J Pathol Transl Med.
2019 Jan;53(1):57-61. 10.4132/jptm.2018.08.21.
Primary Peripheral Gamma Delta T-Cell Lymphoma of the Central Nervous System: Report of a Case Involving the Intramedullary Spinal Cord and Presenting with Myelopathy
- Affiliations
-
- 1Department of Pathology, Seoul National University Hospital, Seoul, Korea. ykjeon@snu.ac.kr
- 2Department of Radiology, Seoul National University Hospital, Seoul, Korea.
- 3Department of Radiology, Korea University Guro Hospital, Seoul, Korea.
- KMID: 2437579
- DOI: http://doi.org/10.4132/jptm.2018.08.21
Abstract
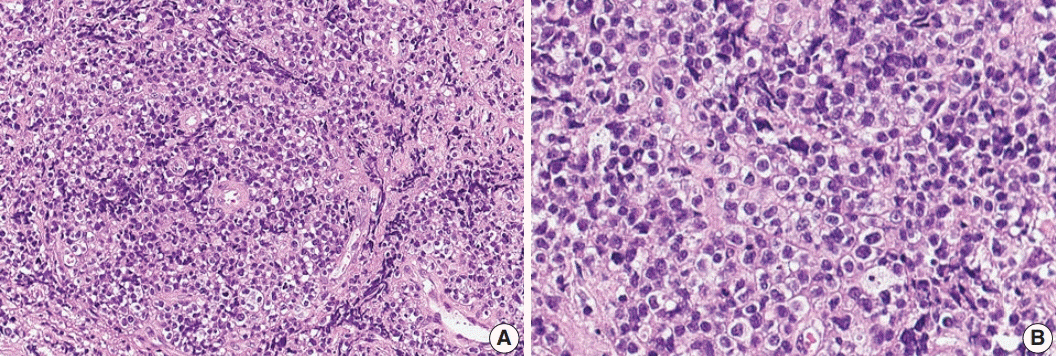
- Primary central nervous system lymphoma of T-cell origin (T-PCNSL) is rare, and its clinicopathological features remain unclear. Peripheral T-cell lymphoma of γδ T-cell origin is an aggressive lymphoma mainly involving extranodal sites. Here, we report a case of γδ T-PCNSL involving the intramedullary spinal cord and presenting with paraplegia. A 75-year-old Korean woman visited the hospital complaining of back pain and lower extremity weakness. Magnetic resonance imaging revealed multifocal enhancing intramedullary nodular lesions in the thoracic and lumbar spinal cord. An enhancing nodular lesion was observed in the periventricular white matter of the lateral ventricle in the brain. There were no other abnormalities in systemic organs or skin. Laminectomy and tumor removal were performed. The tumor consisted of monomorphic, medium-to-large atypical lymphocytes with pale-to-eosinophilic cytoplasm. Immunohistochemically, the tumor cells were CD3(+), TCRβF1(-), TCRγ(+), CD30(-), CD4(-), CD8(-), CD56(+), TIA1(+), granzyme B(+), and CD103(+). Epstein-Barr virus in situ was negative. This case represents a unique T-PCNSL of γδ T-cell origin involving the spinal cord.
Keyword
MeSH Terms
-
Aged
Back Pain
Brain
Central Nervous System*
Cytoplasm
Female
Granzymes
Herpesvirus 4, Human
Humans
Laminectomy
Lateral Ventricles
Lower Extremity
Lymphocytes
Lymphoma
Lymphoma, T-Cell*
Lymphoma, T-Cell, Peripheral
Magnetic Resonance Imaging
Paraplegia
Skin
Spinal Cord Diseases*
Spinal Cord*
T-Lymphocytes*
White Matter
Granzymes
Figure
Reference
-
1. Swerdlow SH, Campo E, Harris NL, et al. WHO classification of tumours of haemotopoietic and lymphoid tissues. Revised 4th ed. Lyon: International Agency for Research on Cancer;2017.2. Shenkier TN, Blay JY, O'Neill BP, et al. Primary CNS lymphoma of T-cell origin: a descriptive analysis from the international primary CNS lymphoma collaborative group. J Clin Oncol. 2005; 23:2233–9.
Article3. Lim T, Kim SJ, Kim K, et al. Primary CNS lymphoma other than DLBCL: a descriptive analysis of clinical features and treatment outcomes. Ann Hematol. 2011; 90:1391–8.
Article4. Menon MP, Nicolae A, Meeker H, et al. Primary CNS T-cell Lymphomas: a clinical, morphologic, immunophenotypic, and molecular analysis. Am J Surg Pathol. 2015; 39:1719–29.5. Nael A, Walavalkar V, Wu W, et al. CD4-positive T-cell primary central nervous system lymphoma in an HIV positive patient. Am J Clin Pathol. 2016; 145:258–65.
Article6. Guzzetta M, Drexler S, Buonocore B, Donovan V. Primary CNS T-cell lymphoma of the spinal cord: case report and literature review. Lab Med. 2015; 46:159–63.
Article7. Flanagan EP, O'Neill BP, Porter AB, Lanzino G, Haberman TM, Keegan BM. Primary intramedullary spinal cord lymphoma. Neurology. 2011; 77:784–91.
Article8. Yang W, Garzon-Muvdi T, Braileanu M, et al. Primary intramedullary spinal cord lymphoma: a population-based study. Neuro Oncol. 2017; 19:414–21.
Article9. Tripodo C, Iannitto E, Florena AM, et al. Gamma-delta T-cell lymphomas. Nat Rev Clin Oncol. 2009; 6:707–17.
Article10. Mooney KL, Choy W, Woodard J, et al. Primary central nervous system gamma delta cytotoxic T-cell lymphoma. J Clin Neurosci. 2016; 26:138–40.
Article11. Arnulf B, Copie-Bergman C, Delfau-Larue MH, et al. Nonhepatosplenic gammadelta T-cell lymphoma: a subset of cytotoxic lymphomas with mucosal or skin localization. Blood. 1998; 91:1723–31.12. Garcia-Herrera A, Song JY, Chuang SS, et al. Nonhepatosplenic gammadelta T-cell lymphomas represent a spectrum of aggressive cytotoxic T-cell lymphomas with a mainly extranodal presentation. Am J Surg Pathol. 2011; 35:1214–25.13. Choe JY, Bisig B, de Leval L, Jeon YK. Primary gammadelta T cell lymphoma of the lung: report of a case with features suggesting derivation from intraepithelial gammadelta T lymphocytes. Virchows Arch. 2014; 465:731–6.14. Küçük C, Jiang B, Hu X, et al. Activating mutations of STAT5B and STAT3 in lymphomas derived from gammadelta-T or NK cells. Nat Commun. 2015; 6:6025.
Article15. Roberti A, Dobay MP, Bisig B, et al. Type II enteropathy-associated T-cell lymphoma features a unique genomic profile with highly recurrent SETD2 alterations. Nat Commun. 2016; 7:12602.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinal Cord Neurosarcoidosis after Cervical Compressive Myelopathy
- Early-Onset Myelopathy after High-voltage Electrical Burn: Case Report
- Primary central nervous system lymphoma in the brainstem and cervical spinal cord: a case report and literature review
- Surgical Treatment of Spinal Cord Intramedullary Cavernous Angioma
- A Case of Spinal Cord Glioblastoma Multiforme with Intracranial Metastasis