Korean J Radiol.
2019 Feb;20(2):236-245. 10.3348/kjr.2018.0339.
Identification of Arterial Hyperenhancement in CT and MRI in Patients with Hepatocellular Carcinoma: Value of Unenhanced Images
- Affiliations
-
- 1Department of Radiology, Hanyang University Medical Center, Hanyang University School of Medicine, Seoul, Korea.
- 2Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kaienes.kang@samsung.com
- 3Division of Hepatology, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Statistics and Data Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2438254
- DOI: http://doi.org/10.3348/kjr.2018.0339
Abstract
OBJECTIVE
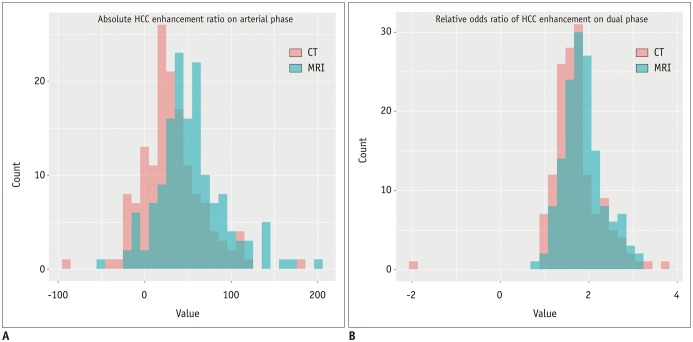
According to the current guidelines, arterial hyperenhancement for diagnosis of hepatocellular carcinoma (HCC) is determined using the arterial phase only. We investigated the optimal definition of arterial hyperenhancement in patients with HCC using computed tomography (CT) and magnetic resonance imaging (MRI).
MATERIALS AND METHODS
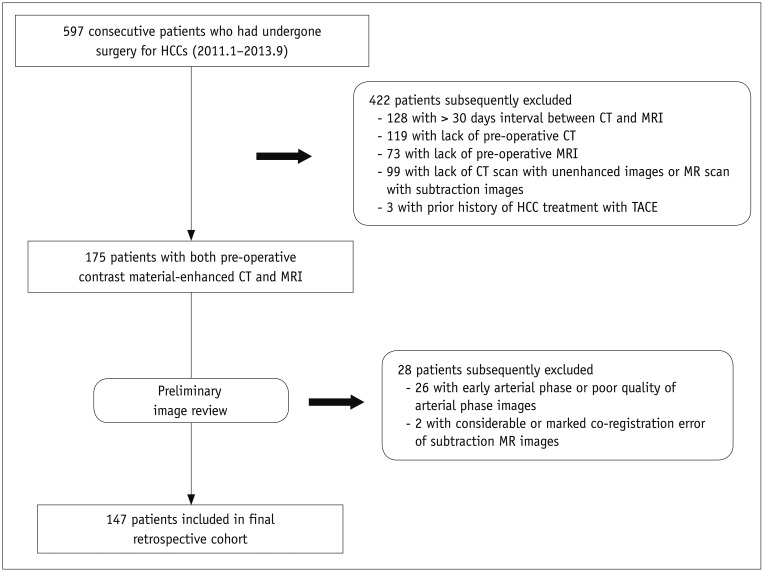
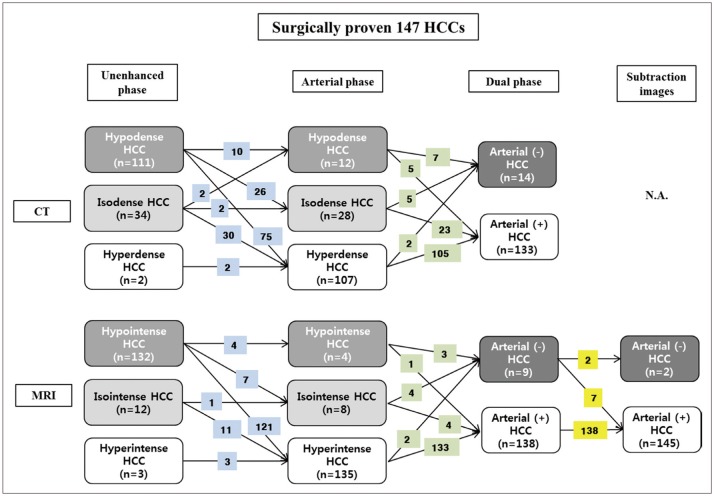
The Institutional Review Board approved this retrospective study. The requirement for informed consent was waived. Between January 2011 and September 2013, 147 consecutive patients with surgically proven HCCs with both pre-operative CT and MRI were included. Identification rates of arterial hyperenhancement on CT and magnetic resonance (MR) images using arterial phase only, dual phase (unenhanced and arterial phases), and also subtraction MR images were assessed qualitatively.
