Korean J Ophthalmol.
2019 Feb;33(1):63-69. 10.3341/kjo.2018.0032.
Effect of Serous Retinal Detachment on the Measurement of Axial Length in Central Serous Chorioretinopathy
- Affiliations
-
- 1Department of Ophthalmology, Chungnam National University College of Medicine, Daejeon, Korea. kimjy@cnu.ac.kr
- KMID: 2434306
- DOI: http://doi.org/10.3341/kjo.2018.0032
Abstract
- PURPOSE
To evaluate the changes of axial length (AXL) in eyes with unilateral idiopathic central serous chorioretinopathy (CSC) after resolution of serous retinal detachment.
METHODS
A total of 31 patients diagnosed with idiopathic unilateral CSC were included in this study. The changes of AXL according to serous retinal detachment were examined. The keratometric value and AXL were measured using partial coherence interferometry. Serous retinal detachment and central macular thickness (CMT) were measured by spectral domain optical coherence tomography.
RESULTS
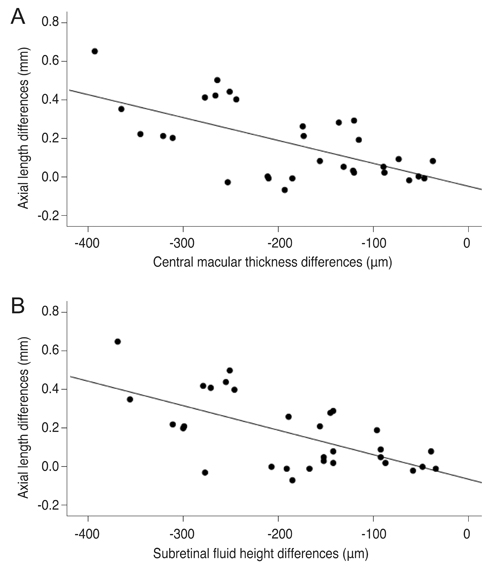
The mean age of the 31 CSC patients, including 19 males, was 42.7 years. The AXL was significantly increased from 23.41 to 23.58 mm after resolution of serous retinal detachment (p < 0.001). The CMT was significantly decreased from 413.4 to 226.8 µm after resolution of serous retinal detachment (p < 0.001). The differences in AXL correlated with CMT differences and subretinal fluid height (r = −0.616, p < 0.001 and r = −0.637, p < 0.001, respectively), and the best-corrected visual acuity was significantly different after resolution of serous retinal detachment (p < 0.001).
CONCLUSIONS
In unilateral idiopathic CSC with serous retinal detachment, a shortened AXL in the acute phase was restored after resolution of serous retinal detachment.
Keyword
MeSH Terms
Figure
Reference
-
1. Hirnschall N, Leisser C, Radda S, et al. Macular disease detection with a swept-source optical coherence tomography-based biometry device in patients scheduled for cataract surgery. J Cataract Refract Surg. 2016; 42:530–536.
Article2. Kovacs I, Ferencz M, Nemes J, et al. Intraocular lens power calculation for combined cataract surgery, vitrectomy and peeling of epiretinal membranes for macular oedema. Acta Ophthalmol Scand. 2007; 85:88–91.3. Ueda T, Nawa Y, Hara Y. Relationship between the retinal thickness of the macula and the difference in axial length. Graefes Arch Clin Exp Ophthalmol. 2006; 244:498–501.
Article4. Binkhorst RD. The accuracy of ultrasonic measurement of the axial length of the eye. Ophthalmic Surg. 1981; 12:363–365.
Article5. Giers U, Epple C. Comparison of a-scan device accuracy. J Cataract Refract Surg. 1990; 16:235–242.
Article6. Olsen T. The accuracy of ultrasonic determination of axial length in pseudophakic eyes. Acta Ophthalmol (Copenh). 1989; 67:141–144.
