Clin Endosc.
2019 Jan;52(1):72-75. 10.5946/ce.2018.058.
A Case of Esophageal Squamous Cell Carcinoma in situ Arising from Esophageal Squamous Papilloma
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. adagio@catholic.ac.kr
- 2Department of Hospital Pathology, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 2438148
- DOI: http://doi.org/10.5946/ce.2018.058
Abstract
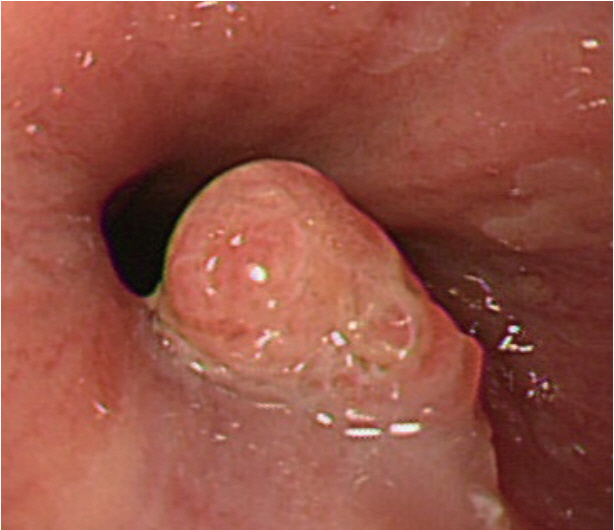
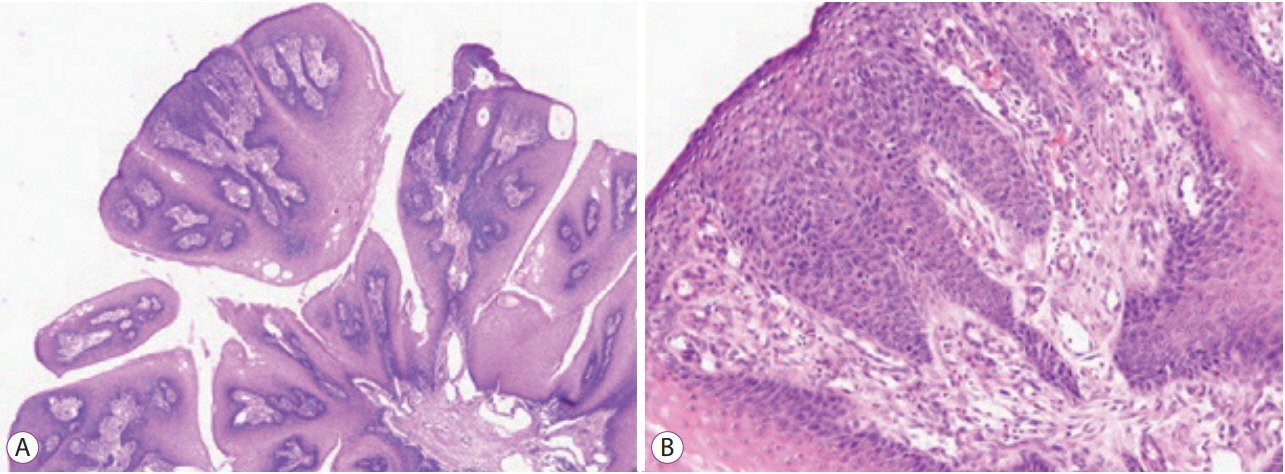
- Squamous papilloma is a common benign tumor of the esophagus. Patients with papilloma are usually asymptomatic, and they are diagnosed incidentally during esophagogastroduodenoscopy. Most papillomas are small and easily removed by forceps biopsy. Recurrence of papilloma after removal is rare. Human papilloma virus infection is supposed to play a role in the development of esophageal papilloma; however, malignant transformation of papilloma is extremely unusual. Here, we report a case of malignant transformation of esophageal squamous papilloma at the gastroesophageal junction into squamous cell carcinoma in situ, which was treated by endoscopic submucosal dissection.
