Cancer Res Treat.
2019 Jan;51(1):240-251. 10.4143/crt.2017.417.
The Comparison of Oncologic Outcomes between Open and Laparoscopic Radical Nephroureterectomy for the Treatment of Upper Tract Urothelial Carcinoma: A Korean Multicenter Collaborative Study
- Affiliations
-
- 1Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. bc2.jung@samsung.com
- 2Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Urology, Center for Prostate Cancer, National Cancer Center, Goyang, Korea.
- 4Department of Urology, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- 5Department of Urology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. kuuro70@snu.ac.kr
- KMID: 2437616
- DOI: http://doi.org/10.4143/crt.2017.417
Abstract
- PURPOSE
We compared oncologic outcomes of patients with upper tract urothelial carcinoma (UTUC) who underwent open nephroureterectomy (ONU) or laparoscopic nephroureterectomy (LNU).
MATERIALS AND METHODS
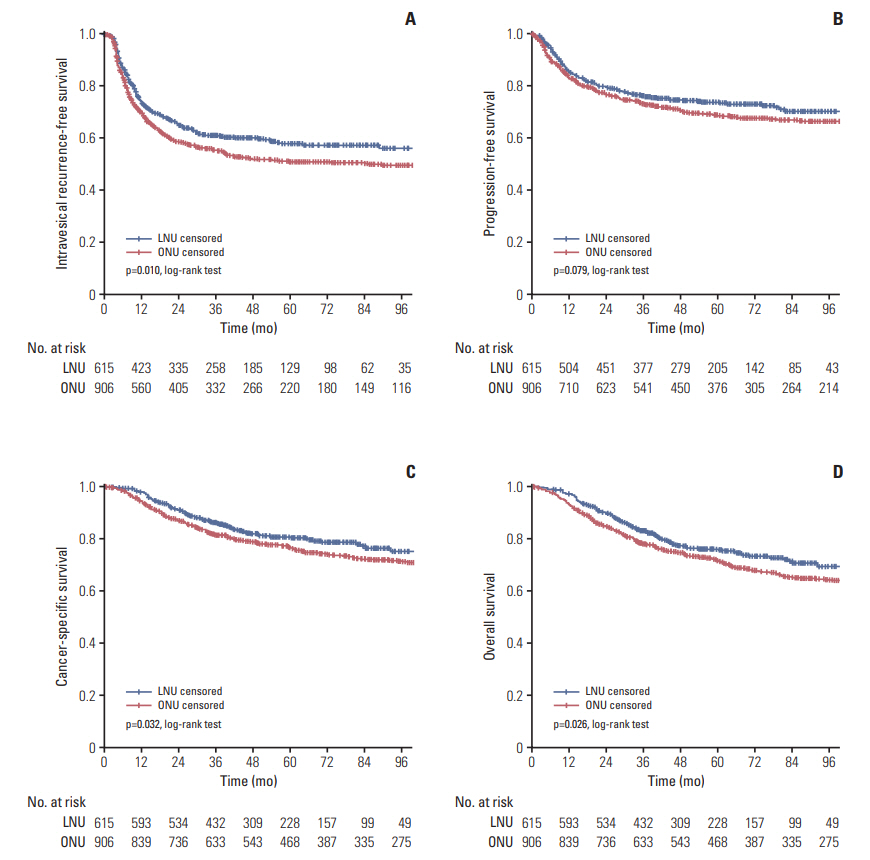
Consecutive cases of ONU and LNU between 2000 and 2012 at five participating institutions were included in this retrospective analysis. Clinical characteristics and pathologic outcomes were compared between the two surgical approaches. The influence of the type of surgical approach on intravesical recurrence-free survival (IVRFS), progression-free survival (PFS), cancer-specific survival (CSS), and overall survival (OS) was analyzed using the Kaplan-Meier method and differences were assessed with the log-rank test. Predictors of IVRFS, PFS, CSS, and OS were also analyzed with a multivariable Cox regression model.
