Ann Lab Med.
2018 Sep;38(5):402-412. 10.3343/alm.2018.38.5.402.
Reducing Test Utilization in Hospital Settings: A Narrative Review
- Affiliations
-
- 1Departments of Clinical Chemistry and Haematology, University Medical Center Utrecht, Utrecht, The Netherlands.
- 2Section Acute Medicine, Department of Internal Medicine, VU University Medical Center, Amsterdam, The Netherlands. p.nanayakkara@vumc.nl
- 3Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht, The Netherlands.
- KMID: 2434728
- DOI: http://doi.org/10.3343/alm.2018.38.5.402
Abstract
- BACKGROUND
Studies addressing the appropriateness of laboratory testing have revealed approximately 20% overutilization. We conducted a narrative review to (1) describe current interventions aimed at reducing unnecessary laboratory testing, specifically in hospital settings, and (2) provide estimates of their efficacy in reducing test order volume and improving patient-related clinical outcomes.
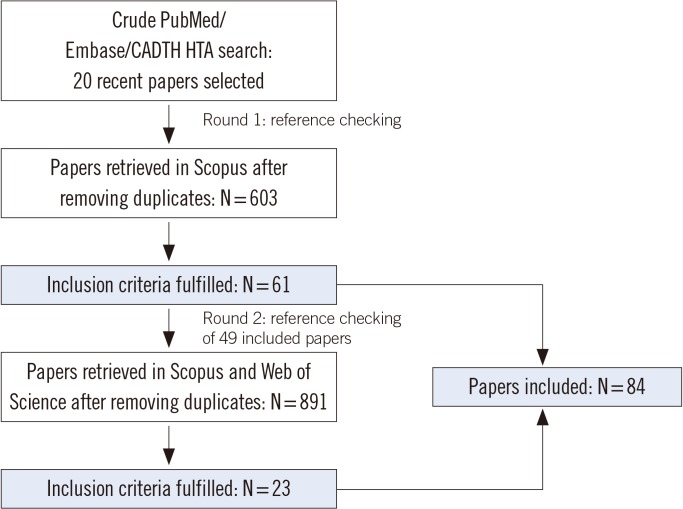
METHODS
The PubMed, Embase, Scopus, Web of Science, and Canadian Agency for Drugs and Technologies in Health-Health Technology Assessment databases were searched for studies describing the effects of interventions aimed at reducing unnecessary laboratory tests. Data on test order volume and clinical outcomes were extracted by one reviewer, while uncertainties were discussed with two other reviewers. Because of the heterogeneity of interventions and outcomes, no meta-analysis was performed.
RESULTS
Eighty-four studies were included. Interventions were categorized into educational, (computerized) provider order entry [(C)POE], audit and feedback, or other interventions. Nearly all studies reported a reduction in test order volume. Only 15 assessed sustainability up to two years. Patient-related clinical outcomes were reported in 45 studies, two of which found negative effects.
CONCLUSIONS
Interventions from all categories have the potential to reduce unnecessary laboratory testing, although long-term sustainability is questionable. Owing to the heterogeneity of the interventions studied, it is difficult to conclude which approach was most successful, and for which tests. Most studies had methodological limitations, such as the absence of a control arm. Therefore, well-designed, controlled trials using clearly described interventions and relevant clinical outcomes are needed.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Sustainability in Healthcare: Perspectives and Reflections Regarding Laboratory Medicine
Aroa Molero, Michele Calabrò, Maguelone Vignes, Bernard Gouget, Damien Gruson
Ann Lab Med. 2021;41(2):139-144. doi: 10.3343/alm.2021.41.2.139.