MeSH Terms
Figure
Reference
-
1. Takeshita K, Murata S, Mitsufuji S, et al. Clinicopathological characteristics of esophageal squamous papillomas in Japanese patients--with comparison of findings from Western countries. Acta Histochem Cytochem. 2006; 39:23–30.
Article2. Mosca S, Manes G, Monaco R, Bellomo PF, Bottino V, Balzano A. Squamous papilloma of the esophagus: long-term follow up. J Gastroenterol Hepatol. 2001; 16:857–861.
Article3. d’Huart MC, Chevaux JB, Bressenot AM, et al. Prevalence of esophageal squamous papilloma (ESP) and associated cancer in northeastern France. Endosc Int Open. 2015; 3:E101–E106.
Article4. Wong MW, Bair MJ, Shih SC, et al. Using typical endoscopic features to diagnose esophageal squamous papilloma. World J Gastroenterol. 2016; 22:2349–2356.
Article5. Odze R, Antonioli D, Shocket D, Noble-Topham S, Goldman H, Upton M. Esophageal squamous papillomas. A clinicopathologic study of 38 lesions and analysis for human papillomavirus by the polymerase chain reaction. Am J Surg Pathol. 1993; 17:803–812.6. Pantham G, Ganesan S, Einstadter D, Jin G, Weinberg A, Fass R. Assessment of the incidence of squamous cell papilloma of the esophagus and the presence of high-risk human papilloma virus. Dis Esophagus. 2017; 30:1–5.
Article7. Bohn OL, Navarro L, Saldivar J, Sanchez-Sosa S. Identification of human papillomavirus in esophageal squamous papillomas. World J Gastroenterol. 2008; 14:7107–7111.
Article8. Syrjänen K, Syrjänen S. Detection of human papillomavirus in esophageal papillomas: systematic review and meta-analysis. Apmis. 2013; 121:363–374.
Article9. Inomata S, Aoyagi K, Eguchi K, Sakisaka S. Giant esophageal papilloma. Gastrointest Endosc. 2004; 60:430.
Article10. Reynoso J, Davis RE, Daniels WW, Awad ZT, Gatalica Z, Filipi CJ. Esophageal papillomatosis complicated by squamous cell carcinoma in situ. Dis Esophagus. 2004; 17:345–347.11. Del Genio G, Del Genio F, Schettino P, et al. Esophageal papilloma: flexible endoscopic ablation by radiofrequency. World J Gastrointest Endosc. 2015; 7:290–294.12. Wolfsen HC, Hemminger LL, Geiger XJ, Krishna M, Woodward TA. Photodynamic therapy and endoscopic metal stent placement for esophageal papillomatosis associated with squamous cell carcinoma. Dis Esophagus. 2004; 17:187–190.
Article13. Kim E, Byrne MF, Donnellan F. Endoscopic mucosal resection of esophageal squamous papillomatosis. Can J Gastroenterol. 2012; 26:780–781.
Article14. Park JS, Youn YH, Park JJ, Kim JH, Park H. Clinical outcomes of endoscopic submucosal dissection for superficial esophageal squamous neoplasms. Clin Endosc. 2016; 49:168–175.
Article15. Attila T, Fu A, Gopinath N, Streutker CJ, Marcon NE. Esophageal papillomatosis complicated by squamous cell carcinoma. Can J Gastroenterol. 2009; 23:415–419.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cutaneous Metastasis of Esophageal Squamous Cell Carcinoma Mimicking Benign Soft Tissue Tumor
- A Case of Esophageal Superficial Squamous Cell Papilloma Complicated by Esophageal Ulcer and Bleeding in a Child
- In situ hybridization study on human papillomavirus DNA expression in benign and malignant squamous lesions of the esophagus
- Correlation between Squamous Papilloma and Human Papillomavirus in Esophagus
- Diagnostic problem of squamous papilloma and oral mucosa malignancy