Korean J Radiol.
2019 Feb;20(2):246-255. 10.3348/kjr.2018.0109.
Structured Reporting versus Free-Text Reporting for Appendiceal Computed Tomography in Adolescents and Young Adults: Preference Survey of 594 Referring Physicians, Surgeons, and Radiologists from 20 Hospitals
- Affiliations
-
- 1Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Department of Radiology, Hallym University Sacred Heart Hospital, Anyang, Korea. drkmj@hallym.or.kr
- 3Program in Biomedical Radiation Sciences, Department of Transdisciplinary Studies, Graduate School of Convergence Science and Technology, Seoul National University, Seoul, Korea.
- 4Department of Radiology, Hanil General Hospital, Seoul, Korea.
- 5Department of Radiology, Daejin Medical Center, Bundang Jesaeng General Hospital, Seongnam, Korea.
- 6Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2438255
- DOI: http://doi.org/10.3348/kjr.2018.0109
Abstract
OBJECTIVE
To survey care providers' preference between structured reporting (SR) and free-text reporting (FTR) for appendiceal computed tomography (CT) in adolescents and young adults.
MATERIALS AND METHODS
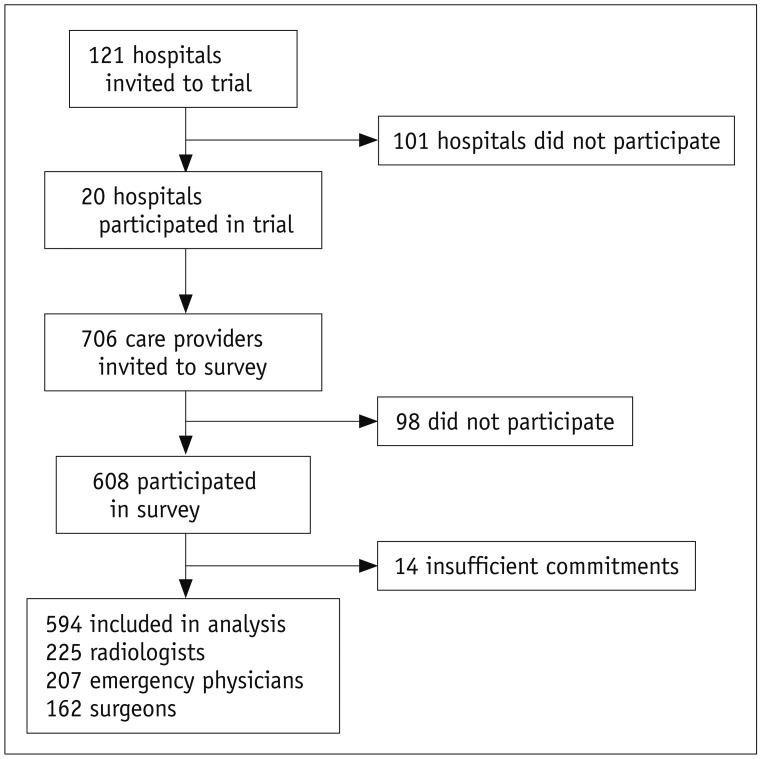
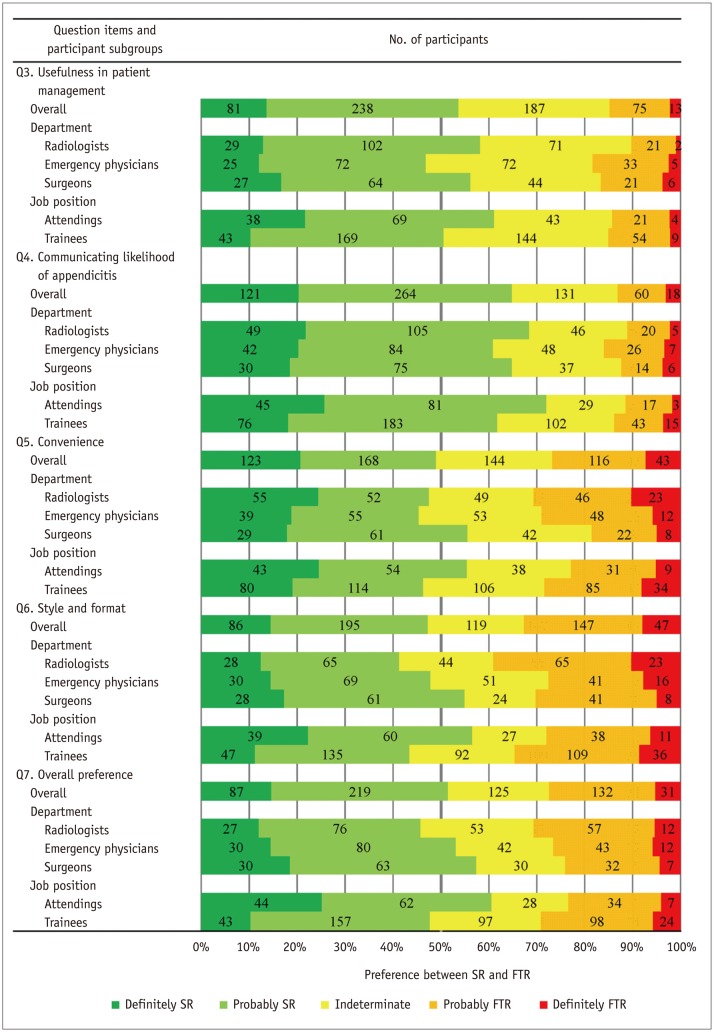
An ethical committee approved this prospective study. The requirement for participant consent was waived. We distributed the Likert scale-based SR form delivering the likelihood of appendicitis across 20 hospitals through a large clinical trial. In the final phase of the trial, we invited 706 potential care providers to participate in an online survey. The survey questions included usefulness