Ann Rehabil Med.
2018 Feb;42(1):189-194. 10.5535/arm.2018.42.1.189.
Rare Concurrence of Congenital Muscular Torticollis and a Malignant Tumor in the Same Sternocleidomastoid Muscle
- Affiliations
-
- 1The Center for Torticollis, Department of Physical Medicine and Rehabilitation, Ajou University School of Medicine, Suwon, Korea. syyim@ajou.ac.kr
- 2Department of Otolaryngology, Ajou University School of Medicine, Suwon, Korea.
- 3Department of Pathology, Ajou University School of Medicine, Suwon, Korea.
- 4Department of Pediatrics, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2440986
- DOI: http://doi.org/10.5535/arm.2018.42.1.189
Abstract
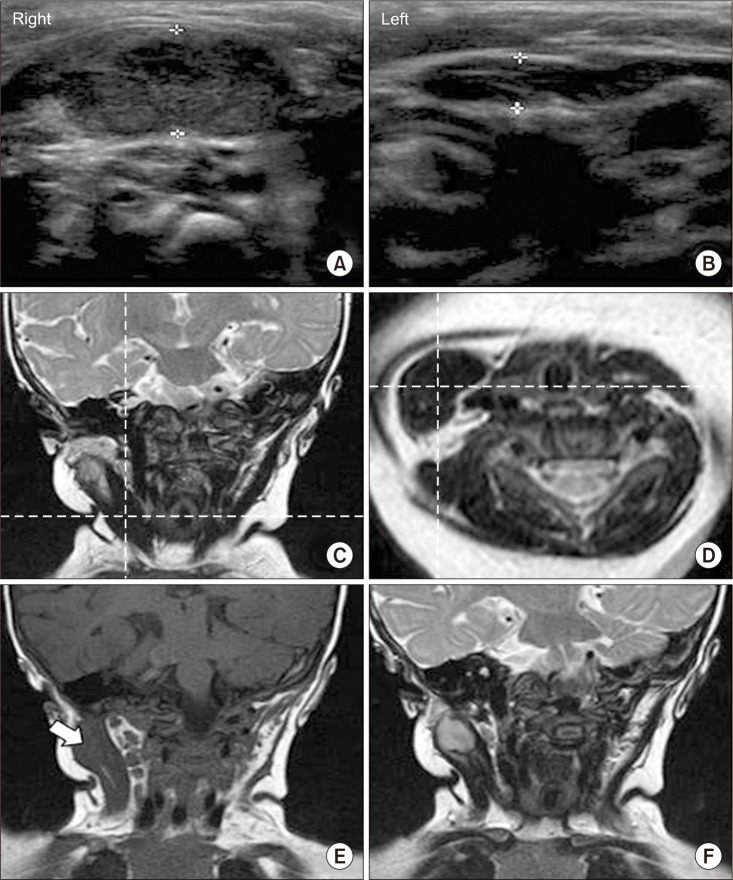
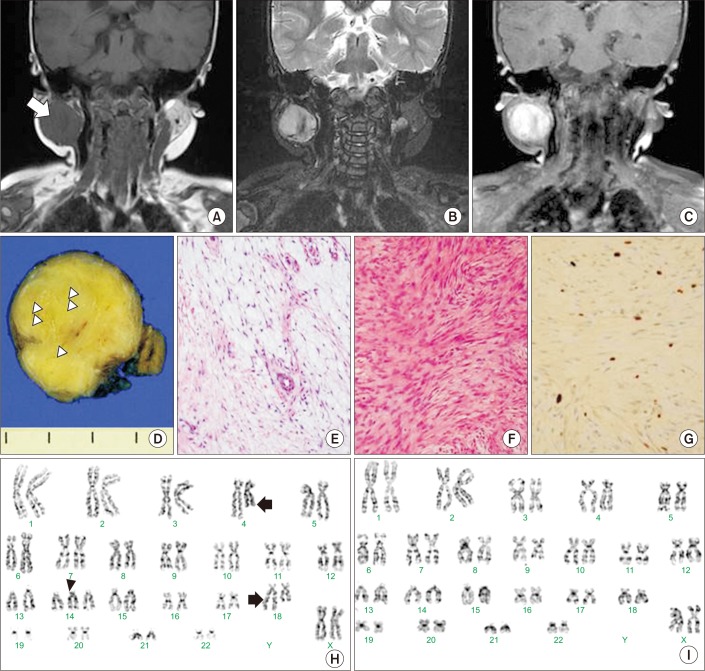
- While congenital muscular torticollis (CMT) can occur along with other conditions, such as clavicle fracture or brachial plexus injury, these conditions exist outside the sternocleidomastoid muscle (SCM). We present a rare case with concurrence of CMT and a malignant tumor inside the same SCM, along with serial clinical and radiological findings of the atypical features of CMT. The malignant tumor was in fact a low-grade fibromyxoid sarcoma. To the best of our knowledge, the current case is the first of a concurrent condition of CMT inside the SCM. This case suggests that concurrent conditions could exist either inside or outside the SCM with CMT. Therefore, a thorough evaluation of SCM is required when subjects with CMT display atypical features, such as the increase of mass or poor response to conservative therapy. In that case, appropriate imaging modalities, such as ultrasonogram or magnetic resonance imaging, are useful for differential diagnosis.
MeSH Terms
Figure
Reference
-
1. Chen MM, Chang HC, Hsieh CF, Yen MF, Chen TH. Predictive model for congenital muscular torticollis: analysis of 1021 infants with sonography. Arch Phys Med Rehabil. 2005; 86:2199–2203. PMID: 16271571.
Article2. Walsh JJ, Morrissy RT. Torticollis and hip dislocation. J Pediatr Orthop. 1998; 18:219–221. PMID: 9531405.
Article3. Hervey-Jumper SL, Justice D, Vanaman MM, Nelson VS, Yang LJ. Torticollis associated with neonatal brachial plexus palsy. Pediatr Neurol. 2011; 45:305–310. PMID: 22000310.
Article4. Mastoraki A, Strigkos T, Tatakis FP, Christophi A, Smyrniotis V. Recurrent low-grade fibromyxoid sarcoma of the neck: report of a case and review of the literature. Indian J Surg Oncol. 2015; 6:296–299. PMID: 27217684.
Article5. Seo HJ, Kim JH. The reliability of the pediatric functional muscle testing in children with developmental delay. J Korean Phys Ther. 2015; 27:183–189.
Article6. Hwang JH, Lee HB, Kim JH, Park MC, Kwack KS, Han JD, et al. Magnetic resonance imaging as a determinant for surgical release of congenital muscular torticollis: correlation with the histopathologic findings. Ann Rehabil Med. 2012; 36:320–327. PMID: 22837966.
Article7. Entel RJ, Carolan FJ. Congenital muscular torticollis: magnetic resonance imaging and ultrasound diagnosis. J Neuroimaging. 1997; 7:128–130. PMID: 9128457.
Article8. Jaber MR, Goldsmith AJ. Sternocleidomastoid tumor of infancy: two cases of an interesting entity. Int J Pediatr Otorhinolaryngol. 1999; 47:269–274. PMID: 10321783.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Sternomastoid Tumor
- Congenital Torticollis with Bilateral Sternocleidomastoid Muscle Contracture
- Solitary Osteochondroma of the Clavicle associated with Congenital Muscular Torticollis: A Case Report
- Ultrasonographic Measurement of the Sternocleidomastoid Muscle in Congenital Muscular Torticollis
- Familial Congenital Muscular Torticollis: A Case Report