J Dent Anesth Pain Med.
2019 Feb;19(1):29-36. 10.17245/jdapm.2019.19.1.29.
Comparison of three behavior modification techniques for management of anxious children aged 4–8 years
- Affiliations
-
- 1Department of Pediatric and Preventive Dentistry, M.R. Ambedkar Dental College and Hospital, Bengaluru, Karnataka, India. sreerak9@gmail.com
- KMID: 2439033
- DOI: http://doi.org/10.17245/jdapm.2019.19.1.29
Abstract
- BACKGROUND
An inability to cope with threatening dental stimuli, i.e., sight, sound, and sensation of airotor, manifests as anxiety and behavioral management problems. Behavior modification techniques involving pre-exposure to dental equipment will give children a first-hand experience of their use, sounds, and clinical effects. The aim of this study was to compare the techniques of Tell-Show-Play-doh, a smartphone dentist game, and a conventional Tell-Show-Do method in the behavior modification of anxious children in the dental operatory.
METHODS
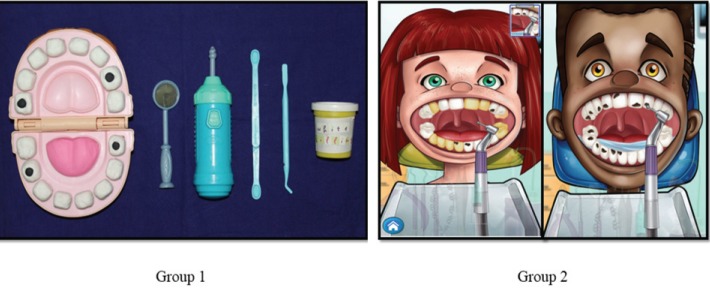
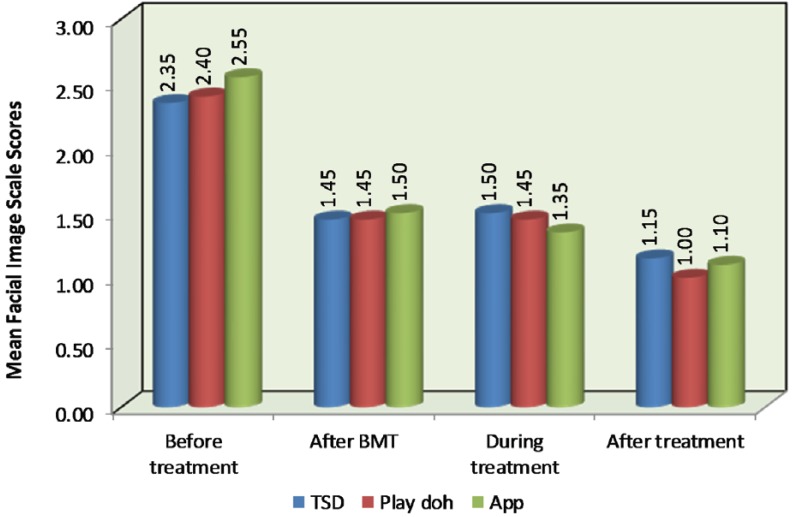
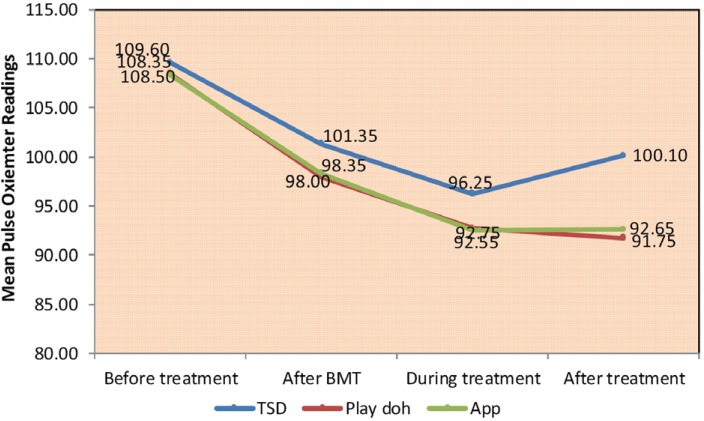
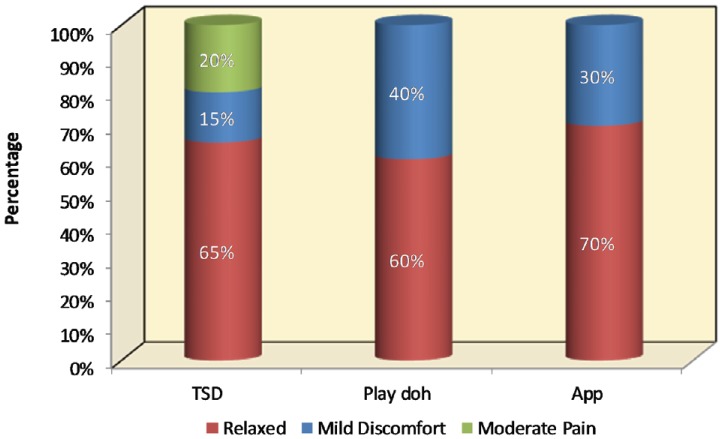
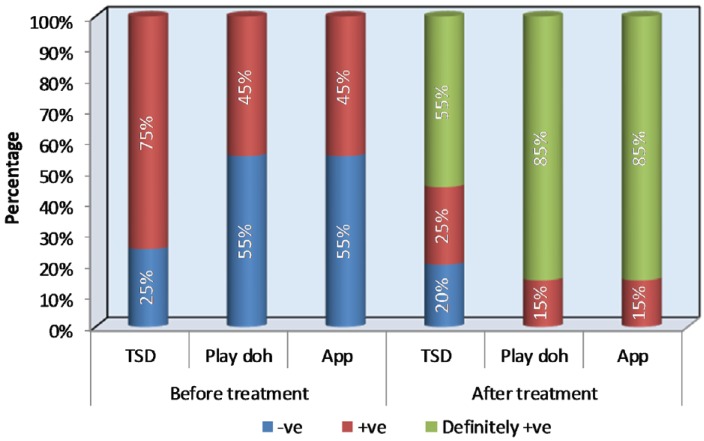
Sixty children in the age group of 4-8 years, with Frankl's behavior rating score of 2 or 3, requiring Class I and II cavity restorations were divided into three groups. The groups were Group 1: Tell-Show-Play-doh; Group 2: smartphone dentist game; and Group 3: Tell-Show-Do technique and each group comprised of 20 children. Pulse rate, Facial Image Scale (FIS), Frankl's behavior rating scale, and FLACC (Face, Leg, Activity, Cry, Consolability) behavior scales were used to quantify anxious behavior. Operator compliance was recorded through a validated questionnaire.
RESULTS
The results showed lower mean pulse rates, lower FIS and FLACC scores, higher percentage of children with Frankl's behavior rating score of 4, and better operator compliance in both the Tell-Show-Play-doh and smartphone dentist game groups than in the conventional Tell-Show-Do group.
