cancer
- Effectiveness of Sentinel Node Biopsy in the Prediction of Axillary Nodal Status in 111 Patients with Breast Cancer