J Korean Ophthalmol Soc.
2019 Mar;60(3):287-291. 10.3341/jkos.2019.60.3.287.
Surgical Repair of a Full-thickness Macular Hole in Retinitis Pigmentosa: a Case Report
- Affiliations
-
- 1Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. junekim@amc.seoul.kr
- KMID: 2440458
- DOI: http://doi.org/10.3341/jkos.2019.60.3.287
Abstract
- PURPOSE
To report the long-term outcome after surgical repair of a full-thickness macular hole (FTMH) in a patient with retinitis pigmentosa (RP).
CASE SUMMARY
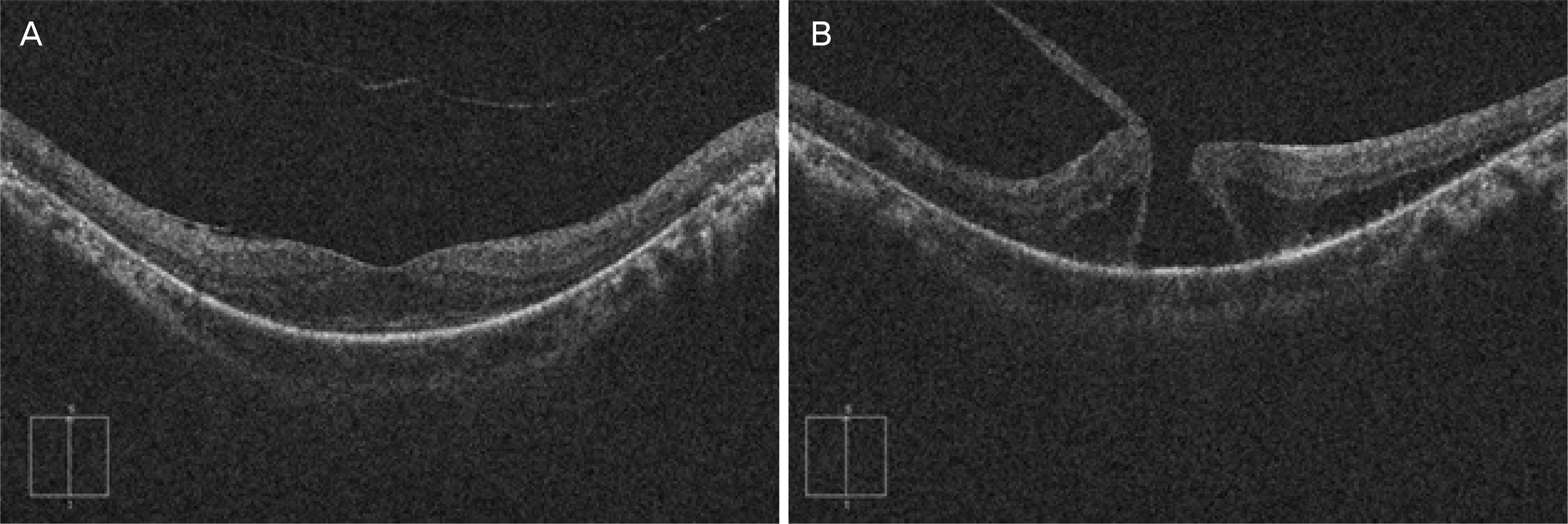
A 55-year-old male who had been diagnosed with retinitis pigmentosa in both eyes 5 years earlier presented with decreased visual acuity in his left eye over the last 6 months. On examination, his Snellen best-corrected visual acuity (BCVA) was 1.0 in the right eye and 0.3 in the left eye. Slit-lamp examination of the anterior segment was remarkable only for posterior chamber intraocular lenses in each eye. Fundus examination demonstrated extensive bony spicule-like pigmentation in the mid-peripheral region in both eyes and a FTMH with approximately one-third disc diameter in the left eye. The optical coherence tomography (OCT) findings confirmed a FTMH with a surrounding cuff of intraretinal fluid and vitreomacular traction in the left eye. The patient underwent 23-gauge pars plana vitrectomy (PPV) with indocyanine green-assisted internal limiting membrane peeling and gas tamponade. One week postoperatively, an anatomically well-sealed macular hole was confirmed by OCT. At the 3-month postoperative follow-up, the BCVA improved to 0.63 and the hole remained closed until his last follow-up (postoperative 6 years).
