Pediatr Gastroenterol Hepatol Nutr.
2019 Mar;22(2):142-151. 10.5223/pghn.2019.22.2.142.
Identifying Predictive Factors for the Recurrence of Pediatric Intussusception
- Affiliations
-
- 1Department of Pediatrics, Keimyung University School of Medicine, Dongsan Medical Center, Daegu, Korea. bearinspring@hotmail.com
- 2Department of Radiology, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 2440588
- DOI: http://doi.org/10.5223/pghn.2019.22.2.142
Abstract
- PURPOSE
The aim of the study was to identify factors related to the recurrence of intussusception in pediatric patients.
METHODS
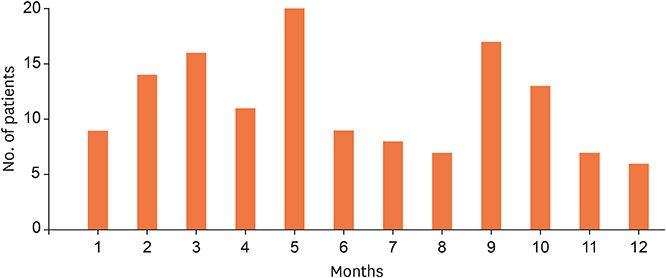
The medical charts of patients diagnosed with intussusception and treated at Dongsan Medical Center, between March 2015 to June 2017, were retrospectively reviewed. Univariate and multivariate analyses were performed.
RESULTS
Among 137 patients, 23 patients (16.8%) had a recurrent intussusception and 8 of these patients (6%) had more than 2 episodes of recurrence. The age at diagnosis was significantly different between the non-recurrence and recurrence group (p=0.026), with age >1 year at the time of diagnosis associated with a greater rate of recurrence (p=0.002). The time interval from symptom onset to the initial reduction ( < 48 vs. ≥48 hours) was significantly longer in the recurrence group (p=0.034) and patients in the recurrence group had higher levels of C-reactive protein (CRP) (p=0.024). Bloody stools and a history of infection were significantly more frequent in the non-recurrence group (p=0.001 and p < 0.001, respectively). On stepwise regression analysis, age >1 year at the time of presentation (odds ratio [OR], 4.79; 95% confidence interval [CI], 1.56-14.06; p=0.016) and no history of infection (OR, 0.18; 95% CI, 0.06-0.58; p=0.004) were retained as predictors of recurrence.
CONCLUSION
Patients with intussusception who are older than 1 year at diagnosis, have an elevated CRP level, a delay of ≥48 hours between symptom onset and the initial reduction, an absence of bloody stools, and no history of infection should be closely monitoring for symptoms and signs of a possible recurrence.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Changes in the Incidence of Intussusception and Infectious Diseases After the COVID-19 Pandemic in Korea
In Hyuk Yoo, Hyun Mi Kang, Dae Chul Jeong
J Korean Med Sci. 2022;37(8):e60. doi: 10.3346/jkms.2022.37.e60.
Reference
-
1. Bruce J, Huh YS, Cooney DR, Karp MP, Allen JE, Jewett TC Jr. Intussusception: evolution of current management. J Pediatr Gastroenterol Nutr. 1987; 6:663–674.2. Saka R, Sasaki T, Matsuda I, Nose S, Onishi M, Fujino T, et al. Chronic ileocolic intussusception due to transmural infiltration of diffuse large B cell lymphoma in a 14-year-old boy: a case report. Springerplus. 2015; 4:366.
Article3. Dias AR, Lopes RI, do Couto RC, Bonafe WW, D'Angelo L, Salvestro ML. Ileal duplication causing recurrent intussusception. J Surg Educ. 2007; 64:51–53.
Article4. Siminas S, Qasem E, Shukla R, Turnock R. Inflammatory fibroid polyp: a rare benign tumor of the alimentary tract in children presenting as intussusception-case report and review of literature. European J Pediatr Surg Rep. 2014; 2:16–19.5. Kim KH, Kang KA, Lim JH, Lee KG, Kwon TJ. Inverted Meckel diverticulum as a lead point of small bowel intussusception: misinterpreting case as a lipoma. Clin Imaging. 2016; 40:840–842.
Article6. Daneman A, Alton DJ, Lobo E, Gravett J, Kim P, Ein SH. Patterns of recurrence of intussusception in children: a 17-year review. Pediatr Radiol. 1998; 28:913–919.
Article7. Lee YW, Yang SI, Kim JM, Kim JY. Clinical features and role of viral isolates from stool samples of intussuception in children. Pediatr Gastroenterol Hepatol Nutr. 2013; 16:162–170.
Article8. Esmaeili-Dooki MR, Moslemi L, Hadipoor A, Osia S, Fatemi SA. Pediatric intussusception in Northern Iran: comparison of recurrent with non-recurrent cases. Iran J Pediatr. 2016; 26:e3898.
Article9. Ksia A, Mosbahi S, Brahim MB, Sahnoun L, Haggui B, Youssef SB, et al. Recurrent intussusception in children and infants. Afr J Paediatr Surg. 2013; 10:299–301.
Article10. Guo WL, Hu ZC, Tan YL, Sheng M, Wang J. Risk factors for recurrent intussusception in children: a retrospective cohort study. BMJ Open. 2017; 7:e018604.