RESULTS
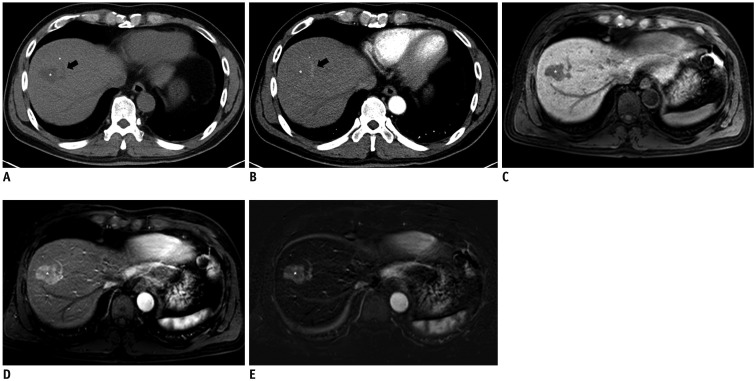
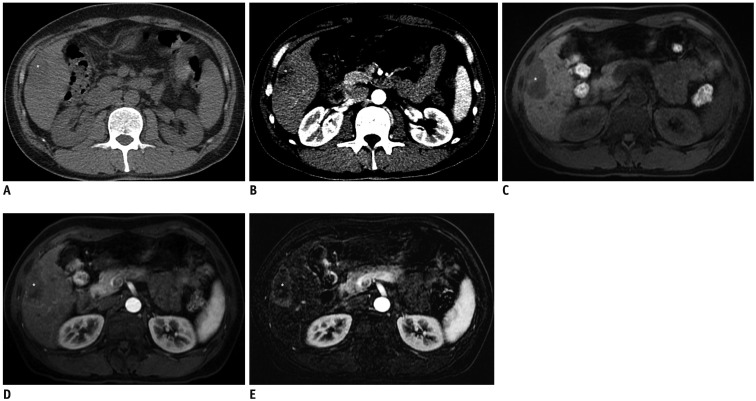
The identification rates for arterial hyperenhancement on CT were significantly different between arterial phase and dual phase (72.8% vs. 90.5%; p < 0.001), whereas the rates were similar on MRI (91.8% vs. 93.9%; p = 0.257). The identification rate of arterial hyperenhancement in MRI increased to 98.6% using subtraction MR images.
CONCLUSION
Visual comparison of arterial and unenhanced phases could be recommended instead of conventional qualitative arterial phase alone assessment to determine arterial hyperenhancement of HCCs, especially when using CT.
Keyword
MeSH Terms
Figure
Reference
-
1. Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011; 53:1020–1022. PMID: 21374666.
Article2. European Association For The Study Of The Liver. European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012; 56:908–943. PMID: 22424438.3. Kokudo N, Hasegawa K, Akahane M, Igaki H, Izumi N, Ichida T, et al. Evidence-based clinical practice guidelines for hepatocellular carcinoma: the Japan Society of Hepatology 2013 update (3rd JSH-HCC Guidelines). Hepatol Res. 2015; 45.
Article4. Korean Liver Cancer Study Group (KLCSG). National Cancer Center, Korea (NCC). 2014 KLCSG-NCC Korea practice guideline for the management of hepatocellular carcinoma. Gut Liver. 2015; 9:267–317. PMID: 25918260.5. Korean Society of Abdominal Radiology. Diagnosis of hepatocellular carcinoma with gadoxetic acid-enhanced MRI: 2016 consensus recommendations of the Korean Society of Abdominal Radiology. Korean J Radiol. 2017; 18:427–443. PMID: 28458595.6. Yoon JH, Park JW, Lee JM. Noninvasive diagnosis of hepatocellular carcinoma: elaboration on Korean Liver Cancer Study Group-National Cancer Center Korea practice guidelines compared with other guidelines and remaining issues. Korean J Radiol. 2016; 17:7–24. PMID: 26798212.
Article7. Park YN. Update on precursor and early lesions of hepatocellular carcinomas. Arch Pathol Lab Med. 2011; 135:704–715. PMID: 21631263.
Article8. Hennedige T, Yang ZJ, Ong CK, Venkatesh SK. Utility of non-contrast-enhanced CT for improved detection of arterial phase hyperenhancement in hepatocellular carcinoma. Abdom Imaging. 2014; 39:1247–1254. PMID: 24943135.
