J Korean Neurosurg Soc.
2019 Jan;62(1):96-105. 10.3340/jkns.2017.0214.
Analysis of the Risk Factors for Unfavorable Radiologic Outcomes after Fusion Surgery in Thoracolumbar Burst Fracture : What Amount of Postoperative Thoracolumbar Kyphosis Correction is Reasonable?
- Affiliations
-
- 1Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. grandblue@gnah.co.kr
- 2Department of Orthopaedic Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 3Spine Center, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 4Department of Emergency Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 5Department of Neurological Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 6Department of Radiology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- KMID: 2434351
- DOI: http://doi.org/10.3340/jkns.2017.0214
Abstract
OBJECTIVE
The aims in the management of thoracolumbar spinal fractures are not only to restore vertebral column stability, but also to obtain acceptable alignment of the thoracolumbar junction (T-L junction) to prevent complications. However, insufficient surgical correction of the thoracolumbar spine would be likely to cause late progression of abnormal kyphosis. Therefore, we identified the surgical factors that affected unfavorable radiologic outcomes of the thoracolumbar spine after surgery.
METHODS
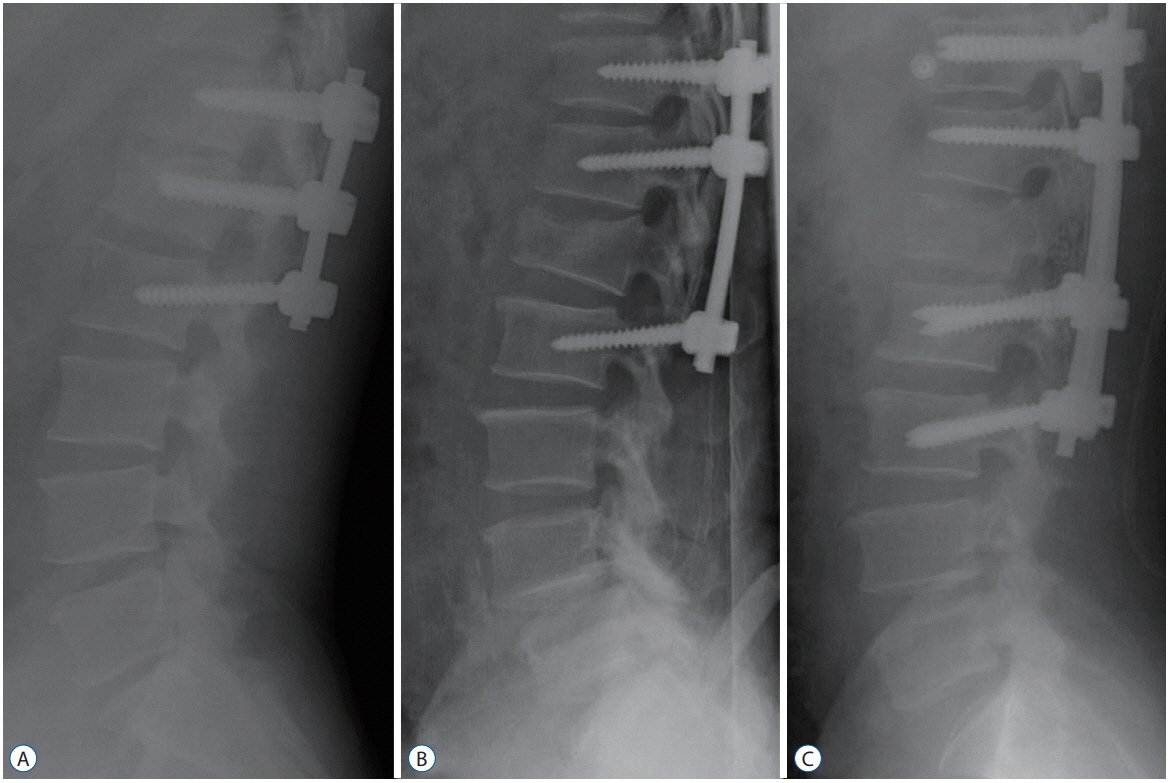
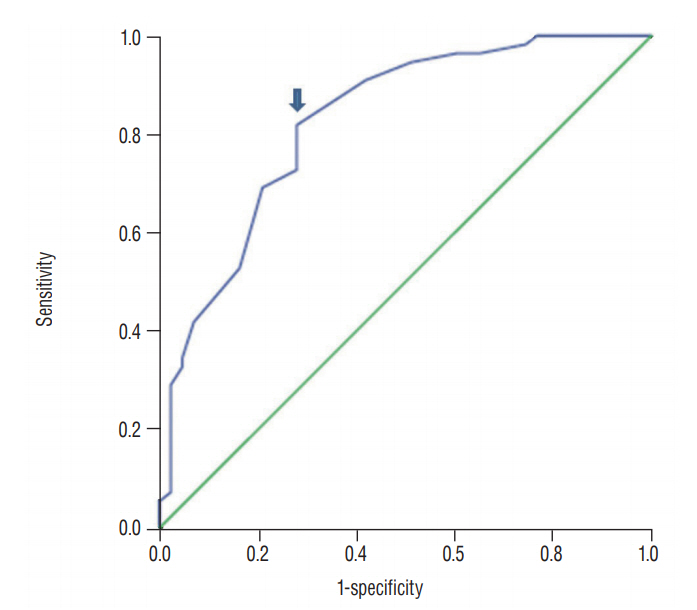
This study was conducted in a single institution from January 2007 to December 2013. A total of 98 patients with unstable thoracolumbar spine fracture were included. In these patients, fixation was done through transpedicular screws with rods by three surgical patterns. We reviewed digital radiographs and analyzed the images preoperatively and postoperatively during follow-up visits to compare the change of the thoracolumbar Cobb angle with radiologic parameters and clinical outcomes. The unfavorable radiologic group was defined as the patients who were measured as having greater than 20 degrees of thoracolumbar Cobb angle on the last follow-up, or who underwent kyphotic progression of thoracolumbar Cobb angle greater than 10 degrees from the immediate postoperative state to final follow-up, or who had overt instrument failure with/without additional surgery. We assessed the risk factors that affected the unfavorable radiologic outcomes.