Article11. Kim SH, Kim BC, Choi WJ, Lee JM. A clinical evaluation of the pediatric recurrent intussusception. Ann Surg Treat Res. 1995; 48:548–557.12. Yoo ES, Seo JW, Lee SJ. The risk factors related to recurrent intussusception by ultrasonography. Korean J Pediatr. 1996; 39:1707–1716.13. Orloff MJ. Intussusception in children and adults. Surg Gynecol Obstet. 1956; 102:313–329.14. Carty HM. Paediatric emergencies: non-traumatic abdominal emergencies. Eur Radiol. 2002; 12:2835–2848.
Article15. Buettcher M, Baer G, Bonhoeffer J, Schaad UB, Heininger U. Three-year surveillance of intussusception in children in Switzerland. Pediatrics. 2007; 120:473–480.
Article16. Niramis R, Watanatittan S, Kruatrachue A, Anuntkosol M, Buranakitjaroen V, Rattanasuwan T, et al. Management of recurrent intussusception: nonoperative or operative reduction? J Pediatr Surg. 2010; 45:2175–2180.
Article17. Chen SC, Wang JD, Hsu HY, Leong MM, Tok TS, Chin YY. Epidemiology of childhood intussusception and determinants of recurrence and operation: analysis of national health insurance data between 1998 and 2007 in Taiwan. Pediatr Neonatol. 2010; 51:285–291.
Article18. Park MR, Lim MS, Seo JK, Ko JS, Chang JY, Yang HR, et al. Small bowel intussusception in children: spontaneous resolution vs. surgical intervention. Korean J Pediatr Gastroenterol Nutr. 2010; 13:128–133.
Article19. Wang Z, He QM, Zhang H, Zhong W, Xiao WQ, Lu LW, et al. Intussusception patients older than 1 year tend to have early recurrence after pneumatic enema reduction. Pediatr Surg Int. 2015; 31:855–858.
Article20. Bines JE, Liem NT, Justice FA, Son TN, Kirkwood CD, de Campo M, et al. Risk factors for intussusception in infants in Vietnam and Australia: adenovirus implicated, but not rotavirus. J Pediatr. 2006; 149:452–460.
Article21. Champoux AN, Del Beccaro MA, Nazar-Stewart V. Recurrent intussusception. Risks and features. Arch Pediatr Adolesc Med. 1994; 148:474–478.22. Eklöf O, Reiter S. Recurrent intussusception. Analysis of a series treated with hydrostatic reduction. Acta Radiol Diagn (Stockh). 1978; 19:250–258.23. Simon AK, Hollander GA, McMichael A. Evolution of the immune system in humans from infancy to old age. Proc Biol Sci. 2015; 282:20143085.
Article24. Clarke EJ Jr, Phillips IA, Alexander ER. Adenovirus infection in intussusception in children in Taiwan. JAMA. 1969; 208:1671–1674.
Article25. May AN, Piper SM, Boutlis CS. Yersinia intussusception: case report and review. J Paediatr Child Health. 2014; 50:91–95.
Article26. Minney-Smith CA, Levy A, Hodge M, Jacoby P, Williams SH, Carcione D, et al. Intussusception is associated with the detection of adenovirus C, enterovirus B and rotavirus in a rotavirus vaccinated population. J Clin Virol. 2014; 61:579–584.
Article27. Nylund CM, Denson LA, Noel JM. Bacterial enteritis as a risk factor for childhood intussusception: a retrospective cohort study. J Pediatr. 2010; 156:761–765.
Article28. Williams K, Koyama T, Schulz D, Kaluza GL, Pautler RG, Weisbrodt N, et al. Use of fluoroscopy to study in vivo motility in mouse pups. J Pediatr Gastroenterol Nutr. 2011; 52:679–685.
Article29. Killoran KE, Miller AD, Uray KS, Weisbrodt NW, Pautler RG, Goyert SM, et al. Role of innate immunity and altered intestinal motility in LPS- and MnCl2-induced intestinal intussusception in mice. Am J Physiol Gastrointest Liver Physiol. 2014; 306:G445–53.
Article30. Ravitch MM. The nonoperative treatment of intussusception: hydrostatic pressure reduction by barium enema. Surg Clin North Am. 1956; 36:1495–1500.
Article31. Fallon SC, Lopez ME, Zhang W, Brandt ML, Wesson DE, Lee TC, et al. Risk factors for surgery in pediatric intussusception in the era of pneumatic reduction. J Pediatr Surg. 2013; 48:1032–1036.
Article32. Smith JL, Helwig EB. Malignant lymphomas of the stomach. its diagnosis, distinction and biologic behavior. Am J Pathol. 1958; 34:553.33. Hasegawa T, Ueda S, Tazuke Y, Monta O, Sakurai T, Takahara N, et al. Colonoscopic diagnosis of lymphoid hyperplasia causing recurrent intussusception: report of a case. Surg Today. 1998; 28:301–304.
Article34. Bhisitkul DM, Todd KM, Listernick R. Adenovirus infection and childhood intussusception. Am J Dis Child. 1992; 146:1331–1333.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors related to the outcome of treatment of the intussusception in children
- Clinical Evaluation of Recurrent Intussusception
- The Pathologic Lead Points in Childhood Intussusception
- The Risk Factors related to Recurrent Intussusception by Ultrasonography
- Significance of Follow-Up Ultrasonography 24 Hours Post-Reduction in Detecting Intussusception Recurrence