J Korean Orthop Assoc.
2019 Feb;54(1):1-8. 10.4055/jkoa.2019.54.1.1.
Surgical Decision for Elderly Spine Deformity Patient
- Affiliations
-
- 1Department of Orthopedic Surgery, Kyung Hee University College of Medicine, Seoul, Korea.
- 2Department of Orthopedic Surgery, Seoul Chuk Spine Hospital, Seoul, Korea.
- 3Department of Orthopedic Surgery, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. keun118@naver.com
- KMID: 2438951
- DOI: http://doi.org/10.4055/jkoa.2019.54.1.1
Abstract
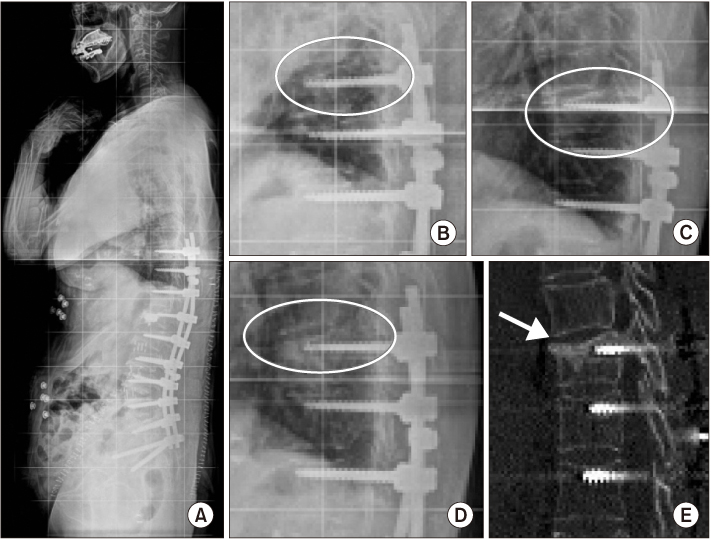
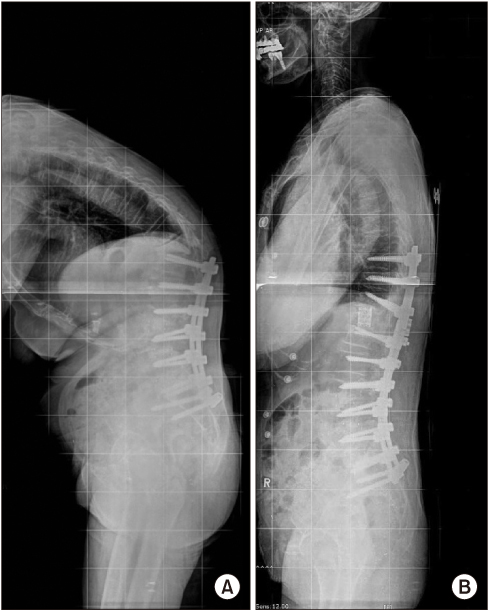
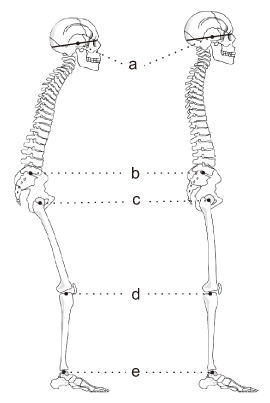
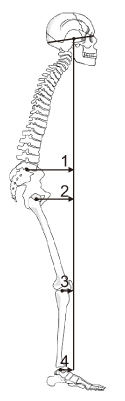
- Globally, the elderly population is increasing rapidly, which means that the number of deformity correction operations for elderly spine deformity patient has increased. On the other hand, for aged patients with deformity correction operation, preoperative considerations to reduce the complications and predict a good clinical outcome are not completely understood. First, medical comorbidity needs to be evaluated preoperatively with the Cumulative Illness Rating Scale for Geriatrics or the Charlson Comorbidity Index scores. Medical comorbidities are associated with the postoperative complication rate. Managing these comorbidities preoperatively decreases the complications after a spine deformity correction operation. Second, bone densitometry need to be checked for osteoporosis. Many surgical techniques have been introduced to prevent the complications associated with posterior instrumentation for osteoporosis patients. The preoperative use of an osteogenesis inducing agent - teriparatide was also reported to reduce the complication rate. Third, total body sagittal alignment need to be considered. Many elderly spine deformity patients accompanied degenerative changes and deformities at their lower extremities. In addition, a compensation mechanism induces the deformed posture of the lower extremities. Recently, some authors introduced a parameter including total body sagittal alignment, which can predict the clinical outcome better than previous parameters limited to the spine or pelvis. As a result, total body sagittal alignment needs to be considered for elderly spine deformity patients after a deformity correction operation. In conclusion, for elderly spine deformity patients, medical comorbidities and osteoporosis need to be evaluated and managed preoperatively to reduce the complication rate. In addition, total body sagittal alignment needs to be considered, which is associated with better clinical outcomes than the previous parameters limited to the spine or pelvis.
Keyword
MeSH Terms
Figure
Reference
-
1. Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005; 30:1082–1085.