RESULTS
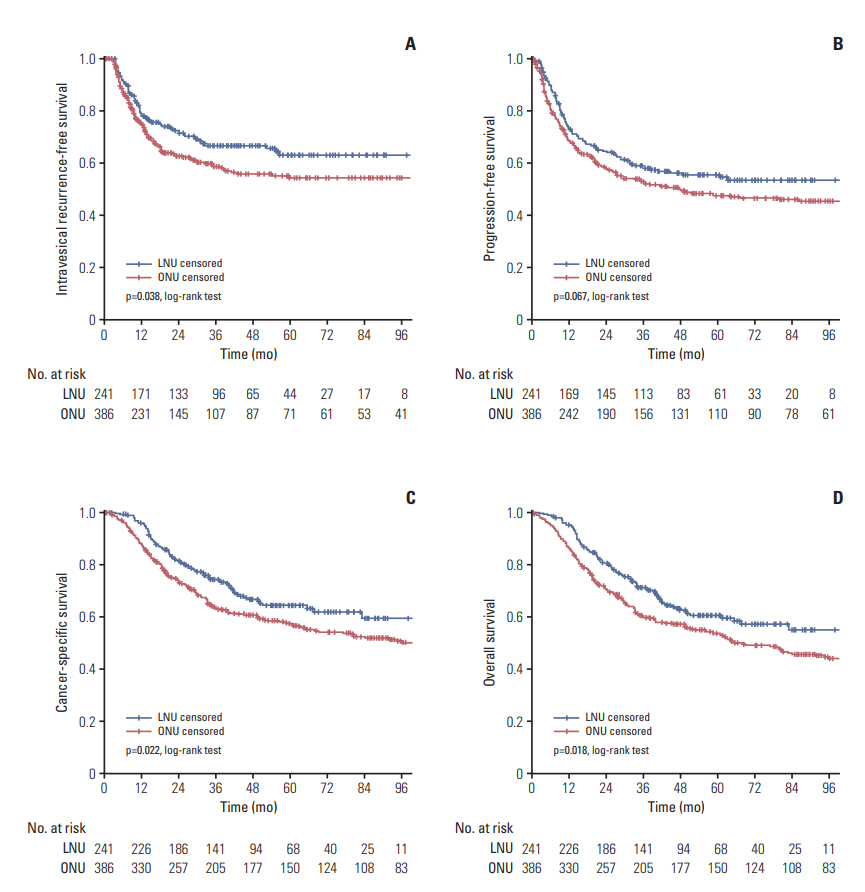
A total of 1,521 patients with UTUC were eligible for the present study (ONU, 906; LNU, 615). The estimated 5-year IVRFS (57.8 vs. 51.0%, p=0.010), CSS (80.4 vs. 76.4%, p=0.032), and OS (75.8 vs. 71.4%, p=0.026) rates were significantly different between the two groups in favor of LNU. Moreover, in patients with locally advanced disease (pT3/pT4), the LNU group showed better 5-year IVRFS (62.9 vs. 54.1%, p=0.038), CSS (64.3 vs. 56.9%, p=0.022), and OS (60.4 vs. 53.1%, p=0.018) rates than the ONU group. Multivariable Cox regression analyses showed that type of surgical approach was independently associated with IVRFS, but was not related to PFS, CSS, and OS.
CONCLUSION
Our findings indicate that LNU provided better oncologic control of IVRFS, CSS, and OS compared with ONU for the management of patients with UTUC.
Figure
Reference
-
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017; 67:7–30.
Article2. Jung KW, Won YJ, Oh CM, Kong HJ, Lee DH, Lee KH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2014. Cancer Res Treat. 2017; 49:292–305.
Article3. Roupret M, Babjuk M, Comperat E, Zigeuner R, Sylvester RJ, Burger M, et al. European Association of Urology guidelines on upper urinary tract urothelial cell carcinoma: 2015 update. Eur Urol. 2015; 68:868–79.4. Tsujihata M, Nonomura N, Tsujimura A, Yoshimura K, Miyagawa Y, Okuyama A. Laparoscopic nephroureterectomy for upper tract transitional cell carcinoma: comparison of laparoscopic and open surgery. Eur Urol. 2006; 49:332–6.
Article5. Simone G, Papalia R, Guaglianone S, Ferriero M, Leonardo C, Forastiere E, et al. Laparoscopic versus open nephroureterectomy: perioperative and oncologic outcomes from a randomised prospective study. Eur Urol. 2009; 56:520–6.
Article6. Capitanio U, Shariat SF, Isbarn H, Weizer A, Remzi M, Roscigno M, et al. Comparison of oncologic outcomes for open and laparoscopic nephroureterectomy: a multi-institutional analysis of 1249 cases. Eur Urol. 2009; 56:1–9.
Article7. Favaretto RL, Shariat SF, Chade DC, Godoy G, Kaag M, Cronin AM, et al. Comparison between laparoscopic and open radical nephroureterectomy in a contemporary group of patients: are recurrence and disease-specific survival associated with surgical technique? Eur Urol. 2010; 58:645–51.