CONCLUSION
The Tell-Show-Play-doh and smartphone dentist game techniques are effective tools to reduce dental anxiety in pediatric patients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Effective and safe pediatric sedation
Young-Eun Jang, Jin-Tae Kim
Anesth Pain Med. 2024;19(Suppl 1):S36-S48. doi: 10.17085/apm.24046.
Reference
-
1. Vishwakarma AP, Bondarde PA, Patil SB, Dodamani AS, Vishwakarma PY, Mujawar SA. Effectiveness of two different behavioral modification techniques among 5–7-year-old children: A randomized controlled trial. J Indian Soc Pedod Prev Dent. 2017; 35:143–149. PMID: 28492193.
Article2. Shah HA, Nanjunda Swamy KV, Kulkarni S, Choubey S. Evaluation of dental anxiety and hemodynamic changes (Sympatho-Adrenal Response) during various dental procedures using smartphone applications v/s traditional behaviour management techniques in pediatric patients. Int J Appl Res. 2017; 3:429–433.3. Kawia HM, Mbawalla HS, Kahabuka FK. Application of behavior management techniques for paediatric dental patients by Tanzanian dental practitioners. Open Dent J. 2015; 9:455–461. PMID: 26962374.4. Wright GZ, Stigers JI. Non-pharmacologic management of children's behaviors. In : Dean JA, Avery DR, McDonald RE, editors. Dentistry for the Child and Adolescent. 9th ed. St. Louis: CV Mosby Co;2011. p. 30.5. Townsend JA. Behaviour guidance of the paediatric dental patient. In : Casa Massimo PS, Fields HW, McTigue DJ, Nowak AJ, editors. Paediatric Dentistry-Infancy through Adolescence. 5th ed. Philadelphia: Elsevier Saunders;2013. p. 358.6. Frankl SN, Shire FR, Fogels HR. Should the parent remain with the child in the dental operatory? J Dent Child. 1962; 29:150–162.7. Buchanan H, Niven N. Validation of a Facial Image Scale to assess child dental anxiety. Int J Paediatr Dent. 2002; 12:47–52. PMID: 11853248.
