Anesth Pain Med.
2018 Apr;13(2):184-191. 10.17085/apm.2018.13.2.184.
A retrospective analysis of neurological complications after ultrasound guided interscalene block for arthroscopic shoulder surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Ewha Womans University School of Medicine, Seoul, Korea. ankyj@ewha.ac.kr
- KMID: 2437427
- DOI: http://doi.org/10.17085/apm.2018.13.2.184
Abstract
- BACKGROUND
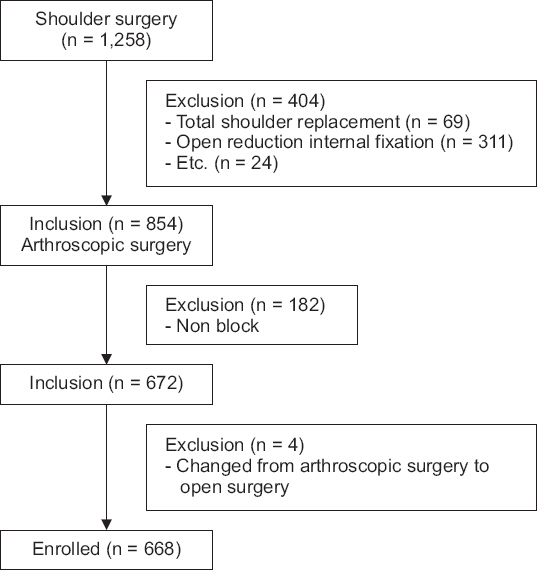
Ultrasound-guided interscalene brachial plexus block (US-ISB) has been reported to be effective postoperative analgesia for arthroscopic shoulder surgery. Although considered rare, various neurological complications have been reported. We retrospectively evaluated 668 patients for post operation neurological symptoms including hemidiaphragmatic paresis and post-operative neurologic symptoms after US-ISB.
METHODS
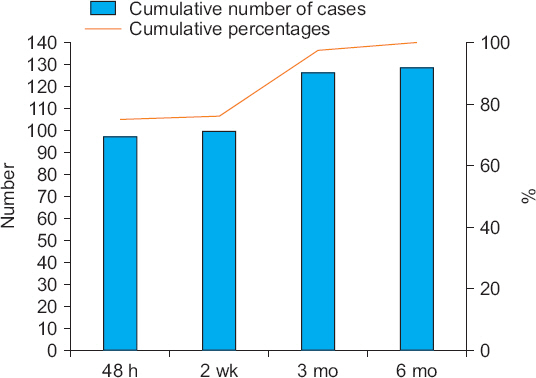
We performed a retrospective chart review of 668 patients undergoing shoulder surgery with single-shot US-ISB from January 2010 to May 2015. The general anesthesia prior to the US-guided ISB procedure was standardized by expert anesthesiologists. Neurological postoperative complications were evaluated at 48 hours, about 2 weeks, 1 month, 3 months, 6 months, and up to resolution after operation.
RESULTS
Three patients (0.4%) developed hemidiaphragmatic paresis (HDP), which were likely US-ISB associated and improved within 1 day. Two patients developed sensory symptoms, also likely US-ISB associated; one was paresthesia at the tip of the thumb/index finger, which resolved within 2 weeks, and the other was hypoesthesia involving the posterior auricular nerve, which resolved within 6 months. Motor and sensory symptoms which were not likely associated with US-ISB were hypoesthesia and pain (n = 28, 4.6%) and motor weakness (n = 2, 0.3%).