Reference
-
1. van Rooijen M, Goedvolk R, Houwert T. A vision for the Dutch health care system in 2040-Towards a sustainable, high-quality health care system. In : World Economic Forum; 2013.2. Hauser RG, Shirts BH. Do we now know what inappropriate laboratory utilization is? Am J Clin Pathol. 2014; 141:774–783. PMID: 24838320.3. Minerowicz C, Abel N, Hunter K, Behling KC, Cerceo E, Bierl C. Impact of weekly feedback on test ordering patterns. Am J Manag Care. 2015; 21:763–768. PMID: 26633250.4. Kobewka DM, Ronksley PE, McKay JA, Forster AJ, Van Walraven C. Influence of educational, audit and feedback, system based, and incentive and penalty interventions to reduce laboratory test utilization: A systematic review. Clin Chem Lab Med. 2015; 53:157–183. PMID: 25263310.5. Zhi M, Ding EL, Theisen-Toupal J, Whelan J, Arnaout R. The landscape of inappropriate laboratory testing: a 15-year meta-analysis. PLoS One. 2013; 8:e78962. PMID: 24260139.6. NVKC. Zinnige Diagnostiek-Overwegingen bij het aanvragen en interpreteren van laboratoriumdiagnostiek (Usefull Diagnostics-Considerations upon requesting and interpreting laboratory diagnostics). Nederlandse Vereniging voor Klinische Chemie (Netherlands Society for Clinical Chemistry and Laboratory Medicine).7. Pageler NM, Franzon D, Longhurst CA, Wood M, Shin AY, Adams ES, et al. Embedding time-limited laboratory orders within computerized provider order entry reduces laboratory utilization. Pediatr Crit Care Med. 2013; 14:413–419. PMID: 23439456.8. Thakkar RN, Kim D, Knight AM, Riedel S, Vaidya D, Wright SM. Impact of an educational intervention on the frequency of daily blood test orders for hospitalized patients. Am J Clin Pathol. 2015; 143:393–397. PMID: 25696797.9. Kumwilaisak K, Noto A, Schmidt UH, Beck CI, Crimi C, Lewandrowski K, et al. Effect of laboratory testing guidelines on the utilization of tests and order entries in a surgical intensive care unit. Crit Care Med. 2008; 36:2993–2999. PMID: 18824907.10. Erlingsdóttir H, Jóhannesson A, Ásgeirsdóttir TL. Can physician laboratory-test requests be influenced by interventions? Scand J Clin Lab Invest. 2015; 75:18–26. PMID: 25300377.11. Miyakis S, Karamanof G, Liontos M, Mountokalakis TD. Factors contributing to inappropriate ordering of tests in an academic medical department and the effect of an educational feedback strategy. Postgrad Med J. 2006; 82:823–829. PMID: 17148707.12. Vegting IL, Van Beneden M, Kramer MHH, Thijs A, Kostense PJ, Nanayakkara PWB. How to save costs by reducing unnecessary testing: Lean thinking in clinical practice. Eur J Intern Med. 2012; 23:70–75. PMID: 22153535.13. Solomon DH, Hashimoto H, Daltroy L, Liang MH. Techniques to improve physicians' use of diagnostic tests: a new conceptual framework. JAMA. 1998; 280:2020–2027. PMID: 9863854.14. Yarbrough PM, Kukhareva PV, Horton D, Edholm K, Kawamoto K. Multifaceted intervention including education, rounding checklist implementation, cost feedback, and financial incentives reduces inpatient laboratory costs. J Hosp Med. 2016; 11:348–354. PMID: 26843272.15. Finegan BA, Rashiq S, McAlister FA, O'Connor P. Selective ordering of preoperative investigations by anesthesiologists reduces the number and cost of tests. Can J Anaesth. 2005; 52:575–580. PMID: 15983141.16. Smit I, Zemlin AE, Erasmus RT. Demand management: an audit of chemical pathology test rejections by an electronic gate-keeping system at an academic hospital in Cape Town. Ann Clin Biochem. 