Acute Crit Care.
2018 Feb;33(1):23-33. 10.4266/acc.2017.00584.
The Effects of a Delirium Notification Program on the Clinical Outcomes of the Intensive Care Unit: A Preliminary Pilot Study
- Affiliations
-
- 1Department of Psychiatry and Institute of Behavioral Science in Medicine, Yonsei University College of Medicine, Seoul, Korea. EMPATHY@yuhs.ac
- 2Department of Psychiatry, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 3Department of Anesthesiology, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Psychiatry, Gangnam Severance Hospital, Yonsei University Health System, Seoul, Korea.
- 5Department of Biomedical Science and Engineering, Institute of Integrated Technology, Gwangju Institute of Science and Technology, Gwangju, Korea.
- KMID: 2436304
- DOI: http://doi.org/10.4266/acc.2017.00584
Abstract
- BACKGROUND
Delirium is common among intensive care unit (ICU) patients, so recent clinical guidelines recommended routine delirium monitoring in the ICU. But, its effect on the patient's clinical outcome is still controversial. In particular, the effect of systems that inform the primary physician of the results of monitoring is largely unknown.
METHODS
The delirium notification program using bedside signs and electronic chart notifications was applied to the pre-existing delirium monitoring protocol. Every patient was routinely evaluated for delirium, pain, and anxiety using validated tools. Clinical outcomes, including duration of delirium, ICU stay, and mortality were reviewed and compared for 3 months before and after the program implementation.
RESULTS
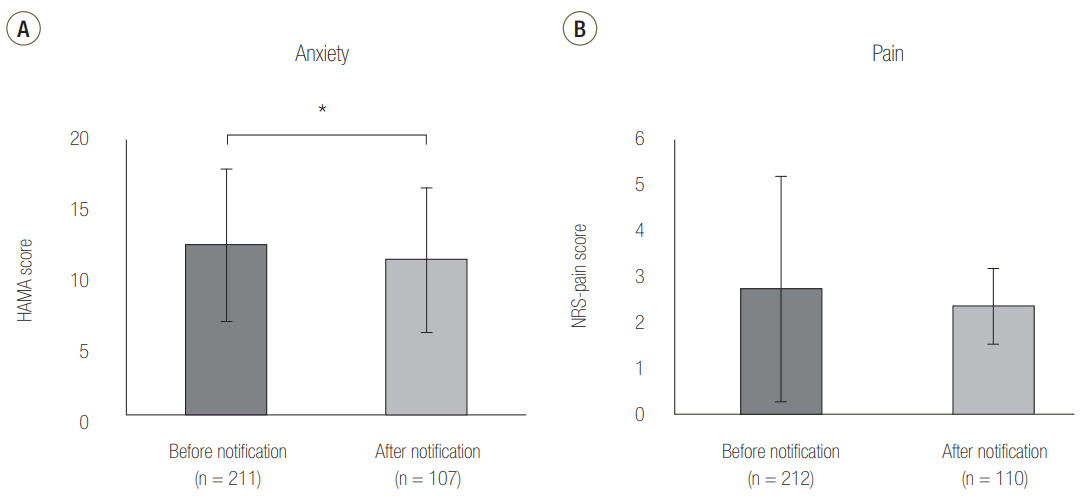
There was no significant difference between the two periods of delirium, ICU stay, and mortality. However, anxiety, an important prognostic factor in the ICU survivor's mental health, was significantly reduced and pain tended to decrease.
CONCLUSIONS
Increasing the physician's awareness of the patient's mental state by using a notification program could reduce the anxiety of ICU patients even though it may not reduce delirium. The results suggested that the method of delivering the results of monitoring was also an important factor in the success of the delirium monitoring program.
Keyword
MeSH Terms
Figure
Reference
-
1. Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM. Antipsychotic medication for prevention and treatment of delirium in hospitalized adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2016; 64:705–14.
Article2. Hshieh TT, Yue J, Oh E, Puelle M, Dowal S, Travison T, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015; 175:512–20.3. Peritogiannis V, Stefanou E, Lixouriotis C, Gkogkos C, Rizos DV. Atypical antipsychotics in the treatment of delirium. Psychiatry Clin Neurosci. 2009; 63:623–31.
Article4. Lynch EP, Lazor MA, Gellis JE, Orav J, Goldman L, Marcantonio ER. The impact of postoperative pain on the development of postoperative delirium. Anesth Analg. 1998; 86:781–5.
Article5. Oh J, Sohn JH, Shin CS, Na SH, Yoon HJ, Kim JJ, et al. Mutual relationship between anxiety and pain in the intensive care unit and its effect on medications. J Crit Care. 2015; 30:1043–8.
Article6. Chen CC, Li HC, Liang JT, Lai IR, Purnomo JD, Yang YT, et al. Effect of a modified hospital elder life program on delirium and length of hospital stay in patients undergoing abdominal surgery: a cluster randomized clinical trial. JAMA Surg. 2017; 152:827–34.7. Jeffs KJ, Berlowitz DJ, Grant S, Lawlor V, Graco M, de Morton NA, et al. An enhanced exercise and cognitive programme does not appear to reduce incident delirium in hospitalised patients: a randomised controlled trial. BMJ Open. 2013; 3:e002569.
Article8. Al-Qadheeb NS, Balk EM, Fraser GL, Skrobik Y, Riker RR, Kress JP, et al. Randomized ICU trials do not demonstrate an association between interventions that reduce delirium duration and short-term mortality: a systematic review and meta-analysis. Crit Care Med. 2014; 42:1442–54.9. Barr J, Fraser GL, Puntillo K, Ely EW, Gelinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013; 41:263–306.