CONCLUSIONS
Incidence of HDP and neurological complications, respectively 0.4% and 0.3%, related to transient minor sensory symptoms occurred after US-ISB for arthroscopic shoulder surgery but the complications improved spontaneously. Therefore, we confirm that the US-ISB procedure with low volumes of local anesthetics is an acceptable technique with a low rate of HDP and neurological complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Borgeat A, Ekatodramis G, Kalberer F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. Anesthesiology. 2001; 95:875–80. DOI: 10.1097/00000542-200110000-00015. PMID: 11605927.2. Candido KD, Sukhani R, Doty R Jr, Nader A, Kendall MC, Yaghmour E, et al. Neurologic sequelae after interscalene brachial plexus block for shoulder/upper arm surgery: the association of patient, anesthetic, and surgical factors to the incidence and clinical course. Anesth Analg. 2005; 100:1489–95. DOI: 10.1213/01.ANE.0000148696.11814.9F. PMID: 15845712.3. Marhofer P, Anderl W, Heuberer P, Fritz M, Kimberger O, Marhofer D, et al. A retrospective analysis of 509 consecutive interscalene catheter insertions for ambulatory surgery. Anaesthesia. 2015; 70:41–6. DOI: 10.1111/anae.12840. PMID: 25209310.4. Moore DD, Maerz T, Anderson K. Shoulder surgeons'perceptions of interscalene nerve blocks and a review of complications rates in the literature. Phys Sportsmed. 2013; 41:77–84. DOI: 10.3810/psm.2013.09.2026. PMID: 24113705.5. Rajpal G, Winger DG, Cortazzo M, Kentor ML, Orebaugh SL. Neurologic outcomes after low-volume, ultrasound-guided interscalene block and ambulatory shoulder surgery. Reg Anesth Pain Med. 2016; 41:477–81. DOI: 10.1097/AAP.0000000000000425. PMID: 27281729.6. Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJ. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth. 2008; 101:549–56. DOI: 10.1093/bja/aen229. PMID: 18682410.7. Davis JJ, Swenson JD, Greis PE, Burks RT, Tashjian RZ. Interscalene block for postoperative analgesia using only ultrasound guidance: the outcome in 200 patients. J Clin Anesth. 2009; 21:272–7. DOI: 10.1016/j.jclinane.2008.08.022. PMID: 19502031.8. McNaught A, Shastri U, Carmichael N, Awad IT, Columb M, Cheung J, et al. Ultrasound reduces the minimum effective local anaesthetic volume compared with peripheral nerve stimulation for interscalene block. Br J Anaesth. 2011; 106:124–30. DOI: 10.1093/bja/aeq306. PMID: 21059701.9. Abdallah FW, Macfarlane AJ, Brull R. The requisites of needle-to-nerve proximity for ultrasound-guided regional anesthesia: a scoping review of the evidence. Reg Anesth Pain Med. 2016; 41:221–8. DOI: 10.1097/AAP.0000000000000201. PMID: 25785841.10. Barrington MJ, Kluger R. Ultrasound guidance reduces the risk of local anesthetic systemic toxicity following peripheral nerve blockade. Reg Anesth Pain Med. 2013; 38:289–99. DOI: 10.1097/AAP.0b013e318292669b. PMID: 23788067.11. Choi S, McCartney CJ. Evidence base for the use of ultrasound for upper extremity blocks:2014 update. Reg Anesth Pain Med. 2016; 41:242–50. DOI: 10.1097/AAP.0000000000000155. PMID: 25376973.12. Neal JM. Ultrasound-guided regional anesthesia and patient safety: update of an evidence-based analysis. Reg Anesth Pain Med. 2016; 41:195–204. DOI: 10.1097/AAP.0000000000000295. PMID: 26695877.13. Neal JM, Brull R, Horn JL, Liu SS, McCartney CJ, Perlas A, et al. The second american society of regional anesthesia and pain medicine evidence-based medicine assessment of ultrasound-guided regional anesthesia: executive summary. Reg Anesth Pain Med. 2016; 41:181–94. DOI: 10.1097/AAP.0000000000000331. PMID: 26695878.14. Hadzic A, Vloka J. Peripheral nerve blocks: principles and practice. New York: McGraw-Hill Companies, Inc;2004. p. 79–80.15. Dwyer T, Henry PD, Cholvisudhi P, Chan VW, Theodoropoulos JS, Brull R. Neurological complications related to elective orthopedic sSurgery: Part 1: common shoulder and elbow procedures. Reg Anesth Pain Med. 2015; 40:431–42. DOI: 10.1097/AAP.0000000000000178. DOI: 10.1097/AAP.0000000000000183.16. Rains DD, Rooke GA, Wahl CJ. Pathomechanisms and complications related to patient positioning and anesthesia during shoulder arthroscopy. Arthroscopy. 