2015; 52:481–487. PMID: 25527691.17. Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PAC, et al. Why don't physicians follow clinical practice guidelines?: a framework for improvement. JAMA. 1999; 282:1458–1465. PMID: 10535437.18. Meng QH, Zhu S, Booth C, Stevens L, Bertsch B, Qureshi M, et al. Impact of the cardiac troponin testing algorithm on excessive and inappropriate troponin test requests. Am J Clin Pathol. 2006; 126:195–199. PMID: 16891193.19. Konger RL, Ndekwe P, Jones G, Schmidt RP, Trey M, Baty EJ, et al. Reduction in unnecessary clinical laboratory testing through utilization management at a US government veterans affairs hospital. Am J Clin Pathol. 2016; 145:355–364. PMID: 27124918.20. Powles LAR, Rolls AE, Lamb BW, Taylor E, Green JSA. Can redesigning a laboratory request form reduce the number of inappropriate PSA requests without compromising clinical outcome. Br J Med Surg Urol. 2012; 567–573.21. Larochelle MR, Knight AM, Pantle H, Riedel S, Trost JC. Reducing excess cardiac biomarker testing at an academic medical center. J Gen Intern Med. 2014; 29:1468–1474. PMID: 24973056.22. Attali M, Barel Y, Somin M, Beilinson N, Shankman M, Ackerman A, et al. A cost-effective method for reducing the volume of laboratory tests in a university-associated teaching hospital. Mt Sinai J Med. 2006; 73:787–794. PMID: 17008940.23. Delvaux N, Van Thienen K, Heselmans A, Van de, Ramaekers D, Aertgeerts B. The effects of computerized clinical decision support systems on laboratory test ordering-a systematic review. Arch Pathol Lab Med. 2017; 141:585–595. PMID: 28353386.24. Iams W, Heck J, Kapp M, Leverenz D, Vella M, Szentirmai E, et al. A multidisciplinary housestaff-led initiative to safely reduce daily laboratory testing. Acad Med. 2016; 91:813–820. PMID: 27028031.25. Tawfik B, Collins JB, Fino NF, Miller DP. House officer-driven reduction in laboratory utilization. South Med J. 2016; 109:5–10. PMID: 26741863.26. Cadogan SL, Browne JP, Bradley CP, Cahill MR. The effectiveness of interventions to improve laboratory requesting patterns among primary care physicians: a systematic review. Implement Sci. 2015; 10:167. PMID: 26637335.27. Aesif SW, Parenti DM, Lesky L, Keiser JF. A cost-effective interdisciplinary approach to microbiologic send-out test use. Arch Pathol Lab Med. 2015; 139:194–198. PMID: 24758733.28. Blum FE, Lund ET, Hall HA, Tachauer AD, Chedrawy EG, Zilberstein J. Reevaluation of the utilization of arterial blood gas analysis in the intensive care unit: effects on patient safety and patient outcome. J Crit Care. 2015; 30:438.29. Greenblatt MB, Nowak JA, Quade CC, Tanasijevic M, Lindeman N, Jarolim P. Impact of a prospective review program for reference laboratory testing requests. Am J Clin Pathol. 2015; 143:627–634. PMID: 25873495.30. DellaVolpe JD, Chakraborti C, Cerreta K, Romero CJ, Firestein CE, Myers L, et al. Effects of implementing a protocol for arterial blood gas use on ordering practices and diagnostic yield. Healthc (Amst). 