Article8. Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997; 23:293–297. PMID: 9220806.9. Rank RC, Rank MS, Vilela JE, Ogawa WN, Correa MS. Dental anxiety and behavior in young children undergoing different distraction techniques. Pesq Bras Odontoped Clin Integr. 2017; 17:e3651.10. Abanto J, Vidigal EA, Carvalho TS, Bönecker M. Factors for determining dental anxiety in preschool children with severe dental caries. Braz Oral Res. 2017; 31:e13. PMID: 28099579.
Article11. Melwani AM, Srinivasan I, Setty JV, Pamnani SS, Lalitya D. A clinical comparative study between conventional and camouflaged syringes to evaluate behavior and anxiety in 6–11-year-old children during local anesthesia administration-a novel approach. J Dent Anesth Pain Med. 2018; 18:35–40. PMID: 29556557.
Article12. Geetha Priya PR, Asokan S, John JB, Punithavathy R, Karthick K. Comparison of behavioral response to caries removal methods: A randomised controlled cross over trial. J Indian Soc Pedod Prev Dent. 2014; 32:48–52. PMID: 24531602.
Article13. Mitrakul K, Asvanund Y, Arunakul M, Paka-Akekaphat S. Effect of audiovisual eyeglasses during dental treatment in 5-8 year-old children. Eur J Paediatr Dent. 2015; 16:239–245. PMID: 26418930.14. Bagattoni S, D'alessandro G, Sadotti A, Alkhamis N, Piana G. Effects of audiovisual distraction in children with special healthcare needs during dental restorations: a randomized crossover clinical trial. Int J Paediatr Dent. 2018; 28:111–120. PMID: 28399334.
Article15. Riba H. A review of behavior evaluation scales in pediatric dentistry and suggested modification to the Frankl scale. EC Dental Science. 2017; 16:269–275.16. Patil VH, Vaid K, Gokhale NS, Shah P, Mundada M, Hugar SM. Evaluation of effectiveness of dental apps in management of child behaviour: A pilot study. Int J Pedod Rehabil. 2017; 2:14–18.
Article17. Wogelius P, Poulsen S, Toft Sørensen H. Prevalence of dental anxiety and behavior management problems among six to eight years old Danish children. Acta Odontol Scand. 2003; 61:178–183. PMID: 12868693.
Article18. Hoist A, Crossner CG, Hoist A. Direct ratings of acceptance of dental treatment in Swedish children. Community Dent Oral Epidemiol. 1987; 15:258–263. PMID: 3477357.
Article19. Corkey B, Freeman R. Predictors of dental anxiety in six-year old children: findings from a pilot study. ASDC J Dent Child. 1994; 61:267–271. PMID: 7989630.20. Cuthbert MI, Melamed BG. A screening device: children at risk for dental fears and management problems. ASDC J Dent Child. 1982; 49:432–436. PMID: 6960031.21. Adair SM, Waller JL, Schafer TE, Rockman RA. A survey of members of the American Academy of Pediatric Dentistry on their use of behavior management techniques. Pediatr Dent. 2004; 26:159–166. PMID: 15132279.22. Sharath A, Rekka P, Muthu MS, Rathna Prabhu V, Sivakumar N. Children's behavior pattern and behavior management techniques used in a structured postgraduate dental program. J Indian Soc Pedod Prev Dent. 2009; 27:22–26. PMID: 19414970.
Article23. Grewal N. Implementation of behavior management techniques: how well accepted they are today. J Indian Soc Pedod Prev Dent. 2003; 21:70–74. PMID: 14700338.24. Meshki R, Alidadi F, Behboudi A, Oliadarani FK. Effects of pre-treatment exposure to dental practice using a smartphone dental simulation game on children's pain and anxiety: a preliminary double-blind randomized clinical trial. J Dent. 2018; 15:250–258.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Behavior Modification on Body Image, Depression and Body Fat in Obese Korean Elementary School Children
- Effects of Behavior Modification on Obesity Index, Skinfold Thickness, Body Fat, Serum Lipids, Serum Leptin in Obese Elementary School Children
- The Effect of Exercise Combined with Behavior Modification Therapy on the Degree of Obesity, Blood Lipid Level and Self-Esteem in Obese Middle-Aged Women
- The Relationship Between Children's Behavior Problem and Their Food Behaviors
- The Effects of Exercise Therapy and Exercise-Behavior Modification Therapy on Obesity, Blood Lipids, and Self-esteem of the Obese Middle-aged Women