Article2. O'Shaughnessy BA, Bridwell KH, Lenke LG, et al. Does a long-fusion “T3-sacrum” portend a worse outcome than a short-fusion “T10-sacrum” in primary surgery for adult scoliosis? Spine (Phila Pa 1976). 2012; 37:884–890.3. Diebo B, Liu S, Lafage V, Schwab F. Osteotomies in the treatment of spinal deformities: indications, classification, and surgical planning. Eur J Orthop Surg Traumatol. 2014; 24:Suppl 1. S11–S20.
Article4. Cassinelli EH, Eubanks J, Vogt M, Furey C, Yoo J, Bohlman HH. Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine (Phila Pa 1976). 2007; 32:230–235.5. Saleh A, Thirukumaran C, Mesfin A, Molinari RW. Complications and readmission after lumbar spine surgery in elderly patients: an analysis of 2,320 patients. Spine J. 2017; 17:1106–1112.
Article6. Wang MY, Widi G, Levi AD. The safety profile of lumbar spinal surgery in elderly patients 85 years and older. Neurosurg Focus. 2015; 39:E3.
Article7. Drazin D, Shirzadi A, Rosner J, et al. Complications and outcomes after spinal deformity surgery in the elderly: review of the existing literature and future directions. Neurosurg Focus. 2011; 31:E3.
Article8. Acosta FL Jr, McClendon J Jr, O'Shaughnessy BA, et al. Morbidity and mortality after spinal deformity surgery in patients 75 years and older: complications and predictive factors. J Neurosurg Spine. 2011; 15:667–674.
Article9. Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976). 2007; 32:2238–2244.10. Ragab AA, Fye MA, Bohlman HH. Surgery of the lumbar spine for spinal stenosis in 118 patients 70 years of age or older. Spine (Phila Pa 1976). 2003; 28:348–353.
Article11. Raffo CS, Lauerman WC. Predicting morbidity and mortality of lumbar spine arthrodesis in patients in their ninth decade. Spine (Phila Pa 1976). 2006; 31:99–103.
Article12. Oldridge NB, Yuan Z, Stoll JE, Rimm AR. Lumbar spine surgery and mortality among medicare beneficiaries, 1986. Am J Public Health. 1994; 84:1292–1298.
Article13. Benz RJ, Garfin SR. Current techniques of decompression of the lumbar spine. Clin Orthop Relat Res. 2001; (384):75–81.
Article14. Smith EB, Hanigan WC. Surgical results and complications in elderly patients with benign lesions of the spinal canal. J Am Geriatr Soc. 1992; 40:867–870.
Article15. Mihailidis HG, Manners S, Churilov L, Quan GMY. Is spinal surgery safe in octogenarians? ANZ J Surg. 2017; 87:605–609.
Article16. DeWald CJ, Stanley T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine (Phila Pa 1976). 2006; 31:S144–S151.17. Puvanesarajah V, Shen FH, Cancienne JM, et al. Risk factors for revision surgery following primary adult spinal deformity surgery in patients 65 years and older. J Neurosurg Spine. 2016; 25:486–493.
Article18. Zindrick MR, Wiltse LL, Widell EH, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986; (203):99–112.
Article19. Wittenberg RH, Shea M, Swartz DE, Lee KS, White AA 3rd, Hayes WC. Importance of bone mineral density in instrumented spine fusions. Spine (Phila Pa 1976). 1991; 16:647–652.
Article20. Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS 3rd, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994; 19:2415–2420.
Article21. Okuyama K, Sato K, Abe E, Inaba H, Shimada Y, Murai H. Stability of transpedicle screwing for the osteoporotic spine. An in vitro study of the mechanical stability. Spine (Phila Pa 1976). 1993; 18:2240–2245.22. Paxinos O, Tsitsopoulos PP, Zindrick MR, et al. Evaluation of pullout strength and failure mechanism of posterior instrumentation in normal and osteopenic thoracic vertebrae. J Neurosurg Spine. 2010; 13:469–476.
Article23. Gilbert SG, Johns PC, Chow DC, Black RC. Relation of vertebral bone screw axial pullout strength to quantitative computed tomographic trabecular bone mineral content. J Spinal Disord. 1993; 6:513–521.
Article24. Hart RA, Prendergast MA. Spine surgery for lumbar degenerative disease in elderly and osteoporotic patients. Instr Course Lect. 2007; 56:257–272.25. Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U. Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J. 2005; 14:551–558.
Article26. Lehman RA Jr, Kuklo TR, Belmont PJ Jr, Andersen RC, Polly DW Jr. Advantage of pedicle screw fixation directed into the apex of the sacral promontory over bicortical fixation: a biomechanical analysis. Spine (Phila Pa 1976). 2002; 27:806–811.27. Brantley AG, Mayfield JK, Koeneman JB, Clark KR. The effects of pedicle screw fit. An in vitro study. Spine (Phila Pa 1976). 1994; 19:1752–1758.28. Bianco RJ, Arnoux PJ, Wagnac E, Mac-Thiong JM, Aubin CÉ. Minimizing pedicle screw pullout risks: a detailed biomechanical analysis of screw design and placement. Clin Spine Surg. 2017; 30:E226–E232.29. Sandén B, Olerud C, Larsson S. Hydroxyapatite coating enhances fixation of loaded pedicle screws: a mechanical in vivo study in sheep. Eur Spine J. 2001; 10:334–339.