Article9. Yu JS, Kim YH, Rofsky NM. Dynamic subtraction magnetic resonance imaging of cirrhotic liver: assessment of high SIlesions on nonenhanced T1-weighted images. J Comput Assist Tomogr. 2005; 29:51–58. PMID: 15665683.10. An C, Park MS, Kim D, Kim YE, Chung WS, Rhee H, et al. Added value of subtraction imaging in detecting arterial enhancement in small (<3 cm) hepatic nodules on dynamic contrast-enhanced MRI in patients at high risk of hepatocellular carcinoma. Eur Radiol. 2013; 23:924–930. PMID: 23138382.11. Bashir MR, Castelli P, Davenport MS, Larson D, Marin D, Hussain HK, et al. Respiratory motion artifact affecting hepatic arterial phase MR imaging with gadoxetate disodium is more common in patients with a prior episode of arterial phase motion associated with gadoxetate disodium. Radiology. 2015; 274:141–148. PMID: 25162310.
Article12. Davenport MS, Viglianti BL, Al-Hawary MM, Caoili EM, Kaza RK, Liu PS, et al. Comparison of acute transient dyspnea after intravenous administration of gadoxetate disodium and gadobenate dimeglumine: effect on arterial phase image quality. Radiology. 2013; 266:452–461. PMID: 23192781.
Article13. Haradome H, Grazioli L, Tsunoo M, Tinti R, Frittoli B, Gambarini S, et al. Can MR fluoroscopic triggering technique and slow rate injection provide appropriate arterial phase images with reducing artifacts on gadoxetic acid-DTPA (Gd-EOB-DTPA)-enhanced hepatic MR imaging? J Magn Reson Imaging. 2010; 32:334–340. PMID: 20677259.
Article14. Grazioli L, Bondioni MP, Haradome H, Motosugi U, Tinti R, Frittoli B, et al. Hepatocellular adenoma and focal nodular hyperplasia: value of gadoxetic acid-enhanced MR imaging in differential diagnosis. Radiology. 2012; 262:520–529. PMID: 22282184.
Article15. Roux M, Pigneur F, Calderaro J, Baranes L, Chiaradia M, Tselikas L, et al. Differentiation of focal nodular hyperplasia from hepatocellular adenoma: role of the quantitative analysis of gadobenate dimeglumine-enhanced hepatobiliary phase MRI. J Magn Reson Imaging. 2015; 42:1249–1258. PMID: 25851028.
Article16. Haimerl M, Wächtler M, Zeman F, Verloh N, Platzek I, Schreyer AG, et al. Quantitative evaluation of enhancement patterns in focal solid liver lesions with Gd-EOB-DTPA-enhanced MRI. PLoS One. 2014; 9:e100315. PMID: 24950259.
Article17. Taouli B, Johnson RS, Hajdu CH, Oei MT, Merad M, Yee H, et al. Hepatocellular carcinoma: perfusion quantification with dynamic contrast-enhanced MRI. AJR Am J Roentgenol. 2013; 201:795–800. PMID: 24059368.
Article18. Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology. 2014; 273:30–50. PMID: 25247563.
Article19. Coleman WB. Mechanisms of human hepatocarcinogenesis. Curr Mol Med. 2003; 3:573–588. PMID: 14527088.
Article20. Hamer OW, Aguirre DA, Casola G, Lavine JE, Woenckhaus M, Sirlin CB. Fatty liver: imaging patterns and pitfalls. Radiographics. 2006; 26:1637–1653. PMID: 17102041.
Article21. Seçil M, Obuz F, Altay C, Gencel O, Iğci E, Sağol O, et al. The role of dynamic subtraction MRI in detection of hepatocellular carcinoma. Diagn Interv Radiol. 2008; 14:200–204. PMID: 19061165.22. Sugimoto K, Kim SR, Imoto S, Tohyama M, Kim SK, Matsuoka T, et al. Characteristics of hypovascular versus hypervascular well-differentiated hepatocellular carcinoma smaller than 2 cm - Focus on tumor size, markers and imaging detectability. Dig Dis. 2015; 33:721–727. PMID: 26488580.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sonazoid-enhanced ultrasonography: comparison with CT/MRI Liver Imaging Reporting and Data System in patients with suspected hepatocellular carcinoma
- Diagnostic Image Feature and Performance of CT and Gadoxetic Acid Disodium-Enhanced MRI in Distinction of Combined HepatocellularCholangiocarcinoma from Hepatocellular Carcinoma
- Atypical Manifestation of Primary Hepatocellular Carcinoma and Hepatic Malignancy Mimicking Lesions
- Detection of Acute Intraventricular Hemorrhage: Comparison of FLAIR MR Imaging with Unenhanced CT
- Usefulness of Arterial Subtraction in Applying Liver Imaging Reporting and Data System (LI-RADS) Treatment Response Algorithm to Gadoxetic Acid-Enhanced MRI