RESULTS
We had 43 patients with unfavorable radiologic outcomes, including 35 abnormal thoracolumbar alignments and 14 instrumental failures with/without additional surgery. The multivariate logistic regression test showed that immediate postoperative T-L junction Cobb angle less than 10.5 degrees was a statistically significant risk factor, as well as the presence of osteoporosis (p=0.017 and 0.049, respectively).
CONCLUSION
Insufficient correction of thoracolumbar kyphosis was considered to be a major factor of an unfavorable radiological outcome. The spinal surgeon should consider that having a T-L junction Cobb angle larger than 10.5 degrees immediately after surgery could result in an unfavorable radiological outcome, which is related to a poor clinical outcome.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Akbarnia BA, Crandall DG, Burkus K, Matthews T. Use of long rods and a short arthrodesis for burst fractures of the thoracolumbar spine. a long-term follow-up study. J Bone Joint Surg Am. 76:1629–1635. 1994.
Article2. Alanay A, Acaroglu E, Yazici M, Oznur A, Surat A. Short-segment pedicle instrumentation of thoracolumbar burst fractures: does transpedicular intracorporeal grafting prevent early failure? Spine (Phila Pa 1976). 26:213–217. 2001.3. Albayrak A, Balioglu MB, Misir A, Kargin D, Tacal MT, Atici Y, et al. Preoperative and postoperative photographs and surgical outcomes of patients with kyphosis. Spine (Phila Pa 1976). 41:E1185–E1190. 2016.
Article4. Been HD, Bouma GJ. Comparison of two types of surgery for thoracolumbar burst fractures: combined anterior and posterior stabilisation vs. posterior instrumentation only. Acta Neurochir (Wien). 141:349–357. 1999.
Article5. Briggs AM, van Dieën JH, Wrigley TV, Greig AM, Phillips B, Lo SK, et al. Thoracic kyphosis affects spinal loads and trunk muscle force. Phys Ther. 87:595–607. 2007.
Article6. Bruno AG, Anderson DE, D’Agostino J, Bouxsein ML. The effect of thoracic kyphosis and sagittal plane alignment on vertebral compressive loading. J Bone Miner Res. 27:2144–2151. 2012.
