Neonatal Med.
2019 Feb;26(1):48-54. 10.5385/nm.2019.26.1.48.
Comparison of Clinical Factors and Neurodevelopmental Outcomes between Early- and Late-Onset Periventricular Leukomalacia in Very Low Birth Weight Infants
- Affiliations
-
- 1Division of Neonatology, Department of Pediatrics, Pusan National University School of Medicine, Yangsan, Korea. byun410@hanmail.net
- KMID: 2440700
- DOI: http://doi.org/10.5385/nm.2019.26.1.48
Abstract
- PURPOSE
To analyze and compare the clinical factors and neurodevelopmental outcomes compare early- and late-onset periventricular leukomalacia (PVL) in very low birth weight infants (VLBWI).
METHODS
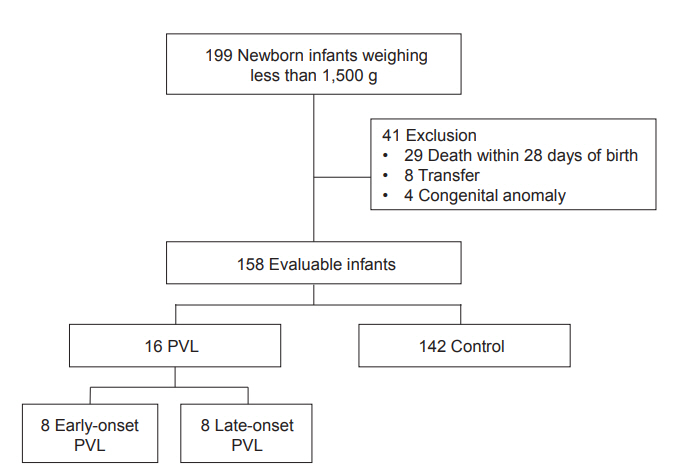
We performed a retrospective study involving 199 newborn infants weighing < 1,500 g admitted to the neonatal intensive care unit between March 2009 and December 2015. VLBWI with PVL were categorized into early- and late-onset PVL groups based on the time of diagnosis based on 28 days of age. We analyzed the clinical factors and neurodevelopmental outcomes between the groups.
RESULTS
The incidence rate of PVL was 10.1% (16/158). The Apgar score at 1 minute and the mean duration of tocolytic therapy were associated with the development of PVL. The incidence rate of premature rupture of membranes (PROM) was significantly higher in the early-onset PVL group (P=0.041). No significant differences were observed in neurodevelopmental outcomes between the early- and late-onset PVL groups.
CONCLUSION
Results suggest that a higher incidence of PROM was associated with clinical characteristics in the early-onset PVL group. No significant intergroup differences were observed in neurodevelopmental outcomes; however, the Bayley Scales of Infant Development-III scores were lower in the early-onset PVL group.
Keyword
MeSH Terms
Figure
Reference
-
1. Sung TJ. Recent advances between prenatal inflammatory response and prematurity associated complications. Korean J Perinatol. 2013; 24:127–32.2. Andrews WW, Cliver SP, Biasini F, Peralta-Carcelen AM, Rector R, Alriksson-Schmidt AI, et al. Early preterm birth: association between in utero exposure to acute inflammation and severe neurodevelopmental disability at 6 years of age. Am J Obstet Gynecol. 2008; 198:466. e1-11.3. Kim S, Song IG, Kim KL, Kim YJ, Shin SH, Lee SH, et al. Outpatient follow-up status and neurodevelopmental outcomes of extremely low birth weight infants. J Korean Soc Neonatol. 2012; 19:17–25.4. Tsimis ME, Johnson CT, Raghunathan RS, Northington FJ, Burd I, Graham EM. Risk factors for periventricular white matter injury in very low birthweight neonates. Am J Obstet Gynecol. 2016; 214:380. e1-6.5. Wang LY, Wang YL, Wang ST, Huang CC. Using the Alberta Infant Motor Scale to early identify very low-birth-weight infants with cystic periventricular leukomalacia. Brain Dev. 2013; 35:32–7.6. Al Tawil KI, El Mahdy HS, Al Rifai MT, Tamim HM, Ahmed IA, Al Saif SA. Risk factors for isolated periventricular leukomalacia. Pediatr Neurol. 2012; 46:149–53.7. Resch B, Neubauer K, Hofer N, Resch E, Maurer U, Haas J, et al. Episodes of hypocarbia and early-onset sepsis are risk factors for cystic periventricular leukomalacia in the preterm infant. Early Hum Dev. 2012; 88:27–31.8. Resch B, Vollaard E, Maurer U, Haas J, Rosegger H, Muller W. Risk factors and determinants of neurodevelopmental outcome in cystic periventricular leucomalacia. Eur J Pediatr. 2000; 159:663–70.9. Chey MJ, Shim GH. Risk factors of cystic periventricular leukomalacia in preterm infants with gestational ages of less than 32 weeks according to gestational age group. Korean J Perinatol. 