2011; 27:532–41. DOI: 10.1016/j.arthro.2010.09.008. PMID: 21186092.17. Li X, Eichinger JK, Hartshorn T, Zhou H, Matzkin EG, Warner JP. A comparison of the lateral decubitus and beach-chair positions for shoulder surgery: advantages and complications. J Am Acad Orthop Surg. 2015; 23:18–28. DOI: 10.5435/JAAOS-23-01-18. PMID: 25538127.18. Peruto CM, Ciccotti MG, Cohen SB. Shoulder arthroscopy positioning: lateral decubitus versus beach chair. Arthroscopy. 2009; 25:891–6. DOI: 10.1016/j.arthro.2008.10.003. PMID: 19664509.19. Selander D, Edshage S, Wolff T. Paresthesiae or no paresthesiae? Nerve lesions after axillary blocks. Acta Anaesthesiol Scand. 1979; 23:27–33. DOI: 10.1111/j.1399-6576.1979.tb01417.x. PMID: 425811.20. Klein SM, Greengrass RA, Steele SM, D'Ercole FJ, Speer KP, Gleason DH, et al. A comparison of 0.5% bupivacaine, 0.5% ropivacaine, and 0.75% ropivacaine for interscalene brachial plexus block. Anesth Analg. 1998; 87:1316–9. DOI: 10.1213/00000539-199812000-00019. DOI: 10.1097/00000539-199812000-00019. PMID: 9842819.21. Lee JH, Cho SH, Kim SH, Chae WS, Jin HC, Lee JS, et al. Ropivacaine for ultrasound-guided interscalene block:5 mL provides similar analgesia but less phrenic nerve paralysis than 10 mL. Can J Anaesth. 2011; 58:1001–6. DOI: 10.1007/s12630-011-9568-5. PMID: 21858614.22. Webb BG, Sallay PI, McMurray SD, Misamore GW. Comparison of interscalene brachial plexus block performed with and without steroids. Orthopedics. 2016; 39:e1100–3. DOI: 10.3928/01477447-20160819-02. PMID: 27575034.23. Woo JH, Kim YJ, Kim DY, Cho S. Dose-dependency of dexamethasone on the analgesic effect of interscalene block for arthroscopic shoulder surgery using ropivacaine 0.5%: a randomised controlled trial. Eur J Anaesthesiol. 2015; 32:650–5. DOI: 10.1097/EJA.0000000000000213. PMID: 25603389.24. Robaux S, Bouaziz H, Boisseau N, Raucoules-Aimé M, Laxenaire MC; S.O.S. Regional Hot Line Service. Persistent phrenic nerve paralysis following interscalene brachial plexus block. Anesthesiology. 2001; 95:1519–21. DOI: 10.1097/00000542-200112000-00035. PMID: 11748414.25. Orebaugh SL, Williams BA, Vallejo M, Kentor ML. Adverse outcomes associated with stimulator-based peripheral nerve blocks with versus without ultrasound visualization. Reg Anesth Pain Med. 2009; 34:251–5. DOI: 10.1097/AAP.0b013e3181a3438e. PMID: 19587625.26. Neal JM, Gerancher JC, Hebl JR, Ilfeld BM, McCartney CJ, Franco CD, et al. Upper extremity regional anesthesia: essentials of our current understanding 2008. Reg Anesth Pain Med. 2009; 34:134–70. DOI: 10.1097/AAP.0b013e31819624eb. PMID: 19282714. PMCID: PMC2779737.27. Neal JM. Ultrasound-guided regional anesthesia and patient safety: an evidence-based analysis. Reg Anesth Pain Med. 2010; 35(2 Suppl):S59–67. DOI: 10.1097/AAP.0b013e3181ccbc96. PMID: 20216027.28. Boulton AJ, Vinik AI, Arezzo JC, Bril V, Feldman EL, Freeman R, et al. Diabetic neuropathies: a statement by the American Diabetes Association. Diabetes Care. 2005; 28:956–62. DOI: 10.2337/diacare.28.4.956. PMID: 15793206.29. Park TS, Kim YS. Neuropraxia of the cutaneous nerve of the cervical plexus after shoulder arthroscopy. Arthroscopy. 2005; 21:631. DOI: 10.1016/j.arthro.2005.02.003. PMID: 15891736.30. Pearsall AW 4th, Holovacs TF, Speer KP. The low anterior five-o'clock portal during arthroscopic shoulder surgery performed in the beach-chair position. Am J Sports Med. 1999; 27:571–4. DOI: 10.1177/03635465990270050401. PMID: 10496571.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analgesic effect of low-dose levobupivacaine for ultrasound-guided interscalene brachial plexus block for arthroscopic shoulder surgery
- Ultrasound Guided Low Approach Interscalene Brachial Plexus Block for Upper Limb Surgery
- Feasibility of ultrasound-guided posterior approach for interscalene catheter placement during arthroscopic shoulder surgery
- Hypoesthesia of the Cutaneous Branch of Cervical Plexus after Shoulder Arthroscopy under General Anesthesia with Ultrasound Guided-Interscalene Block
- Comparison between two different concentrations of a fixed dose of ropivacaine in interscalene brachial plexus block for pain management after arthroscopic shoulder surgery: a randomized clinical trial