Ann Surg Treat Res.
2019 Feb;96(2):86-94. 10.4174/astr.2019.96.2.86.
Oncologic evaluation of obesity as a factor in patients with rectal cancer undergoing laparoscopic surgery: a propensity-matched analysis using body mass index
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea. kdw@snubh.org
- 2Department of Surgery, The Catholic University of Korea, Uijeongbu St. Mary's Hospital, Uijeongbu, Korea.
- 3Seoul National University Hospital Gangnam Center, Seoul, Korea.
- 4Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 5Medical Research Collaborating Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- 6Department of Radiation Oncology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 2433945
- DOI: http://doi.org/10.4174/astr.2019.96.2.86
Abstract
- PURPOSE
This study evaluated the oncologic impact of obesity, as determined by body mass index (BMI), in patients who underwent laparoscopic surgery for rectal cancer.
METHODS
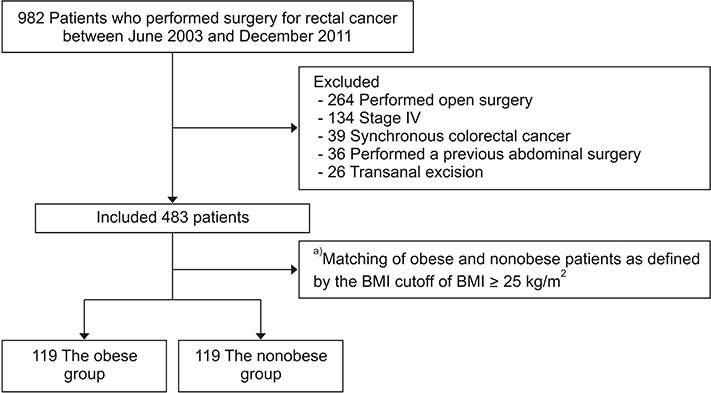
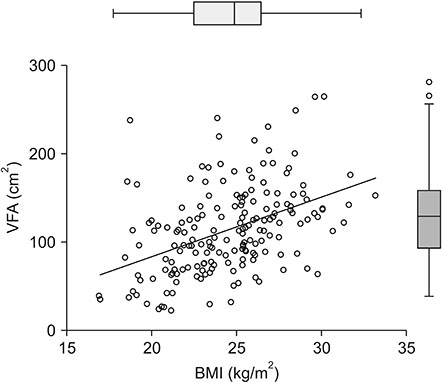
The records of 483 patients with stage I-III rectal cancer who underwent laparoscopic surgery between June 2003 and December 2011 were reviewed. A matching model based on BMI was constructed to balance obese and nonobese patients. Cox hazard regression models for overall survival (OS) and disease-free survival (DFS) were used for multivariate analyses. Additional analysis using visceral fat area (VFA) measurement was performed for matched patients. The threshold for obesity was BMI ≥ 25 kg/m2 or VFA ≥ 130 cm2.
RESULTS
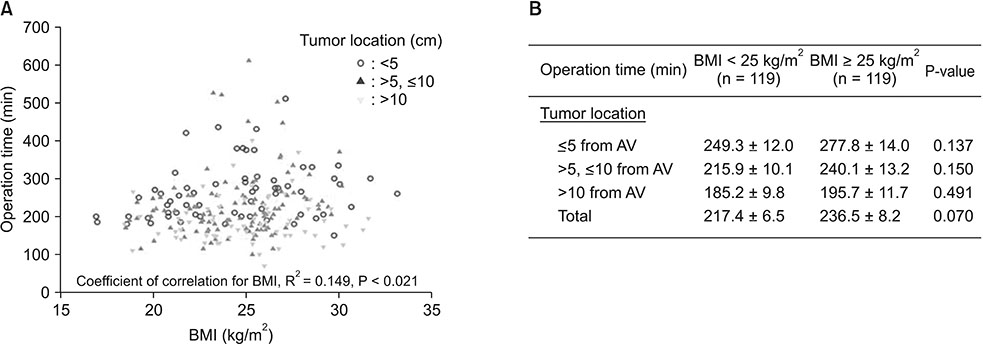
The score matching model yielded 119 patients with a BMI ≥ 25 kg/m2 (the obese group) and 119 patients with a BMI < 25 kg/m2 (the nonobese group). Surgical outcomes including operation time, estimated blood loss, nil per os periods, and length of hospital stay did not differ between the obese and the nonobese group. The retrieved lymph node numbers and pathologic CRM positive rate were also similar in between the 2 groups. After a median follow-up of 48 months (range, 3-126 months), OS and DFS rates were similar between the 2 groups. A tumor location-adjusted model for overall surgical complications showed that a BMI ≥ 25 kg/m2 were not risk factors. Multivariable analyses for OS and DFS showed no significant association with a BMI ≥ 25 kg/m2.
CONCLUSION
Obesity was not associated with long-term oncologic outcomes in patients undergoing laparoscopic surgery for rectal cancer in the Asian population.
Keyword
MeSH Terms
Figure
Reference
-
1. STARSurg Collaborative. Multicentre prospective cohort study of body mass index and postoperative complications following gastrointestinal surgery. Br J Surg. 2016; 103:1157–1172.2. Bouchard C, Despres JP, Mauriege P. Genetic and nongenetic determinants of regional fat distribution. Endocr Rev. 1993; 14:72–93.
Article3. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003; 348:1625–1638.
Article4. Watanabe J, Tatsumi K, Ota M, Suwa Y, Suzuki S, Watanabe A, et al. The impact of visceral obesity on surgical outcomes of laparoscopic surgery for colon cancer. Int J Colorectal Dis. 2014; 29:343–351.