Article7. Buchowski JM, Kuhns CA, Bridwell KH, Lenke LG. Surgical management of posttraumatic thoracolumbar kyphosis. Spine J. 8:666–677. 2008.
Article8. Cahueque M, Cobar A, Zuñiga C, Caldera G. Management of burst fractures in the thoracolumbar spine. J Orthop. 13:278–281. 2016.
Article9. Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976). 17(8 Suppl):S317–S324. 1992.
Article10. Dai LY, Jiang SD, Wang XY, Jiang LS. A review of the management of thoracolumbar burst fractures. Surg Neurol. 67:221–231. discussion 231. 2007.
Article11. Daniaux H, Seykora P, Genelin A, Lang T, Kathrein A. Application of posterior plating and modifications in thoracolumbar spine injuries. Indication, techniques, and results. Spine (Phila Pa 1976). 16(3 Suppl):S125–S133. 1991.12. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 8:817–831. 1983.
Article13. Dobran M, Nasi D, Brunozzi D, di Somma L, Gladi M, Iacoangeli M, et al. Treatment of unstable thoracolumbar junction fractures: short-segment pedicle fixation with inclusion of the fracture level versus long-segment instrumentation. Acta Neurochir (Wien). 158:1883–1889. 2016.
Article14. Ebelke DK, Asher MA, Neff JR, Kraker DP. Survivorship analysis of VSP spine instrumentation in the treatment of thoracolumbar and lumbar burst fractures. Spine (Phila Pa 1976). 16(8 Suppl):S428–S432. 1991.
Article15. Esses SI, Botsford DJ, Kostuik JP. Evaluation of surgical treatment for burst fractures. Spine (Phila Pa 1976). 15:667–673. 1990.
Article16. Esses SI, Botsford DJ, Wright T, Bednar D, Bailey S. Operative treatment of spinal fractures with the AO internal fixator. Spine (Phila Pa 1976). 16(3 Suppl):S146–S150. 1991.
Article17. Gertzbein SD. Scoliosis research society. Multicenter spine fracture study. Spine (Phila Pa 1976). 17:528–540. 1992.18. Gertzbein SD, Court-Brown CM, Marks P, Martin C, Fazl M, Schwartz M, et al. The neurological outcome following surgery for spinal fractures. Spine (Phila Pa 1976). 13:641–644. 1988.
Article19. Greenough CG, Fraser RD. Assessment of outcome in patients with low-back pain. Spine (Phila Pa 1976). 17:36–41. 1992.
Article20. Haas N, Blauth M, Tscherne H. Anterior plating in thoracolumbar spine injuries. indication, technique, and results. Spine (Phila Pa 1976). 16(3 Suppl):S100–S111. 1991.
Article21. Hu R, Mustard CA, Burns C. Epidemiology of incident spinal fracture in a complete population. Spine (Phila Pa 1976). 21:492–499. 1996.
Article22. Josten C, Schmidt C, Spiegl U. Osteoporotic vertebral body fractures of the thoracolumbar spine. Diagnostics and therapeutic strategies. Chirurg. 83:866–874. 2012.23. Khoueir P, Oh BC, Wang MY. Delayed posttraumatic thoracolumbar spinal deformities: diagnosis and management. Neurosurgery. 63(3 Suppl):117–124. 2008.24. Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 6:479–487. 2006.
Article25. Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 34:535–546. 2011.
Article26. Knop C, Fabian HF, Bastian L, Blauth M. Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine (Phila Pa 1976). 26:88–99. 2001.
Article27. Kraemer WJ, Schemitsch EH, Lever J, McBroom RJ, McKee MD, Waddell JP. Functional outcome of thoracolumbar burst fractures without neurological deficit. J Orthop Trauma. 10:541–544. 1996.
Article28. Lindsey RW, Dick W. The fixateur interne in the reduction and stabilization of thoracolumbar spine fractures in patients with neurologic deficit. Spine (Phila Pa 1976). 16(3 Suppl):S140–S145. 1991.
Article29. McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am. 75:162–167. 1993.