2014; 2:130–135. PMID: 26250381.31. Dickerson JA, Cole B, Conta JH, Wellner M, Wallace SE, Jack RM, et al. Improving the value of costly genetic reference laboratory testing with active utilization management. Arch Pathol Lab Med. 2014; 138:110–113. PMID: 24377818.32. Delgado-Corcoran C, Bodily S, Frank DU, Witte MK, Castillo R, Bratton SL. Reducing blood testing in pediatric patients after heart surgery: a quality improvement project. Pediatr Crit Care Med. 2014; 15:756–761. PMID: 25068246.33. Seegmiller AC, Kim AS, Mosse CA, Levy MA, Thompson MA, Kressin MK, et al. Optimizing personalized bone marrow testing using an evidence-based, interdisciplinary team approach. Am J Clin Pathol. 2013; 140:643–650. PMID: 24124142.34. Gentile NT, Ufberg J, Barnum M, McHugh M, Karras D. Guidelines reduce X-ray and blood gas utilization in acute asthma. Am J Emerg Med. 2003; 21:451–453. PMID: 14574649.35. Davidoff F, Goodspeed R, Clive J. Changing test ordering behavior: a randomized controlled trial comparing probabilistic reasoning with cost-containment education. Med Care. 1989; 27:45–58. PMID: 2492066.36. FowkesFGR , Hall R, Jones JH, Scanlon MF, Elder GH, Hobbs DR, et al. Trial of strategy for reducing the use of laboratory tests. Br Med J (Clin Res Ed). 1986; 292:883–885.37. Giordano D, Zasa M, Iaccarino C, Vincenti V, Dascola I, Brevi BC, et al. Improving laboratory test ordering can reduce costs in surgical wards. Acta Biomed. 2015; 86:32–37.38. Corson AH, Fan VS, White T, Sullivan SD, Asakura K, Myint M, et al. A multifaceted hospitalist quality improvement intervention: decreased frequency of common labs. J Hosp Med. 2015; 10:390–395. PMID: 25809958.39. Salman M, Pike DC, Wu R, Oncken C. Effectiveness and safety of a clinical decision rule to reduce repeat ionized calcium testing: a pre/post test intervention. Conn Med. 2016; 80:5–10. PMID: 26882784.40. Svecova N, Sammut L. Update on inappropriate C-reactive protein testing in epistaxis patients. Clin Otolaryngol. 2013; 38:192.41. Moyer AM, Saenger AK, Willrich M, Donato LJ, Baumann NA, Block DR, et al. implementation of clinical decision support rules to reduce repeat measurement of serum ionized calcium, serum magnesium, and N-terminal Pro-B-type natriuretic peptide in intensive care unit inpatients. Clin Chem. 2016; 62:824–830. PMID: 27022069.42. Santos IS, Bensenor IM, Machado JB, Fedeli LM, Lotufo PA. Intervention to reduce C-reactive protein determination requests for acute infections at an emergency department. Emerg Med J. 2012; 29:965–968. PMID: 22307925.43. Lippi G, Brambilla M, Bonelli P, Aloe R, Balestrino A, Nardelli A, et al. Effectiveness of a computerized alert system based on re-testing intervals for limiting the inappropriateness of laboratory test requests. Clin Biochem. 2015; 48:1174–1176. PMID: 26074445.44. Prat G, Lefèvre M, Nowak E, Tonnelier JM, Renault A, L'Her E, et al. Impact of clinical guidelines to improve appropriateness of laboratory tests and chest radiographs. Intensive Care Med. 2009; 35:1047–1053. PMID: 19221715.45. Levick DL, Stern G, Meyerhoefer CD, Levick A, Pucklavage D. Reducing unnecessary testing in a CPOE system through implementation of a targeted CDS intervention. BMC Med Inform Decis Mak. 2013; 13:43. PMID: 23566021.46. Niès J, Colombet I, Zapletal E, Gillaizeau F, Durieux P. Effects of automated alerts on unnecessarily repeated serology tests in a cardiovascular surgery department: a time series analysis. BMC Health Serv Res. 2010; 10:70. PMID: 20298618.47. Chen P, Tanasijevic MJ, Schoenenberger RA, Fiskio J, Kuperman GJ, Bates DW. A computer-based intervention for improving the appropriateness of antiepileptic drug level monitoring. Am J Clin Pathol. 