J Korean Ophthalmol Soc.
2019 Mar;60(3):292-297. 10.3341/jkos.2019.60.3.292.
Two Cases of Uveo-meningeal Syndrome
- Affiliations
-
- 1Department of Ophthalmology, Dankook University College of Medicine, Cheonan, Korea. kseeye@hanmail.net
- KMID: 2440459
- DOI: http://doi.org/10.3341/jkos.2019.60.3.292
Abstract
- PURPOSE
We report two cases of uveo-meningeal syndrome involving the retina, uvea, and optic disc in both eyes after viral meningitis.
CASE SUMMARY
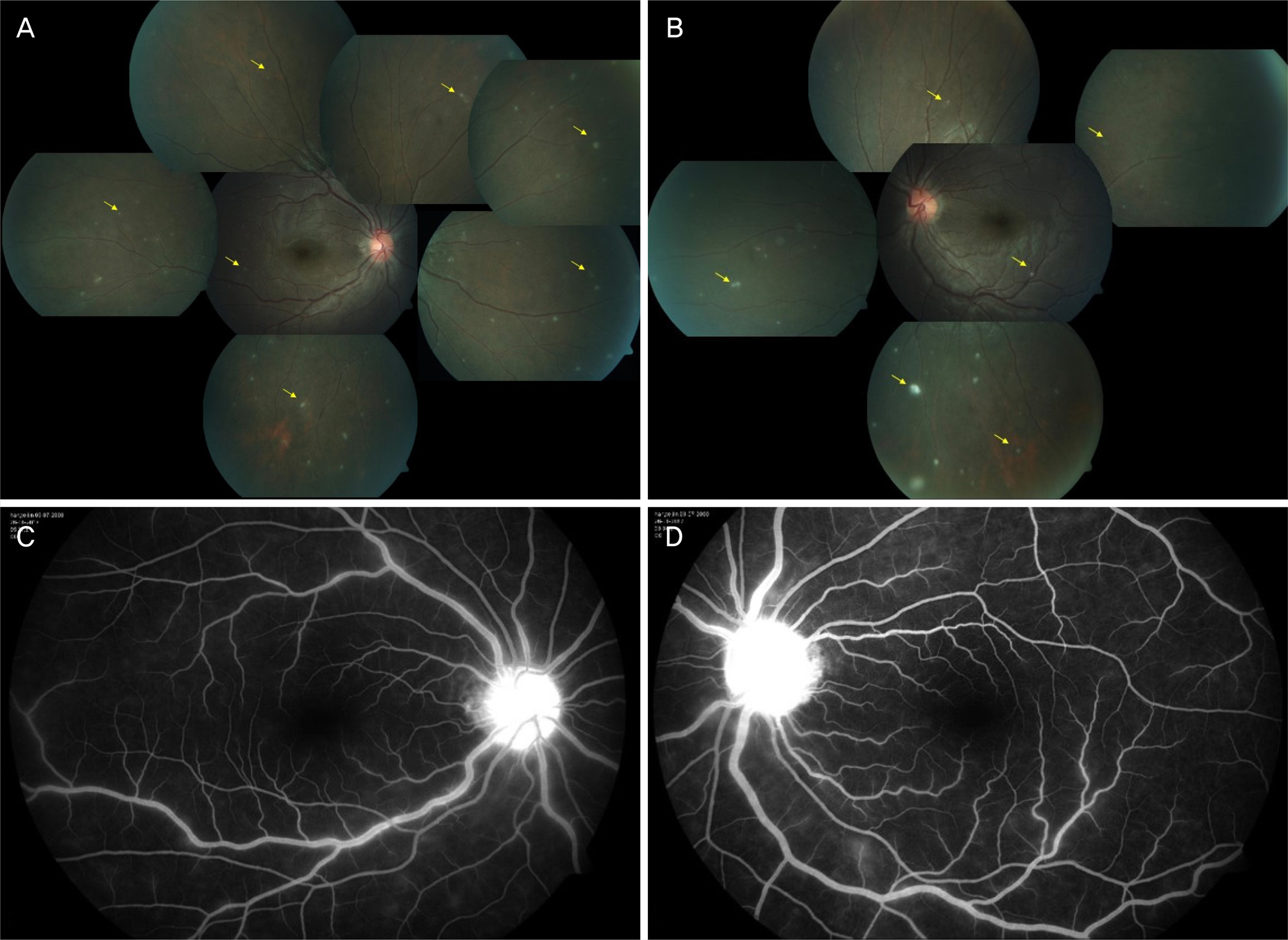
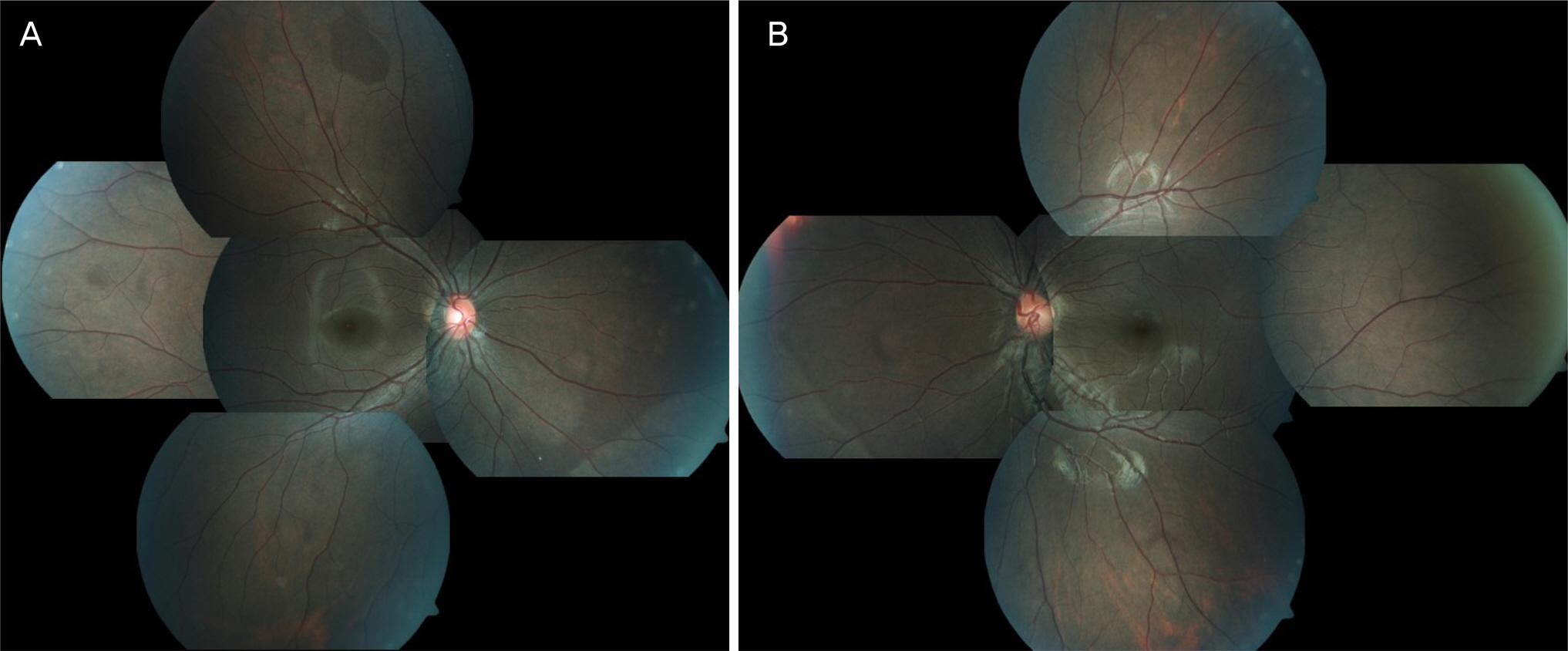
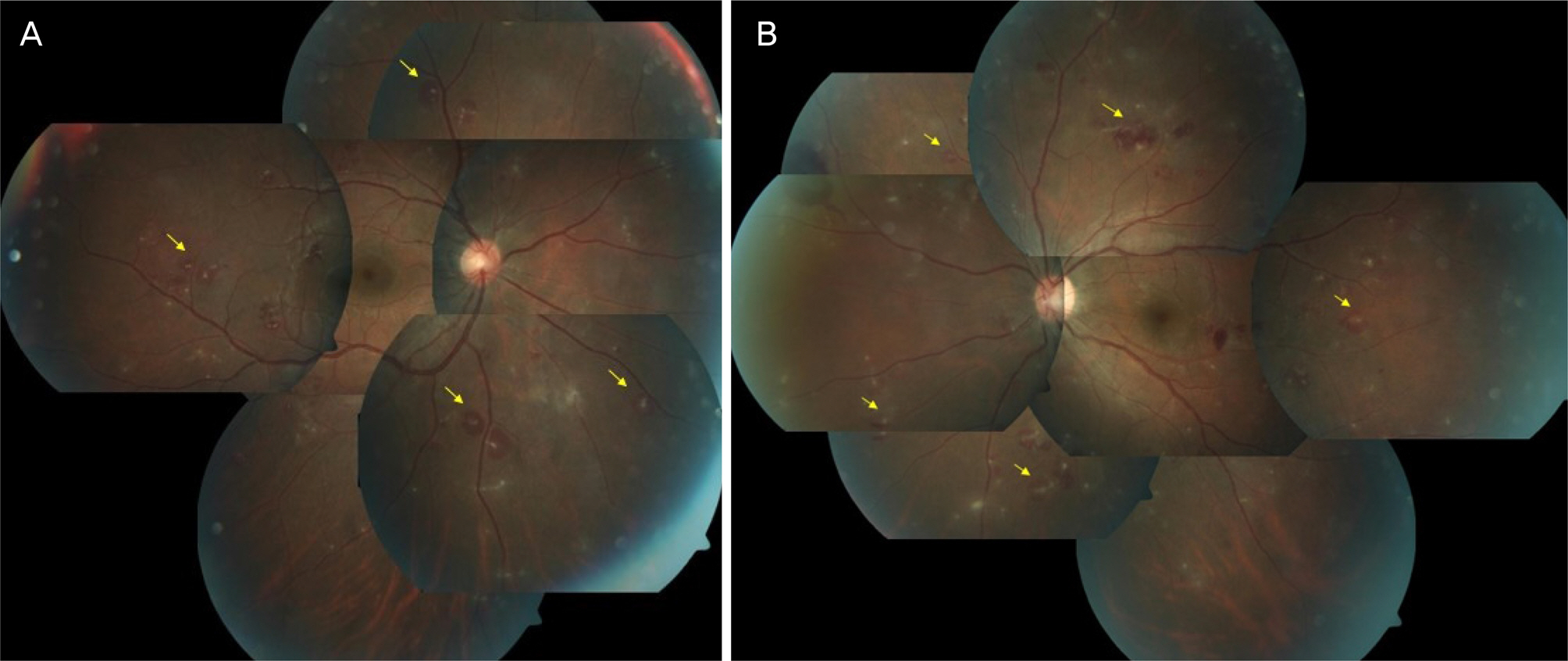
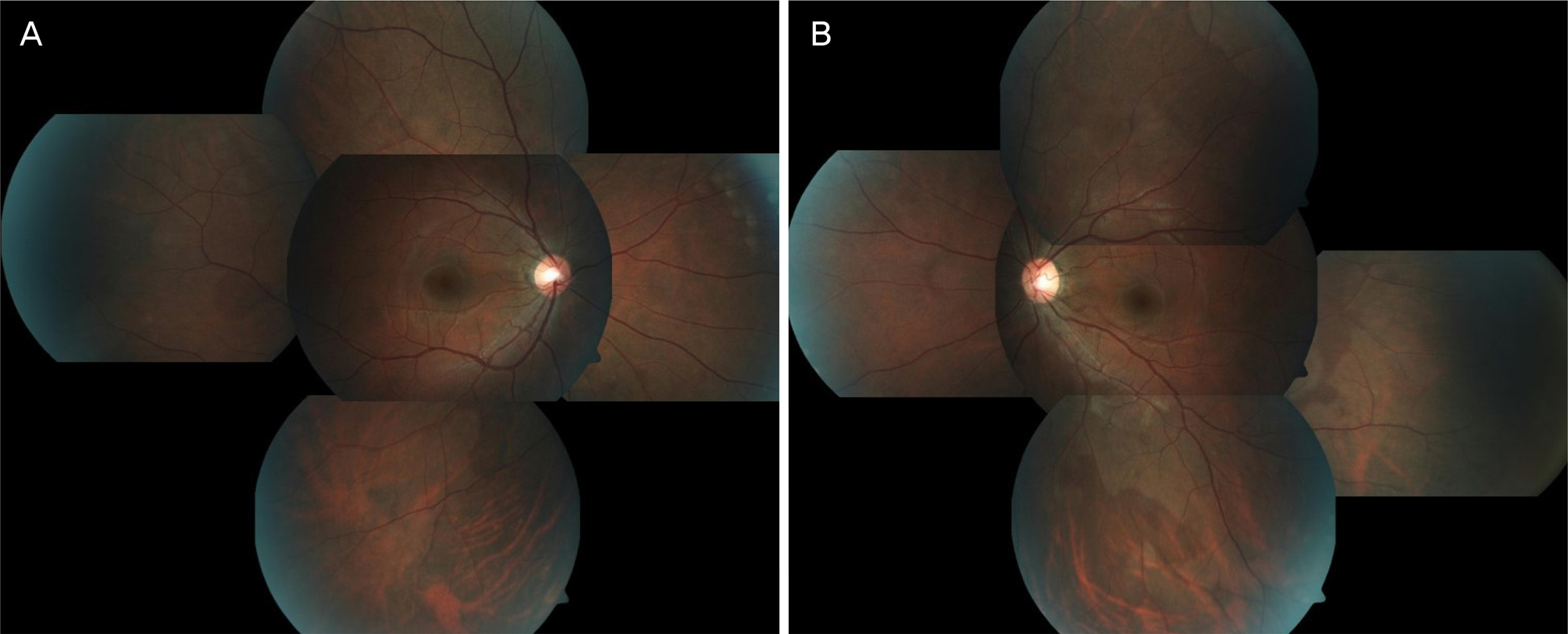
A 16-year-old female was referred to our department with blurred vision in both eyes. She was hospitalized in the pediatric ward with viral meningitis. She showed a norma best-corrected visual acuity (BCVA) and normal intraocular pressure in both eyes, but had severe inflammation in the anterior chamber on slit lamp examination, and optic disc edema and multiple whitish lesions on fundus examination. She was treated with intravenous antibiotic