Article5. Moon HG, Ju YT, Jeong CY, Jung EJ, Lee YJ, Hong SC, et al. Visceral obesity may affect oncologic outcome in patients with colorectal cancer. Ann Surg Oncol. 2008; 15:1918–1922.
Article6. Nakamura T, Miura H, Ikeda A, Sato T, Naito M, Ogura N, et al. Laparoscopic surgery for obese patients with colon cancer: a case-matched control study. Surg Today. 2013; 43:763–768.7. Makino T, Trencheva K, Shukla PJ, Rubino F, Zhuo C, Pavoor RS, et al. The influence of obesity on short- and long-term outcomes after laparoscopic surgery for colon cancer: a case-matched study of 152 patients. Surgery. 2014; 156:661–668.
Article8. Ishii Y, Hasegawa H, Nishibori H, Watanabe M, Kitajima M. Impact of visceral obesity on surgical outcome after laparoscopic surgery for rectal cancer. Br J Surg. 2005; 92:1261–1262.
Article9. Seki Y, Ohue M, Sekimoto M, Takiguchi S, Takemasa I, Ikeda M, et al. Evaluation of the technical difficulty performing laparoscopic resection of a rectosigmoid carcinoma: visceral fat reflects technical difficulty more accurately than body mass index. Surg Endosc. 2007; 21:929–934.
Article10. Ballian N, Yamane B, Leverson G, Harms B, Heise CP, Foley EF, et al. Body mass index does not affect postoperative morbidity and oncologic outcomes of total mesorectal excision for rectal adenocarcinoma. Ann Surg Oncol. 2010; 17:1606–1613.
Article11. Aytac E, Lavery IC, Kalady MF, Kiran RP. Impact of obesity on operation performed, complications, and long-term outcomes in terms of restoration of intestinal continuity for patients with mid and low rectal cancer. Dis Colon Rectum. 2013; 56:689–697.
Article12. Seishima R, Okabayashi K, Hasegawa H, Sugiyama D, Ishii Y, Tsuruta M, et al. Obesity was associated with a decreased postoperative recurrence of rectal cancer in a Japanese population. Surg Today. 2014; 44:2324–2331.
Article13. Chen B, Zhang Y, Zhao S, Yang T, Wu Q, Jin C, et al. The impact of general/visceral obesity on completion of mesorectum and perioperative outcomes of laparoscopic TME for rectal cancer: a STARD-compliant article. Medicine (Baltimore). 2016; 95:e4462.14. Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011; 364:719–729.15. Examination Committee of Criteria for ‘Obesity Disease’ in Japan. Japan Society for the Study of Obesity. New criteria for ‘obesity disease’ in Japan. Circ J. 2002; 66:987–992.16. Kang J, Baek SE, Kim T, Hur H, Min BS, Lim JS, et al. Impact of fat obesity on laparoscopic total mesorectal excision: more reliable indicator than body mass index. Int J Colorectal Dis. 2012; 27:497–505.
Article17. Kang SB, Park JS, Kim DW, Lee TG. Intraoperative technical difficulty during laparoscopy-assisted surgery as a prognostic factor for colorectal cancer. Dis Colon Rectum. 2010; 53:1400–1408.
Article18. Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010; 11:637–645.
Article19. Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008; 26:303–312.
Article20. Delaney CP, Pokala N, Senagore AJ, Casillas S, Kiran RP, Brady KM, et al. Is laparoscopic colectomy applicable to patients with body mass index >30? A case-matched comparative study with open colectomy. Dis Colon Rectum. 2005; 48:975–981.21. Chern H, Chou J, Donkor C, Shia J, Guillem JG, Nash GM, et al. Effects of obesity in rectal cancer surgery. J Am Coll Surg. 2010; 211:55–60.
Article22. Min YW, Kim SA, Lee JH, Kim JY, Chang DK, Rhee PL, et al. Overweight is associated with a favorable survival in patients with colorectal cancer: a prospective cohort study in an Asian population. Ann Surg Oncol. 2012; 19:3460–3464.
Article23. Mullen JT, Davenport DL, Hutter MM, Hosokawa PW, Henderson WG, Khuri SF, et al. Impact of body mass index on perioperative outcomes in patients undergoing major intra-abdominal cancer surgery. Ann Surg Oncol. 2008; 15:2164–2172.
Article24. Inui A. Cancer anorexia-cachexia syndrome: current issues in research and management. CA Cancer J Clin. 2002; 52:72–91.
Article25. Meyerhardt JA, Tepper JE, Niedzwiecki D, Hollis DR, McCollum AD, Brady D, et al. Impact of body mass index on outcomes and treatment-related toxicity in patients with stage II and III rectal cancer: findings from Intergroup Trial 0114. J Clin Oncol. 2004; 22:648–657.
Article26. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.27. Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014; 63(25 Pt B):2985–3023.28. Jee SH, Sull JW, Park J, Lee SY, Ohrr H, Guallar E, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006; 355:779–787.
Article29. Kim MK, Lee WY, Kang JH, Kang JH, Kim BT, Kim SM, et al. 2014 clinical practice guidelines for overweight and obesity in Korea. Endocrinol Metab (Seoul). 2014; 29:405–409.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the quality of total mesorectal excision after robotic and laparoscopic surgery for rectal cancer: a multicenter, propensity score-matched study
- Laparoscopic Surgery for Rectal Cancer
- The Impacts of Obesity on a Laparoscopic Low Anterior Resection
- Long-term Oncologic Outcomes of Obesity after Laparoscopic Surgery for Colorectal Cancer in Asian Patients
- The Role of Robotic Surgery for Rectal Cancer: Overcoming Technical Challenges in Laparoscopic Surgery by Advanced Techniques