2003; 119:432–438. PMID: 12645347.48. Wisser D, Van Ackern K, Knoll E, Wisser H, Bertsch T. Blood loss from laboratory tests. Clin Chem. 2003; 49:1651–1655. PMID: 14500590.49. Bates DW, Kuperman GJ, Rittenberg E, Teich JM, Fiskio J, Ma'luf N, et al. A randomized trial of a computer-based intervention to reduce utilization of redundant laboratory tests. Am J Med. 1999; 106:144–150. PMID: 10230742.50. Merlani P, Garnerin P, Diby M, Ferring M, Ricou B. Linking guideline to regular feedback to increase appropriate requests for clinical tests: blood gas analysis in intensive care. Br Med J. 2001; 323:620–624. PMID: 11557715.51. Barie PS, Hydo LJ. Learning to not know: results of a program for ancillary cost reduction in surgical care. J Trauma. 1996; 41:714–720. PMID: 8858034.52. Gortmaker SL, Bickford AF, Mathewson HO, Dumbaugh K, Tirrell PC. A successful experiment to reduce unnecessary laboratory use in a community hospital. Med Care. 1988; 26:631–642. PMID: 3132579.53. Procop GW, Yerian LM, Wyllie R, Harrison AM, Kottke-Marchant K. Duplicate laboratory test reduction using a clinical decision support tool. Am J Clin Pathol. 2014; 141:718–723. PMID: 24713745.54. De Bie P, Tepaske R, Hoek A, Sturk A, Van Dongen-Lases E. Reduction in the number of reported laboratory results for an adult intensive care unit by effective order management and parameter selection on the blood gas analyzers. Point Care. 2016; 15:7–10.55. Waldron JL, Ford C, Dobie D, Danks G, Humphrey R, Rolli A, et al. An automated minimum retest interval rejection rule reduces repeat CRP workload and expenditure, and influences clinician-requesting behaviour. J Clin Pathol. 2014; 67:731–733. PMID: 24898477.56. Krasowski MD, Savage J, Ehlers A, Maakestad J, Schmidt GA, La'ulu SL, et al. Ordering of the serum angiotensin-converting enzyme test in patients receiving angiotensin-converting enzyme inhibitor therapy an avoidable but common error. Chest. 2015; 148:1447–1453. PMID: 26225637.57. Janssens PMW, Wasser G. Managing laboratory test ordering through test frequency filtering. Clin Chem Lab Med. 2013; 51:1207–1215. PMID: 23454715.58. Wang TJ, Mort EA, Nordberg P, Chang Y, Cadigan ME, Mylott L, et al. A utilization management intervention to reduce unnecessary testing in the coronary care unit. Arch Intern Med. 2002; 162:1885–1890. PMID: 12196088.59. Toubert ME, Chevret S, Cassinat B, Schlageter MH, Beressi JP, Rain JD. From guidelines to hospital practice: reducing inappropriate ordering of thyroid hormone and antibody tests. Eur J Endocrinol. 2000; 142:605–610. PMID: 10822223.60. Procop GW, Keating C, Stagno P, Kottke-Marchant K, Partin M, Tuttle R, et al. Reducing duplicate testing: A comparison of two clinical decision support tools. Am J Clin Pathol. 2015; 143:623–626. PMID: 25873494.61. Ko A, Murry JS, Hoang DM, Harada MY, Aquino L, Coffey C, et al. High-value care in the surgical intensive care effect on ancillary resources. J Surg Res. 2016; 202:455–460. PMID: 27041599.62. Kobkitjaroen J, Pongprasobchai S, Tientadakul P. γ-Glutamyl transferase testing, change of its designation on the laboratory request form, and resulting ratio of inappropriate to appropriate use. Lab Med. 2015; 46:265–270. PMID: 26199270.63. Le Maguet P, Asehnoune K, Autet LM, Gaillard T, Lasocki S, Mimoz O, et al. Transitioning from routine to on-demand test ordering in intensive care units: a prospective, multicentre, interventional study. Br J Anaesth. 