in patient management, communicating the likelihood of appendicitis, convenience, style and format, and overall preference. Logistic regression analysis was performed for the overall preference. Three months after the completion of the trial, we checked if the use of the SR was sustained.
RESULTS
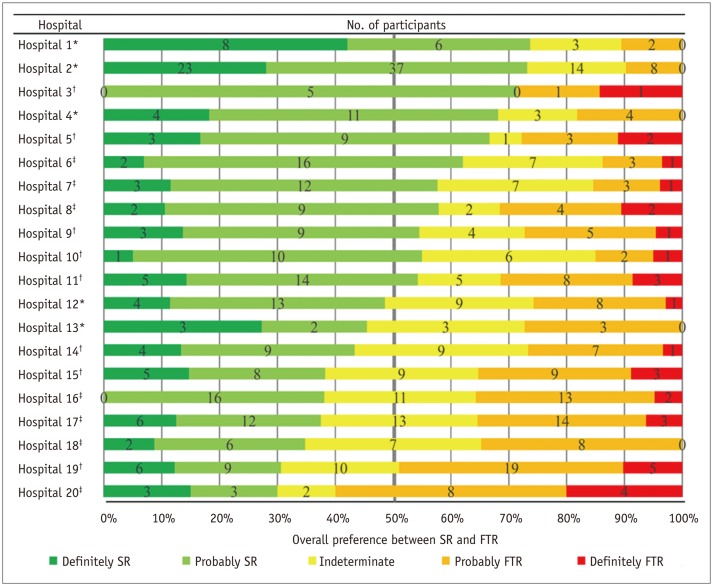
Responses were analyzed from 594 participants (175 attendings and 419 trainees; 225 radiologists, 207 emergency physicians, and 162 surgeons). For each question, 47.3-64.8% of the participants preferred SR, 13.1-32.7% preferred FTR, and the remaining had no preference. The overall preference varied considerably across the hospitals, but slightly across the departments or job positions. The overall preference for SR over FTR was significantly associated with attendings, SR experience for appendiceal CT, hospitals with small appendectomy volume, and hospitals enrolling more patients in the trial. Five hospitals continued using the SR in usual care after the trial.
CONCLUSION
Overall, the care providers preferred SR to FTR. Further investigation into the sustained use of the SR is needed.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Using 2-mSv Appendiceal CT in Usual Practice for Adolescents and Young Adults: Willingness Survey of 579 Radiologists, Emergency Physicians, and Surgeons from 20 Hospitals
Hyuk Jung Kim, Kyoung Ho Lee, Min-Jeong Kim, Sung Bin Park, Yousun Ko,
Korean J Radiol. 2020;21(1):68-76. doi: 10.3348/kjr.2019.0010.
Reference
-
1. Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015; 386:1278–1287. PMID: 26460662.