CONCLUSIONS
Although macular hole is a rare occurrence in RP patients, it should be considered as a cause of significant visual loss in patients with this disorder. Our case suggested that over the long-term, PPV may be tolerable in the management for FTMH in RP.
MeSH Terms
Figure
Reference
-
References
1. Hartong DT, Berson EL, Dryja TP. Retinitis pigmentosa. Lancet. 2006; 368:1795–809.
Article2. You QS, Xu L, Wang YX, et al. Prevalence of retinitis pigmentosa in North China: the Beijing Eye Public Health Care Project. Acta Ophthalmol. 2013; 91:e499–500.
Article3. Hirakawa H, Iijima H, Gohdo T, Tsukahara S. Optical coherence tomography of cystoid macular edema associated with retinitis pigmentosa. Am J Ophthalmol. 1999; 128:185–91.
Article4. Testa F, Rossi S, Colucci R, et al. Macular abnormalities in Italian patients with retinitis pigmentosa. Br J Ophthalmol. 2014; 98:946–50.
Article5. Hagiwara A, Yamamoto S, Ogata K, et al. Macular abnormalities in patients with retinitis pigmentosa: prevalence on OCT examination and outcomes of vitreoretinal surgery. Acta Ophthalmol. 2011; 89:e122–5.
Article6. Giusti C, Forte R, Vingolo EM. Clinical pathogenesis of macular holes in patients affected by retinitis pigmentosa. Eur Rev Med Pharmacol Sci. 2002; 6:45–8.7. Jin ZB, Gan DK, Xu GZ, Nao IN. Macular hole formation in abdominals with retinitis pigmentosa and prognosis of pars plana vitrectomy. Retina. 2008; 28:610–4.8. García-Fernández M, Castro-Navarro J, Bajo-Fuente A. Unilateral recurrent macular hole in a patient with retinitis pigmentosa: a case report. J Med Case Rep. 2013; 7:69.
Article9. Lee JH, Kim TK, Kim SY, et al. Pars plana vitrectomy for vitreous hemorrhage in coats-type retinitis pigmentosa. J Korean Ophthalmol Soc. 2016; 57:677–81.
Article10. Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991; 109:654–9.
Article11. Kadonosono K, Itoh N, Uchio E, et al. Staining of internal limiting membrane in macular hole surgery. Arch Ophthalmol. 2000; 118:1116–8.
Article12. Lee SJ, Jang SY, Moon D, et al. abdominal surgical outcomes after vitrectomy for symptomatic lamellar macular holes. Retina. 2012; 32:1743–8.13. Casparis H, Bovey EH. Surgical treatment of lamellar macular hole associated with epimacular membrane. Retina. 2011; 31:1783–90.
Article14. Gass JD. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988; 106:629–39.
Article15. Raja M, Goldsmith C, Burton BJ. Spontaneous resolution of full-thickness macular hole in retinitis pigmentosa. BMJ Case Rep. 2011; 2011:bcr0320113999.
Article16. Engelbrecht NE, Freeman J, Sternberg P Jr, et al. Retinal pigment epithelial changes after macular hole surgery with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol. 2002; 133:89–94.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Unilateral Retinitis Pigmentosa
- Pars Plana Vitrectomy for Cystoid Macular Edema in a Retinitis Pigmentosa Patient
- A Case of Retinitis Pigmentosa without Pigment
- A Full-Thickness Macular Hole in a Female Adult with Bilateral Retinal Capillary Hemangiomas
- Eccentric Macular Hole Formation After Macular Hole Surgery