2015; 115:941–942. PMID: 26582861.64. Janssens PMW, Staring W, Winkelman K, Krist G. Active intervention in hospital test request panels pays. Clin Chem Lab Med. 2015; 53:731–742. PMID: 25301675.65. Mallows JL. The effect of a gold coin fine on C-reactive protein test ordering in a tertiary referral emergency department. Med J Aust. 2013; 199:813–814. PMID: 24329676.66. Fang DZ, Sran G, Gessner D, Loftus PD, Folkings A, Christopher JY III, et al. Cost and turn-around time display decreases inpatient ordering of reference laboratory tests: a time series. BMJ Qual Saf. 2014; 23:994–1000.67. Chu KH, Wagholikar AS, Greenslade JH, O'Dwyer JA, Brown AF. Sustained reductions in emergency department laboratory test orders: impact of a simple intervention. Postgrad Med J. 2013; 89:566–571. PMID: 23737505.68. Nightingale P, Peters M, Mutimer D, Neuberger J. Effects of a computerised protocol management system on ordering of clinical tests. Qual Health Care. 1994; 3:23–28. PMID: 10171956.69. Feldman LS, Shihab HM, Thiemann D, Yeh HC, Ardolino M, Mandell S, et al. Impact of providing fee data on laboratory test ordering: a controlled clinical trial. JAMA Intern Med. 2013; 173:903–908. PMID: 23588900.70. Algaze C, Wood M, Pageler N, Sharek P, Longhurst C, Shin A. Use of a checklist and clinical decision support tool reduces laboratory use and improves cost. Pediatrics. 2016; 137:1–8.71. Durieux P, Ravaud P, Porcher R, Fulla Y, Manet CS, Chaussade S. Long-term impact of a restrictive laboratory test ordering form on tumor marker prescriptions. Int J Technol Assess Health Care. 2003; 19:106–113. PMID: 12701943.72. Petrou P. Failed attempts to reduce inappropriate laboratory utilization in an emergency department setting in Cyprus: lessons learned. J Emerg Med. 2016; 50:510–517. PMID: 26433423.73. Seguin P, Bleichner J, Grolier J, Guillou Y, Mallédant Y. Effects of price information on test ordering in an intensive care unit. Intensive Care Med. 2002; 28:332–335. PMID: 11904664.74. Barth JH, Balen AH, Jennings A. Appropriate design of biochemistry request cards can promote the use of protocols and reduce unnecessary investigations. Ann Clin Biochem. 2001; 38:714–716. PMID: 11732657.75. Merkeley HL, Hemmett J, Cessford TA, Amiri N, Geller GS, Baradaran N, et al. Multipronged strategy to reduce routine-priority blood testing in intensive care unit patients. J Crit Care. 2016; 31:212–216. PMID: 26476580.76. Emerson JF, Emerson SS. The impact of requisition design on laboratory utilization. Am J Clin Pathol. 2001; 116:879–884. PMID: 11764077.77. Pysher TJ, Bach PR, Lowichik A, Petersen MD, Shields LH. Chemistry test ordering patterns after elimination of predefined multitest chemistry panels in a children's hospital. Pediatr Dev Pathol. 1999; 2:446–453. PMID: 10441622.78. Hutton HD, Drummond HS, Fryer AA. The rise and fall of C-reactive protein: managing demand within clinical biochemistry. Ann Clin Biochem. 2009; 46:155–158. PMID: 19164341.79. Bates DW, Kuperman GJ, Jha A, Teich JM, John Orav E, Ma'luf N, et al. Does the computerized display of charges affect inpatient ancillary test utilization? Arch Intern Med. 1997; 157:2501–2508. PMID: 9385303.80. Durand-Zaleski I, Roudot-Thoraval F, Rymer JC, Rosa J, Revuz J. Reducing unnecessary laboratory use with new test request form: example of tumour markers. Lancet. 