Article2. Drake FT, Florence MG, Johnson MG, Jurkovich GJ, Kwon S, Schmidt Z, et al. ; SCOAP Collaborative. Progress in the diagnosis of appendicitis: a report from Washington State's Surgical Care and Outcomes Assessment Program. Ann Surg. 2012; 256:586–594. PMID: 22964731.3. Park JH. LOCAT Group. Diagnostic imaging utilization in cases of acute appendicitis: multi-center experience. J Korean Med Sci. 2014; 29:1308–1316. PMID: 25246752.
Article4. Daly CP, Cohan RH, Francis IR, Caoili EM, Ellis JH, Nan B. Incidence of acute appendicitis in patients with equivocal CT findings. AJR Am J Roentgenol. 2005; 184:1813–1820. PMID: 15908536.
Article5. Kim K, Kim YH, Kim SY, Kim S, Lee YJ, Kim KP, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med. 2012; 366:1596–1605. PMID: 22533576.
Article6. Sim JY, Kim HJ, Yeon JW, Suh BS, Kim KH, Ha YR, et al. Added value of ultrasound re-evaluation for patients with equivocal CT findings of acute appendicitis: a preliminary study. Eur Radiol. 2013; 23:1882–1890. PMID: 23392792.
Article7. Ahn S. LOCAT group. LOCAT (low-dose computed tomography for appendicitis trial) comparing clinical outcomes following low- vs standard-dose computed tomography as the first-line imaging test in adolescents and young adults with suspected acute appendicitis: study protocol for a randomized controlled trial. Trials. 2014; 15:28. PMID: 24438500.
Article8. Cooper VF, Goodhartz LA, Nemcek AA Jr, Ryu RK. Radiology resident interpretations of on-call imaging studies: the incidence of major discrepancies. Acad Radiol. 2008; 15:1198–1204. PMID: 18692761.9. Ruchman RB, Jaeger J, Wiggins EF 3rd, Seinfeld S, Thakral V, Bolla S, et al. Preliminary radiology resident interpretations versus final attending radiologist interpretations and the impact on patient care in a community hospital. AJR Am J Roentgenol. 2007; 189:523–526. PMID: 17715095.
Article10. Reiner BI, Knight N, Siegel EL. Radiology reporting, past, present, and future: the radiologist's perspective. J Am Coll Radiol. 2007; 4:313–319. PMID: 17467614.
Article11. Larson DB, Towbin AJ, Pryor RM, Donnelly LF. Improving consistency in radiology reporting through the use of department-wide standardized structured reporting. Radiology. 2013; 267:240–250. PMID: 23329657.
Article12. KSAR Study Group for Rectal Cancer. Essential items for structured reporting of rectal cancer MRI: 2016 Consensus Recommendation from the Korean Society of Abdominal Radiology. Korean J Radiol. 2017; 18:132–151. PMID: 28096724.13. Faggioni L, Coppola F, Ferrari R, Neri E, Regge D. Usage of structured reporting in radiological practice: results from an Italian online survey. Eur Radiol. 2017; 27:1934–1943. PMID: 27572812.
Article14. Powell DK, Silberzweig JE. State of structured reporting in radiology, a survey. Acad Radiol. 2015; 22:226–233. PMID: 25442793.
Article15. D'Orsi CJ. ACR. 2013 ACR BI-RADS Atlas: breast imaging reporting and data system. Reston, VA: American College of Radiology;2014.16. Cury RC, Abbara S, Achenbach S, Agatston A, Berman DS, Budoff MJ, et al. CAD-RADS(TM) coronary artery disease - reporting and data system. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. J Cardiovasc Comput Tomogr. 2016; 10:269–228. PMID: 27318587.
Article17. Dunnick NR, Langlotz CP. The radiology report of the future: a summary of the 2007 intersociety conference. J Am Coll Radiol. 2008; 5:626–629. PMID: 18442766.
Article18. Godwin BD, Drake FT, Simianu VV, Shriki JE, Hippe DS, Dighe M, et al. A novel reporting system to improve accuracy in appendicitis imaging. AJR Am J Roentgenol. 2015; 204:1212–1219. PMID: 26001230.
Article19. Simianu VV, Shamitoff A, Hippe DS, Godwin BD, Shriki JE, Drake FT, et al. The reliability of a standardized reporting system for the diagnosis of appendicitis. Curr Probl Diagn Radiol. 2017; 46:267–274. PMID: 27743632.
