Cancer Res Treat.
2019 Jan;51(1):12-23. 10.4143/crt.2017.273.
The Effect of Hospital Case Volume on Clinical Outcomes in Patients with Nasopharyngeal Carcinoma: A Multi-institutional Retrospective Analysis (KROG-1106)
- Affiliations
-
- 1Proton Therapy Center, Research Institute and Hospital, National Cancer Center, Goyang, Korea. kwancho@ncc.re.kr
- 2Department of Radiation Oncology, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Radiation Oncology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Department of Radiation Oncology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
- 7Department of Radiation Oncology, Pusan National University Hospital, Busan, Korea.
- 8Department of Radiation Oncology, Ajou University School of Medicine, Suwon, Korea.
- 9Department of Radiation Oncology, School of Medicine, Kyungpook National University, Daegu, Korea.
- 10Department of Radiation Oncology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- 11Department of Radiation Oncology, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 12Department of Radiation Oncology, Chungnam National University School of Medicine, Daejeon, Korea.
- 13Department of Radiation Oncology, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
- 14Department of Radiation Oncology, Chung-Ang University Hospital, Seoul, Korea.
- KMID: 2437594
- DOI: http://doi.org/10.4143/crt.2017.273
Abstract
- PURPOSE
The purpose of this study was to investigate the effect of hospital case volume on clinical outcomes in patients with nasopharyngeal carcinoma (NPC).
MATERIALS AND METHODS
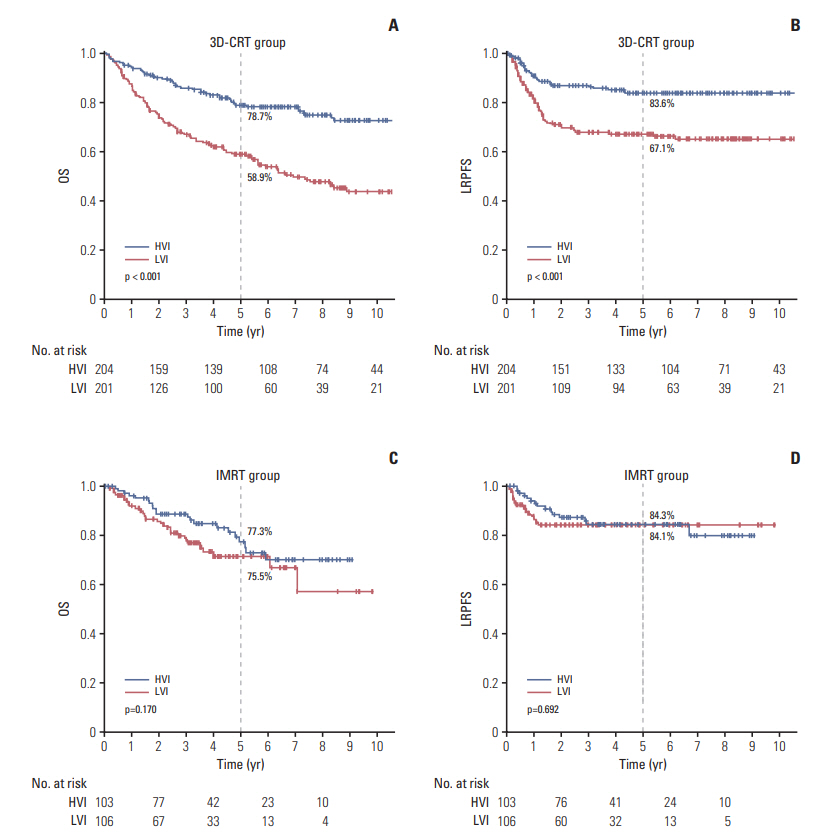
Data on 1,073 patients with cT1-4N0-3M0 NPC were collected from a multi-institutional retrospective database (KROG 11-06). All patients received definitive radiotherapy (RT) either with three-dimensional-conformal RT (3D-CRT) (n=576) or intensity-modulated RT (IMRT) (n=497). The patients were divided into two groups treated at high volume institution (HVI) (n=750) and low volume institution (LVI) (n=323), defined as patient volume ≥ 10 (median, 13; range, 10 to 18) and < 10 patients per year (median, 3; range, 2 to 6), respectively. Endpoints were overall survival (OS) and loco-regional progression-free survival (LRPFS).
RESULTS
At a median follow-up of 56.7 months, the outcomes were significantly better in those treated at HVI than at LVI. For the 614 patients of propensity score-matched cohort, 5-year OS and LRPFS were consistently higher in the HVI group than in the LVI group (OS: 78.4% vs. 62.7%, p < 0.001; LRPFS: 86.2% vs. 65.8%, p < 0.001, respectively). According to RT modality, significant difference in 5-year OS was observed in patients receiving 3D-CRT (78.7% for HVI vs. 58.9% for LVI, p < 0.001) and not in those receiving IMRT (77.3% for HVI vs. 75.5% for LVI, p=0.170).
CONCLUSION
A significant relationship was observed between HVI and LVI for the clinical outcomes of patients with NPC. However, the difference in outcome becomes insignificant in the IMRT era, probably due to the standardization of practice by education.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002; 346:1128–37.