Article30. Hu SS. Internal fixation in the osteoporotic spine. Spine (Phila Pa 1976). 1997; 22:43S–48S.
Article31. Hasegawa K, Takahashi HE, Uchiyama S, et al. An experimental study of a combination method using a pedicle screw and laminar hook for the osteoporotic spine. Spine (Phila Pa 1976). 1997; 22:958–962.
Article32. Hasegawa T, Inufusa A, Imai Y, Mikawa Y, Lim TH, An HS. Hydroxyapatite-coating of pedicle screws improves resistance against pull-out force in the osteoporotic canine lumbar spine model: a pilot study. Spine J. 2005; 5:239–243.
Article33. Choma TJ, Rechtine G, McGuire RA, Brodke DS. Treating the aging spine. Instr Course Lect. 2016; 65:269–279.
Article34. Yan YB, Teo EC, Qiu TX, et al. Finite element study on the amount of injection cement during the pedicle screw augmentation. J Spinal Disord Tech. 2013; 26:29–36.
Article35. Paré PE, Chappuis JL, Rampersaud R, et al. Biomechanical evaluation of a novel fenestrated pedicle screw augmented with bone cement in osteoporotic spines. Spine (Phila Pa 1976). 2011; 36:E1210–E1214.
Article36. Pfeiffer FM, Choma TJ, Kueny R. Finite element analysis of Stryker Xia pedicle screw in artificial bone samples with and without supplemental cement augmentation. Comput Methods Biomech Biomed Engin. 2015; 18:1459–1467.
Article37. Kerry G, Ruedinger C, Steiner HH. Cement embolism into the venous system after pedicle screw fixation: case report, literature review, and prevention tips. Orthop Rev (Pavia). 2013; 5:e24.
Article38. Lubansu A, Rynkowski M, Abeloos L, Appelboom G, Dewitte O. Minimally invasive spinal arthrodesis in osteoporotic population using a cannulated and fenestrated augmented screw: technical description and clinical experience. Minim Invasive Surg. 2012; 2012:507826.
Article39. Battula S, Schoenfeld AJ, Sahai V, Vrabec GA, Tank J, Njus GO. The effect of pilot hole size on the insertion torque and pullout strength of self-tapping cortical bone screws in osteoporotic bone. J Trauma. 2008; 64:990–995.
Article40. Carmouche JJ, Molinari RW, Gerlinger T, Devine J, Patience T. Effects of pilot hole preparation technique on pedicle screw fixation in different regions of the osteoporotic thoracic and lumbar spine. J Neurosurg Spine. 2005; 3:364–370.
Article41. Kim H, Chang BS, Lee CK. Considerations for surgical treatment of osteoporotic spinal fracture: surgical indication, approach, fixation, and graft material. J Korean Soc Spine Surg. 2016; 23:41–53.
Article42. Yagi M, Ohne H, Konomi T, et al. Teriparatide improves volumetric bone mineral density and fine bone structure in the UIV+1 vertebra, and reduces bone failure type PJK after surgery for adult spinal deformity. Osteoporos Int. 2016; 27:3495–3502.
Article43. Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009; 34:E599–E606.44. Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 2013; 38:E803–E812.45. Neal CJ, McClendon J, Halpin R, Acosta FL, Koski T, Ondra SL. Predicting ideal spinopelvic balance in adult spinal deformity. J Neurosurg Spine. 2011; 15:82–91.
Article46. Smith JS, Shaffrey CI, Lafage V, et al. Comparison of best versus worst clinical outcomes for adult spinal deformity surgery: a retrospective review of a prospectively collected, multicenter database with 2-year follow-up. J Neurosurg Spine. 2015; 23:349–359.
Article47. Barrey C, Roussouly P, Perrin G, Le Huec JC. Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J. 2011; 20:Suppl 5. 626–633.
Article48. Lafage R, Schwab F, Challier V, et al. Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976). 2016; 41:62–68.49. Jalai CM, Cruz DL, Diebo BG, et al. Full-body analysis of age-adjusted alignment in adult spinal deformity patients and lower-Limb compensation. Spine (Phila Pa 1976). 2017; 42:653–661.
Article50. Kim YC, Lenke LG, Lee SJ, Gum JL, Wilartratsami S, Blanke KM. The cranial sagittal vertical axis (CrSVA) is a better radiographic measure to predict clinical outcomes in adult spinal deformity surgery than the C7 SVA: a monocentric study. Eur Spine J. 2017; 26:2167–2175.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ankylosing Spondylitis: Prevention And Surgical Correction Of Deformity
- Concepts and Techniques to Prevent Cervical Spine Deformity After Spine Surgery: A Narrative Review
- Latest knowledge on a comprehensive understanding of cervical deformity and selection of effective treatment methods using recent classification systems: a narrative review
- Shared Decision Making in Geriatric Care
- Cervical Deformity Arising From Upper Thoracic Malalignment