Article20. Athans BS, Depinet HE, Towbin AJ, Zhang Y, Zhang B, Trout AT. Use of clinical data to predict appendicitis in patients with equivocal US findings. Radiology. 2016; 280:557–567. PMID: 26878226.
Article21. Fallon SC, Orth RC, Guillerman RP, Munden MM, Zhang W, Elder SC, et al. Development and validation of an ultrasound scoring system for children with suspected acute appendicitis. Pediatr Radiol. 2015; 45:1945–1952. PMID: 26280638.
Article22. Larson DB, Trout AT, Fierke SR, Towbin AJ. Improvement in diagnostic accuracy of ultrasound of the pediatric appendix through the use of equivocal interpretive categories. AJR Am J Roentgenol. 2015; 204:849–856. PMID: 25794076.
Article23. LOCAT Group. Low-dose CT for the diagnosis of appendicitis in adolescents and young adults (LOCAT): a pragmatic, multicentre, randomised controlled non-inferiority trial. Lancet Gastroenterol Hepatol. 2017; 2:793–804. PMID: 28919126.24. Joo SM, Lee KH, Kim YH, Kim SY, Kim K, Kim KJ, et al. Detection of the normal appendix with low-dose unenhanced CT: use of the sliding slab averaging technique. Radiology. 2009; 251:780–787. PMID: 19336669.
Article25. Kim SY, Lee KH, Kim K, Kim TY, Lee HS, Hwang SS, et al. Acute appendicitis in young adults: low- versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology. 2011; 260:437–445. PMID: 21633052.
Article26. Bosmans JM, Weyler JJ, De Schepper AM, Parizel PM. The radiology report as seen by radiologists and referring clinicians: results of the COVER and ROVER surveys. Radiology. 2011; 259:184–195. PMID: 21224423.
Article27. Panicek DM, Hricak H. How sure are you, doctor? A standardized lexicon to describe the radiologist's level of certainty. AJR Am J Roentgenol. 2016; 207:2–3. PMID: 27065212.
Article28. Hobby JL, Tom BD, Todd C, Bearcroft PW, Dixon AK. Communication of doubt and certainty in radiological reports. Br J Radiol. 2000; 73:999–1001. PMID: 11064655.
Article29. Kong A, Barnett GO, Mosteller F, Youtz C. How medical professionals evaluate expressions of probability. N Engl J Med. 1986; 315:740–744. PMID: 3748081.
Article30. Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H. Improving communication of diagnostic radiology findings through structured reporting. Radiology. 2011; 260:174–181. PMID: 21518775.
Article31. Langlotz CP. Structured radiology reporting: are we there yet? Radiology. 2009; 253:23–25. PMID: 19789252.
Article32. Sistrom CL, Honeyman-Buck J. Free text versus structured format: information transfer efficiency of radiology reports. AJR Am J Roentgenol. 2005; 185:804–812. PMID: 16120938.
Article33. Weiss DL, Langlotz CP. Structured reporting: patient care enhancement or productivity nightmare? Radiology. 2008; 249:739–747. PMID: 19011178.
Article34. Johnson AJ, Chen MY, Swan JS, Applegate KE, Littenberg B. Cohort study of structured reporting compared with conventional dictation. Radiology. 2009; 253:74–80. PMID: 19709993.
Article35. Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997; 50:1129–1136. PMID: 9368521.
Article36. Nielsen JW, Boomer L, Kurtovic K, Lee E, Kupzyk K, Mallory R, et al. Reducing computed tomography scans for appendicitis by introduction of a standardized and validated ultrasonography report template. J Pediatr Surg. 2015; 50:144–148. PMID: 25598112.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiologic Reports: Attitudes, Preferred Type, and Opinion of Referring Physicians
- Using 2-mSv Appendiceal CT in Usual Practice for Adolescents and Young Adults: Willingness Survey of 579 Radiologists, Emergency Physicians, and Surgeons from 20 Hospitals
- Added Value of Coronal Reformations for Duty Radiologists and for Referring Physicians or Surgeons in the CT Diagnosis of Acute Appendicitis
- Automated Reporting System Using Structured Data Entry: Application to Prostate US
- Added Value of Structured Reporting for US of the Pediatric Appendix: Additional CT Examinations and Negative Appendectomy