Article2. Gruen RL, Pitt V, Green S, Parkhill A, Campbell D, Jolley D. The effect of provider case volume on cancer mortality: systematic review and meta-analysis. CA Cancer J Clin. 2009; 59:192–211.
Article3. Schrag D, Panageas KS, Riedel E, Cramer LD, Guillem JG, Bach PB, et al. Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection. Ann Surg. 2002; 236:583–92.
Article4. Das IJ, Cheng CW, Chopra KL, Mitra RK, Srivastava SP, Glatstein E. Intensity-modulated radiation therapy dose prescription, recording, and delivery: patterns of variability among institutions and treatment planning systems. J Natl Cancer Inst. 2008; 100:300–7.
Article5. Hong TS, Tome WA, Harari PM. Heterogeneity in head and neck IMRT target design and clinical practice. Radiother Oncol. 2012; 103:92–8.
Article6. Nelms BE, Robinson G, Markham J, Velasco K, Boyd S, Narayan S, et al. Variation in external beam treatment plan quality: an inter-institutional study of planners and planning systems. Pract Radiat Oncol. 2012; 2:296–305.
Article7. Moon SH, Cho KH, Lee CG, Keum KC, Kim YS, Wu HG, et al. IMRT vs. 2D-radiotherapy or 3D-conformal radiotherapy of nasopharyngeal carcinoma : Survival outcome in a Korean multi-institutional retrospective study (KROG 11-06). Strahlenther Onkol. 2016; 192:377–85.8. Sung SY, Kang MK, Kay CS, Keum KC, Kim SH, Kim YS, et al. Patterns of care for patients with nasopharyngeal carcinoma (KROG 11-06) in South Korea. Radiat Oncol J. 2015; 33:188–97.
Article9. Chen YW, Mahal BA, Muralidhar V, Nezolosky M, Beard CJ, Den RB, et al. Association between treatment at a high-volume facility and improved survival for radiation-treated men with high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2016; 94:683–90.10. Koshy M, Malik R, Mahmood U, Husain Z, Sher DJ. Stereotactic body radiotherapy and treatment at a high volume facility is associated with improved survival in patients with inoperable stage I non-small cell lung cancer. Radiother Oncol. 2015; 114:148–54.
Article11. Wang EH, Rutter CE, Corso CD, Decker RH, Wilson LD, Kim AW, et al. Patients selected for definitive concurrent chemoradiation at high-volume facilities achieve improved survival in stage III non-small-cell lung cancer. J Thorac Oncol. 2015; 10:937–43.
Article12. Lee CC, Huang TT, Lee MS, Su YC, Chou P, Hsiao SH, et al. Survival rate in nasopharyngeal carcinoma improved by high caseload volume: a nationwide population-based study in Taiwan. Radiat Oncol. 2011; 6:92.
Article13. Wuthrick EJ, Zhang Q, Machtay M, Rosenthal DI, Nguyen-Tan PF, Fortin A, et al. Institutional clinical trial accrual volume and survival of patients with head and neck cancer. J Clin Oncol. 2015; 33:156–64.
Article14. Boero IJ, Paravati AJ, Xu B, Cohen EE, Mell LK, Le QT, et al. Importance of radiation oncologist experience among patients with head-and-neck cancer treated with intensity-modulated radiation therapy. J Clin Oncol. 2016; 34:684–90.
Article15. Lee N, Xia P, Quivey JM, Sultanem K, Poon I, Akazawa C, et al. Intensity-modulated radiotherapy in the treatment of nasopharyngeal carcinoma: an update of the UCSF experience. Int J Radiat Oncol Biol Phys. 2002; 53:12–22.
Article16. Al-Sarraf M, LeBlanc M, Giri PG, Fu KK, Cooper J, Vuong T, et al. Chemoradiotherapy versus radiotherapy in patients with advanced nasopharyngeal cancer: phase III randomized Intergroup study 0099. J Clin Oncol. 1998; 16:1310–7.
Article17. Langendijk JA, Leemans CR, Buter J, Berkhof J, Slotman BJ. The additional value of chemotherapy to radiotherapy in locally advanced nasopharyngeal carcinoma: a meta-analysis of the published literature. J Clin Oncol. 2004; 22:4604–12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Neoadjuvant Chemotherapy in the Treatment of Nasopharyngeal Carcinoma: A Multi-institutional Retrospective Study (KROG 11-06) Using Propensity Score Matching Analysis
- Impact of institutional case volume on intensive care unit mortality
- A Case of Newly Found Lymphoepithelial Carcinoma in Retropharynx of the Patient Who Had Been in the NED State of Nasopharyngeal Carcinoma: Controversy about the Recurrence of Undiffentiated Nasopharyngeal Carcinoma
- A Case of Multiple Complications after Treatment in Patients with the Second Primary Nasopharyngeal Cancer
- Focal Nasopharyngeal Activity Detected on [18F]FDG PET/CT: Clinical Implications and Comparison of Metabolic Parameters for Prediction of Malignancy