2016; 27:36–44.10. Oda N, Takeuchi K, Tanaka A, Maruo T. Obstetric risk factors associated with the development of periventricular leukomalacia in preterm infants born to mothers complicated by placenta previa. Fetal Diagn Ther. 2008; 24:345–8.11. Denzler A, Burkhardt T, Natalucci G, Zimmermann R. Latency after preterm prelabor rupture of the membranes: increased risk for periventricular leukomalacia. J Pregnancy. 2014; 2014:874984.12. Gibbs RS, Blanco JD, St Clair PJ, Castaneda YS. Quantitative bacteriology of amniotic fluid from women with clinical intraamniotic infection at term. J Infect Dis. 1982; 145:1–8.13. Lee NY, Cho SJ, Park EA. Influence of antenatal magnesium sulfate exposure on perinatal outcomes in VLBW infants with maternal preeclampsia. Neonatal Med. 2013; 20:28–34.14. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978; 92:529–34.15. Walsh MC, Kliegman RM, Fanaroff AA. Necrotizing enterocolitis: a practitioner's perspective. Pediatr Rev. 1988; 9:219–26.16. Shim JW, Jin HS, Bae CW. Changes in survival rate for very-lowbirth-weight infants in Korea: Comparison with other countries. J Korean Med Sci. 2015; 30 Suppl 1:S25–34.17. Cho JH, Choi SK, Chung SH, Choi YS, Bae CW. Changes in neonatal and perinatal vital statistics during last 5 decades in republic of Korea: compared with OECD nations. Neonatal Med. 2013; 20:402–12.18. Ahn SY, Shim SY, Sung IK. Intraventricular hemorrhage and post hemorrhagic hydrocephalus among very-low-birth-weight infants in Korea. J Korean Med Sci. 2015; 30 Suppl 1:S52–8.19. Perlman JM, Risser R, Broyles RS. Bilateral cystic periventricular leukomalacia in the premature infant: associated risk factors. Pediatrics. 1996; 97(6 Pt 1):822–7.20. Volpe JJ. Neurobiology of periventricular leukomalacia in the premature infant. Pediatr Res. 2001; 50:553–62.21. O'Shea TM, Allred EN, Dammann O, Hirtz D, Kuban KC, Paneth N, et al. The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early Hum Dev. 2009; 85:719–25.22. Thomas W, Speer CP. Chorioamnionitis: important risk factor or innocent bystander for neonatal outcome? Neonatology. 2011; 99:177–87.23. Deguchi K, Mizuguchi M, Takashima S. Immunohistochemical expression of tumor necrosis factor alpha in neonatal leukomalacia. Pediatr Neurol. 1996; 14:13–6.24. Choi EK, Park D, Kim TK, Lee SH, Bae DK, Yang G, et al. Animal models of periventricular leukomalacia. Lab Anim Res. 2011; 27:77–84.25. Lee YS, Yoo DS. Cystic periventricular leukomalacia in the neonate: analysis of sequential sonographic findings and neurologic outcomes. J Korean Radiol Soc. 2003; 49:57–62.26. de Vries LS, Eken P, Dubowitz LM. The spectrum of leukomalacia using cranial ultrasound. Behav Brain Res. 1992; 49:1–6.27. Pierrat V, Duquennoy C, van Haastert IC, Ernst M, Guilley N, de Vries LS. Ultrasound diagnosis and neurodevelopmental outcome of localised and extensive cystic periventricular leucomalacia. Arch Dis Child Fetal Neonatal Ed. 2001; 84:F151–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes of neurodevelopmental outcomes and risk factors of very low birth weight infants below 1,500 g, in the last 10 years
- Neurologic Outcomes of Periventricular Leukomalacia
- A Study on the Prediction of Neurodevelopmental Outcome by Cranial Ultrasound in Preterm and Low Birth Weight Infants
- Neurodevelopmental Outcomes of Very Low Birth Weight Infants
- Neurodevelopmental outcomes of preterm infants