Article30. Mermelstein LE, McLain RF, Yerby SA. Reinforcement of thoracolumbar burst fractures with calcium phosphate cement. A biomechanical study. Spine (Phila Pa 1976). 23:664–670. discussion 670-671. 1998.
Article31. Müller U, Berlemann U, Sledge J, Schwarzenbach O. Treatment of thoracolumbar burst fractures without neurologic deficit by indirect reduction and posterior instrumentation: bisegmental stabilization with monosegmental fusion. Eur Spine J. 8:284–289. 1999.
Article32. Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful shortsegment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine (Phila Pa 1976). 25:1157–1170. 2000.
Article33. Paxinos O, Tsitsopoulos PP, Zindrick MR, Voronov LI, Lorenz MA, Havey RM, et al. Evaluation of pullout strength and failure mechanism of posterior instrumentation in normal and osteopenic thoracic vertebrae. J Neurosurg Spine. 13:469–476. 2010.
Article34. Rojas-Tomba F, Hernández-Ruiz Á, Menéndez-Quintanilla I, García de Quevedo-Puerta D, Moriel-Durán J, Villanueva-Pareja F. Radiologic and functional outcomes in unstable thoracolumbar fractures treated with short-segment pedicle instrumentation. Clin Spine Surg. 30:459–465. 2017.
Article35. Schulz R, Melcher RP, Garib MC, Schulz H, Weissman K, Harms J. Does kyphotic deformity correlate with functional outcomes in fractures at the thoracolumbar junction treated by 360° instrumented fusion? Eur J Orthop Surg Traumatol. 24 Suppl 1:s93–s101. 2014.
Article36. Song KS, Chang BS, Yeom JS, Lee JH, Park KW, Lee CK. Surgical treatment of severe angular kyphosis with myelopathy: anterior and posterior approach with pedicle screw instrumentation. Spine (Phila Pa 1976). 33:1229–1235. 2008.37. Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 18:485–488. 2005.38. Tropiano P, Huang RC, Louis CA, Poitout DG, Louis RP. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine (Phila Pa 1976). 28:2459–2465. 2003.
Article39. Vaccaro AR, Silber JS. Post-traumatic spinal deformity. Spine (Phila Pa 1976). 26(24 Suppl):S111–S118. 2001.
Article40. Vaccaro AR, Kim DH, Brodke DS, Harris M, Chapman JR, Schildhauer T, et al. Diagnosis and management of thoracolumbar spine fractures. Instr Course Lect. 53:359–373. 2004.
Article41. Wang XB, Lü GH, Li J, Wang B, Lu C, Phan K. Posterior distraction and instrumentation cannot always reduce displaced and rotated posterosuperior fracture fragments in thoracolumbar burst fracture. Clin Spine Surg. 30:E317–E322. 2017.
Article42. Wood KB, Buttermann GR, Phukan R, Harrod CC, Mehbod A, Shannon B, et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective randomized study with follow-up at sixteen to twenty-two years. J Bone Joint Surg Am. 97:3–9. 2015.
Article43. Xu BS, Tang TS, Yang HL. Long-term results of thoracolumbar and lumbar burst fractures after short-segment pedicle instrumentation, with special reference to implant failure and correction loss. Orthop Surg. 1:85–93. 2009.
Article44. Zeng Y, Chen Z, Sun C, Li W, Qi Q, Guo Z, et al. Posterior surgical correction of posttraumatic kyphosis of the thoracolumbar segment. J Spinal Disord Tech. 26:37–41. 2013.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Posterior Fixation Alone and Supplementation with Posterolateral Fusion in Thoracolumbar Burst Fractures
- Treatment of Unstable Fracture of the Thoracolumbar Spine Using Kaneda Instrumentation
- Comparative Study of Radiologic Changes after Conservative Treatment in Compression fracture and Stable Bursting Fracture of Thoracolumbar Spine
- Results of Staged 360-Degree Spinal Fusion for Unstable Thoracolumbar Burst Fracture
- Significance of Anterior Support in Thoracolumbar Burst Fracture: Single Stage Interbody Fusion with Transpedicular Screw Fixation Versus Pedicle Screw Fixation with Lamina Onlay Fusion