Article8. Walton TJ, Novara G, Matsumoto K, Kassouf W, Fritsche HM, Artibani W, et al. Oncological outcomes after laparoscopic and open radical nephroureterectomy: results from an international cohort. BJU Int. 2011; 108:406–12.
Article9. Ariane MM, Colin P, Ouzzane A, Pignot G, Audouin M, Cornu JN, et al. Assessment of oncologic control obtained after open versus laparoscopic nephroureterectomy for upper urinary tract urothelial carcinomas (UUT-UCs): results from a large French multicenter collaborative study. Ann Surg Oncol. 2012; 19:301–8.
Article10. Liu JY, Dai YB, Zhou FJ, Long Z, Li YH, Xie D, et al. Laparoscopic versus open nephroureterectomy to treat localized and/or locally advanced upper tract urothelial carcinoma: oncological outcomes from a multicenter study. BMC Surg. 2017; 17:8.
Article11. Rieken M, Xylinas E, Kluth L, Trinh QD, Lee RK, Fajkovic H, et al. Diabetes mellitus without metformin intake is associated with worse oncologic outcomes after radical nephroureterectomy for upper tract urothelial carcinoma. Eur J Surg Oncol. 2014; 40:113–20.
Article12. Zhang S, Luo Y, Wang C, Fu SJ, Yang L. Long-term oncologic outcomes of laparoscopic nephroureterectomy versus open nephroureterectomy for upper tract urothelial carcinoma: a systematic review and meta-analysis. PeerJ. 2016; 4:e2063.
Article13. Kim HS, Ku JH, Jeong CW, Kwak C, Kim HH. Laparoscopic radical nephroureterectomy is associated with worse survival outcomes than open radical nephroureterectomy in patients with locally advanced upper tract urothelial carcinoma. World J Urol. 2016; 34:859–69.
Article14. Ni S, Tao W, Chen Q, Liu L, Jiang H, Hu H, et al. Laparoscopic versus open nephroureterectomy for the treatment of upper urinary tract urothelial carcinoma: a systematic review and cumulative analysis of comparative studies. Eur Urol. 2012; 61:1142–53.
Article15. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–4.
Article16. Epstein JI, Amin MB, Reuter VR, Mostofi FK. The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Bladder Consensus Conference Committee. Am J Surg Pathol. 1998; 22:1435–48.17. Kikuchi E, Margulis V, Karakiewicz PI, Roscigno M, Mikami S, Lotan Y, et al. Lymphovascular invasion predicts clinical outcomes in patients with node-negative upper tract urothelial carcinoma. J Clin Oncol. 2009; 27:612–8.
Article18. Sung HH, Jeon HG, Han DH, Jeong BC, Seo SI, Lee HM, et al. Diagnostic ureterorenoscopy is associated with increased intravesical tecurrence following tadical nephroureterectomy in upper tract urothelial carcinoma. PLoS One. 2015; 10:e0139976.19. Clayman RV, Kavoussi LR, Figenshau RS, Chandhoke PS, Albala DM. Laparoscopic nephroureterectomy: initial clinical case report. J Laparoendosc Surg. 1991; 1:343–9.
Article20. Rodriguez JF, Packiam VT, Boysen WR, Johnson SC, Smith ZL, Smith ND, et al. Utilization and outcomes of nephroureterectomy for upper tract urothelial carcinoma by surgical approach. J Endourol. 2017; 31:661–5.
Article21. Fairey AS, Kassouf W, Estey E, Tanguay S, Rendon R, Bell D, et al. Comparison of oncological outcomes for open and laparoscopic radical nephroureterectomy: results from the Canadian Upper Tract Collaboration. BJU Int. 2013; 112:791–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Urothelial Tumors of the Upper Urinary Tract: Multiplicity and Prognostic Variables
- Transperitoneal Laparoscopic Nephroureterectomy for Upper Urinary Tract Transitional Cell Carcinoma: A Comparison with Open Nephroureterectomy
- Identification of Significant Prognostic Tissue Markers Associated with Survival in Upper Urinary Tract Urothelial Carcinoma Patients Treated with Radical Nephroureterectomy: A Retrospective Immunohistochemical Analysis Using Tissue Microarray
- Radical Cystectomy Versus Bladder-Preserving Therapy in Muscle-Invasive Bladder Cancer Patients After Nephroureterectomy for Upper Tract Urothelial Carcinoma: A Multicenter Retrospective Analysis
- Single Early Intravesical Instillation of Epirubicin for Preventing Bladder Recurrence after Nephroureterectomy in Upper Urinary Tract Urothelial Carcinoma