1993; 342:150–153. PMID: 8101259.81. Iturrate E, Jubelt L, Volpicelli F, Hochman K. Optimize your electronic medical record to increase value: reducing laboratory overutilization. Am J Med. 2016; 129:215–220. PMID: 26475957.82. Han SJ, Saigal R, Rolston JD, Cheng JS, Lau CY, Mistry RI, et al. Targeted reduction in neurosurgical laboratory utilization: resident-led effort at a single academic institution. J Neurosurg. 2014; 120:173–177. PMID: 24125592.83. May TA, Clancy M, Critchfield J, Ebeling F, Enriquez A, Gallagher C, et al. Reducing unnecessary inpatient laboratory testing in a teaching hospital. Am J Clin Pathol. 2006; 126:200–206. PMID: 16891194.84. Niemeijer GC, Trip A, Ahaus KCTB, Wendt KW, Does RJMM. Quality quandaries: reducing overuse of diagnostic tests for trauma patients. Qual Eng. 2012; 24:558–563.85. Marx WH, DeMaintenon NL, Mooney KF, Mascia ML, Medicis J, Franklin PD, et al. Cost reduction and outcome improvement in the intensive care unit. J Trauma. 1999; 46:625–630. PMID: 10217225.86. Martin AR, Wolf MA, Thibodeau LA, Dzau V, Braunwald E. A trial of two strategies to modify the test-ordering behavior of medical residents. N Engl J Med. 1980; 303:1330–1336. PMID: 7432374.87. Zalts R, Ben-Hur D, Yahia A, Khateeb J, Belsky V, Grushko N, et al. Hospital care efficiency and the SMART (specific, measurable, agreed, required, and timely) medicine initiative. JAMA Intern Med. 2016; 176:398–399. PMID: 26831353.88. Zlabek JA, Wickus JW, Mathiason MA. Early cost and safety benefits of an inpatient electronic health record. J Am Med Inform Assoc. 2011; 18:169–172. PMID: 21292703.89. Amukele TK, Baird GS, Chandler WL. Reducing the use of coagulation test panels. Blood Coagul Fibrinolysis. 2011; 22:688–695. PMID: 21934488.90. Dorizzi RM, Ferrari A, Rossini A, Mozzo U, Meneghelli S, Melloni N, et al. Tumour markers workload of an university hospital laboratory two years after the redesign of the optical reading request forms. Accred Qual Assur. 2008; 13:133–137.91. Calderon-Margalit R, Mor-Yosef S, Mayer M, Adler B, Shapira SC. An administrative intervention to improve the utilization of laboratory tests within a university hospital. Int J Qual Health Care. 2005; 17:243–248. PMID: 15837715.92. Rosenbloom S, Chiu K, Byrne D, Talbert D, Neilson E, Miller R. Interventions to regulate ordering of serum magnesium levels: report of an unintended consequence of decision support. J Am Med Inform Assoc. 2005; 12:546–553. PMID: 15905483.93. Vidyarthi AR, Hamill T, Green AL, Rosenbluth G, Baron RB. Changing resident test ordering behavior: a multilevel intervention to decrease laboratory utilization at an academic medical center. Am J Med Qual. 2015; 30:81–87. PMID: 24443317.94. Kim JY, Dzik WH, Dighe AS, Lewandrowski KB. Utilization management in a large urban academic medical center: a 10-year experience. Am J Clin Pathol. 2011; 135:108–118. PMID: 21173132.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- “Leisure Life Satisfaction:” Will It Have a Beneficial Impact on Depression Among Older Adults in Community Care Settings in Korea?
- Strategies for sustaining and enhancing nursing students’ engagement in academic and clinical settings: a narrative review
- Present and Future of Research on Continuous Glucose Monitoring: A Narrative Review
- Teaching Medical Humanities through an Illness Narrative
- The mechanism of action of pulsed radiofrequency in reducing pain: a narrative review