Article7. Drexler W, Findl O, Menapace R, et al. Partial coherence interferometry: a novel approach to biometry in cataract surgery. Am J Ophthalmol. 1998; 126:524–534.
Article8. Tehrani M, Krummenauer F, Kumar R, Dick HB. Comparison of biometric measurements using partial coherence interferometry and applanation ultrasound. J Cataract Refract Surg. 2003; 29:747–752.
Article9. Vogel A, Dick HB, Krummenauer F. Reproducibility of optical biometry using partial coherence interferometry: intraobserver and interobserver reliability. J Cataract Refract Surg. 2001; 27:1961–1968.
Article10. Liew G, Quin G, Gillies M, Fraser-Bell S. Central serous chorioretinopathy: a review of epidemiology and pathophysiology. Clin Exp Ophthalmol. 2013; 41:201–214.
Article11. Nicholson B, Noble J, Forooghian F, Meyerle C. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol. 2013; 58:103–126.
Article12. Schatz H. Central serous chorioretinopathy and serous detachment of the retinal pigment epithelium. Int Ophthalmol Clin. 1975; 15:159–168.
Article13. Olsen T. Sources of error in intraocular lens power calculation. J Cataract Refract Surg. 1992; 18:125–129.
Article14. Olsen T. Prediction of the effective postoperative (intraocular lens) anterior chamber depth. J Cataract Refract Surg. 2006; 32:419–424.
Article15. Connors R 3rd, Boseman P 3rd, Olson RJ. Accuracy and reproducibility of biometry using partial coherence interferometry. J Cataract Refract Surg. 2002; 28:235–238.
Article16. Eleftheriadis H. IOLMaster biometry: refractive results of 100 consecutive cases. Br J Ophthalmol. 2003; 87:960–963.
Article17. Rose LT, Moshegov CN. Comparison of the Zeiss IOLMaster and applanation A-scan ultrasound: biometry for intraocular lens calculation. Clin Exp Ophthalmol. 2003; 31:121–124.
Article18. Packer M, Fine IH, Hoffman RS, et al. Immersion A-scan compared with partial coherence interferometry: outcomes analysis. J Cataract Refract Surg. 2002; 28:239–242.19. Attas-Fox L, Zadok D, Gerber Y, et al. Axial length measurement in eyes with diabetic macular edema: a-scan ultrasound versus IOLMaster. Ophthalmology. 2007; 114:1499–1504.20. Lege BA, Haigis W. Laser interference biometry versus ultrasound biometry in certain clinical conditions. Graefes Arch Clin Exp Ophthalmol. 2004; 242:8–12.
Article21. Moon H, Lee DY, Nam DH. Axial length in unilateral idiopathic central serous chorioretinopathy. Int J Ophthalmol. 2016; 9:717–720.
Article22. Oh JH, Oh J, Togloom A, et al. Biometric characteristics of eyes with central serous chorioretinopathy. Invest Ophthalmol Vis Sci. 2014; 55:1502–1508.
Article23. Mayer CF, Ardjomand N, Wackernagel W, Velikay-Parel M. Misleading axial length measurements with the IOLMaster due to a dense posterior vitreous surface membrane and a macular edema in a diabetic patient. Graefes Arch Clin Exp Ophthalmol. 2013; 251:387–389.
Article24. Rahman R, Bong CX, Stephenson J. Accuracy of intraocular lens power estimation in eyes having phacovitrectomy for rhegmatogenous retinal detachment. Retina. 2014; 34:1415–1420.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Atypical Central Serous Chorioretinopathy with Bullous Retinal Detachment
- Measurement and Analysis of Neurosensory Retinal Detachment in Central Serous Chorioretinopathy Using Heidelberg Retina Tomograph
- Central Serous Chorioretinopathy in a Patient with Retinal Macrovessel
- A Case of Central Serous Chorioretinopathy with Bullous Retinal Detachment
- A Case of Atypical Idiopathic Central Serous Chorioretinopathy