Article10. Palacios-Ceña D, Cachón-Pérez JM, Martínez-Piedrola R, Gueita-Rodriguez J, Perez-de-Heredia M, Fernández-de-las-Peñas C. How do doctors and nurses manage delirium in intensive care units? A qualitative study using focus groups. BMJ Open. 2016; 6:e009678.
Article11. Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004; 291:1753–62.
Article12. Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010; 38:1513–20.
Article13. Pisani MA, Kong SY, Kasl SV, Murphy TE, Araujo KL, Van Ness PH. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med. 2009; 180:1092–7.
Article14. Leslie DL, Inouye SK. The importance of delirium: economic and societal costs. J Am Geriatr Soc. 2011; 59 Suppl 2:S241–3.
Article15. Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008; 168:27–32.
Article16. Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012; 367:30–9.
Article17. Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013; 369:1306–16.
Article18. Page VJ, Navarange S, Gama S, McAuley DF. Routine delirium monitoring in a UK critical care unit. Crit Care. 2009; 13:R16.
Article19. Luetz A, Weiss B, Boettcher S, Burmeister J, Wernecke KD, Spies C. Routine delirium monitoring is independently associated with a reduction of hospital mortality in critically ill surgical patients: a prospective, observational cohort study. J Crit Care. 2016; 35:168–73.
Article20. Trogrlić Z, van der Jagt M, Bakker J, Balas MC, Ely EW, van der Voort PH, et al. A systematic review of implementation strategies for assessment, prevention, and management of ICU delirium and their effect on clinical outcomes. Crit Care. 2015; 19:157.
Article21. Andrews L, Silva SG, Kaplan S, Zimbro K. Delirium monitoring and patient outcomes in a general intensive care unit. Am J Crit Care. 2015; 24:48–56.
Article22. Jung JH, Lim JH, Kim EJ, An HC, Kang MK, Lee J, et al. The experience of delirium care and clinical feasibility of the CAM-ICU in a Korean ICU. Clin Nurs Res. 2013; 22:95–111.
Article23. Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med. 2001; 29:1370–9.
Article24. Heo EY, Lee BJ, Hahm BJ, Song EH, Lee HA, Yoo CG, et al. Translation and validation of the Korean confusion assessment method for the intensive care unit. BMC Psychiatry. 2011; 11:94.
Article25. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res (Hoboken). 2011; 63 Suppl 11:S240–52.26. Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001; 94:149–58.
Article27. Bruss GS, Gruenberg AM, Goldstein RD, Barber JP. Hamilton anxiety rating scale interview guide: joint interview and test-retest methods for interrater reliability. Psychiatry Res. 1994; 53:191–202.
Article28. Shear MK, Vander Bilt J, Rucci P, Endicott J, Lydiard B, Otto MW, et al. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A). Depress Anxiety. 2001; 13:166–78.
Article29. Yu A, Teitelbaum J, Scott J, Gesin G, Russell B, Huynh T, et al. Evaluating pain, sedation, and delirium in the neurologically critically ill-feasibility and reliability of standardized tools: a multi-institutional study. Crit Care Med. 2013; 41:2002–7.30. Chanques G, Viel E, Constantin JM, Jung B, de Lattre S, Carr J, et al. The measurement of pain in intensive care unit: comparison of 5 self-report intensity scales. Pain. 2010; 151:711–21.
Article31. Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med. 1981; 9:591–7.
Article32. Girard TD, Shintani AK, Jackson JC, Gordon SM, Pun BT, Henderson MS, et al. Risk factors for posttraumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care. 2007; 11:R28.
Article33. Castillo MI, Cooke ML, Macfarlane B, Aitken LM. Trait anxiety but not state anxiety during critical illness was associated with anxiety and depression over 6 months after ICU. Crit Care Med. 2016; 44:100–10.
Article34. Zaal IJ, Devlin JW, Peelen LM, Slooter AJ. A systematic review of risk factors for delirium in the ICU. Crit Care Med. 2015; 43:40–7.
Article35. Huai J, Ye X. A meta-analysis of critically ill patients reveals several potential risk factors for delirium. Gen Hosp Psychiatry. 2014; 36:488–96.
Article36. Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001; 27:1892–900.
Article37. Martinez F, Tobar C, Hill N. Preventing delirium: should non-pharmacological, multicomponent interventions be used? A systematic review and metaanalysis of the literature. Age Ageing. 2015; 44:196–204.
Article38. DAS-Taskforce 2015, Baron R, Binder A, Biniek R, Braune S, Buerkle H, et al. Evidence and consensus based guideline for the management of delirium, analgesia, and sedation in intensive care medicine: revision 2015 (DAS-guideline 2015)-short version. Ger Med Sci. 2015; 13:19.39. Fleischer S, Berg A, Behrens J, Kuss O, Becker R, Horbach A, et al. Does an additional structured information program during the intensive care unit stay reduce anxiety in ICU patients? A multicenter randomized controlled trial. BMC Anesthesiol. 2014; 14:48.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Influencing Intensive Care Unit Nurses’ Competency in Delirium Care in A Tertiary General Hospital
- Delirium in the intensive care unit
- Effects of a Multifaceted Pediatric Delirium Education Program for Pediatric Intensive Care Unit Nurses on their Delirium Knowledge, Self-confidence in Delirium Nursing, and Delirium Assessment Accuracy: A One Group Pretest-Posttest Design
- Investigation of Delirium Occurrence and Intervention Status in Intensive Care Unit at a Hospital and Perception of Delirium by Medical Staff
- Intensive Care Unit Nurse's Knowledge, Nursing Performance, and Stress about Delirium