injections and steroid eye drops. After close observation, inflammation in the anterior chamber, optic disc edema, and the multiple whitish lesions in the retina were improved. A 27-year-old male who was treated for viral meningitis at the neurology department was referred to us with blurred vision in both eyes. His BCVAs were 0.7 (right eye) and 0.6 (left eye). The intraocular pressure was normal in both eyes. Slit lamp examination revealed inflammation in the anterior chamber and optic disc edema, and a fundus examination revealed multiple infiltrations. He received treatment for presumed herpes virus infection. After close observation, inflammation in the anterior chamber, optic disc edema, and multiple infiltrations with hemorrhage in the retina were improved.
CONCLUSIONS
Clinicians should consider the possibility of uveo-meningeal syndrome, which can cause inflammation in the uvea,retina, and optic disc simultaneous with viral meningitis accompanying blurred vision.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Brazis PW, Stewart M, Lee AG. The uveo-meningeal syndromes. Neurologist. 2004; 10:171–84.
Article2. Lavezzo MM, Sakata VM, Morita C, et al. Vogt-Koyanagi-Harada disease: review of rare autoimmune disease targeting antigens of melanocytes. Orphanet J Rare Dis. 2016; 11:29.
Article3. Heavner W, Pevny L. Eye development and retinogenesis. Cold spring Harb Perspect Biol. 2012; 4:a008391.
Article4. Decimo I, Fumagalli G, Berton V, et al. Meninges: from protective membrane to stem cell niche. Am J Stem cells. 2012; 1:92–105.5. Allegri P, Risotto R, Herbort CP, Murialdo U. CNS disease and uveitis. J Ophthalmic Vis Res. 2011; 6:284–308.6. Yashar SS, Yashar B, Epstein E, Viani RM. Uveitis associated with Mycoplasma pneumonia meningitis. Acta Ophthalmol Scand. 2001; 79:100–1.7. Otomo K, Kaburaki T, Shigeeda T, et al. Bilateral anterior uveitis in a patient with bacterial meningitis. Int Ophthalmol. 2012; 32:401–3.
Article8. Park WK, Baek JW, Ra H. Two cases of acute retinal necrosis after viral meningitis. J Korean Ophthalmol Soc. 2017; 58:1295–300.
Article9. Smith JR, Rosenbaum JT. Neurological concomitants of uveitis. Br J Ophthalmol. 2004; 88:1498–9.
Article10. Williams DF, Mieler WF. abdominal follow-up of acute placoid multifocal posterior placoid pigment epitheliopathy. Br J Ophthalmol. 1989; 73:985–90.11. Vandercam T, Hintzen RQ, de Boer JH, Van der Lelij A. Herpetic encephalitis is a risk factor for acute retinal necrosis. Neurology. 2008; 71:1268–74.
Article12. Rautenberg P, Hillenkamp J, Granč ič ova L, et al. Virus diagnostics and antiviral therapy in acute retinal necrosis (ARN). Arbuthnot P, editor. Antiviral Drugs. 1st ed.Rijeka: InTech;2012. p. 17–34.
Article13. Gatry DS, Spalton DJ, Tilzey A, Hykin PG. Acute retinal necrosis syndrome. Br J Ophthalmol. 1991; 75:292–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rupture of a Middle Meningeal Artery Pseudoaneurysm in Moyamoya Syndrome Related with Tuberculous Meningitis
- Unusual Course of the Accessory Meningeal Artery
- Primary Spinal Meningeal Melanocytoma
- Spinal Extradural Meningeal Cyst in Klippel-Trenaunay Syndrome
- Meningeal Melanocytoma Associated with Ota's Nevus: Report of a case