J Dent Rehabil Appl Sci.
2018 Dec;34(4):280-289. 10.14368/jdras.2018.34.4.280.
Influence of crown-to-implant ratio of short vs long implants on implant stability and marginal bone loss in the mandibular single molar implant
- Affiliations
-
- 1Department of Prosthodontics and Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Republic of Korea. limdds@snu.ac.kr
- 2Dental Life Science Research Institute and Clinical Translational Research Center for Dental Science, Seoul National University Dental Hospital, Seoul, Republic of Korea.
- KMID: 2432364
- DOI: http://doi.org/10.14368/jdras.2018.34.4.280
Abstract
- PURPOSE
The purpose of this randomized clinical trial is to determine whether implant length and the crown-to-implant (C/I) ratio influence implant stability and peri-implant marginal bone loss (MBL).
MATERIALS AND METHODS
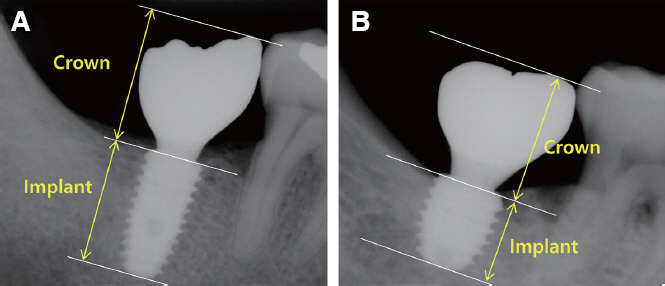
46 patients with single tooth missing in the posterior molar region of the mandible were included in this study. 19 implants (CMI IS-III active® long implant) of 5.0 mm diameter and 10 mm length were installed for the control group, while 27 implants (CMI IS-III active® short implant) of 5.5 mm diameter and 6.6, 7.3 or 8.5 mm length were placed for the experimental group. Each implant was inserted and immediately loaded using the digitally pre-fabricated surgical template and provisional restoration. The CAD-CAM monolithic zirconia crown was fabricated at 3 months after the surgery as a definitive restoration. The ISQ value and the MBL was measured at 48 weeks after the surgery. The correlation between the C/I ratio, MBL, and secondary implant stability was analyzed.
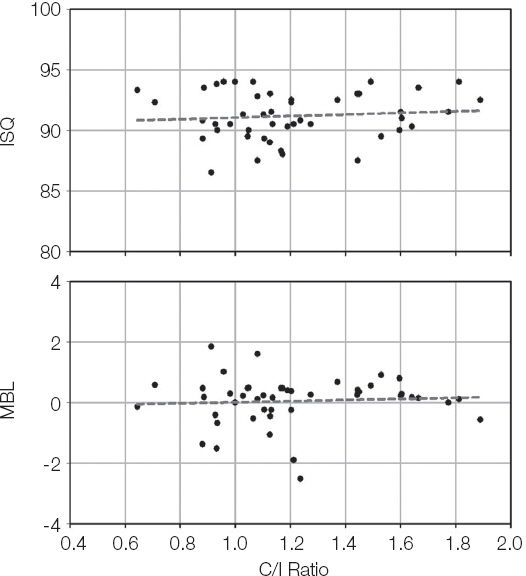
RESULTS
Successful results in terms of ISQ and MBL were achieved with both groups. There was no significant difference between the groups in terms of ISQ values and MBL at 48 weeks after the surgery (P > 0.05). No significant correlation was found between the C/I ratio and secondary stability as well as the C/I ratio and the MBL (P > 0.05).
CONCLUSION
The influence of C/I ratio in both groups was not shown on the stability nor the marginal bone loss in implants supporting single crown of the mandible. Short implant could be a preferable alternative option in the reduced bone height mandible under the limited condition despite its higher C/I ratio.
Keyword
Figure
Reference
-
References
1. Urban IA, Jovanovic SA, Lozada JL. Vertical ridge augmentation using guided bone regeneration (GBR) in three clinical scenarios prior to implant placement: a retrospective study of 35 patients 12 to 72 months after loading. Int J Oral Maxillofac Implants. 2009; 24:502–10. PMID: 19587874.2. Bahat O. Brånemark system implants in the posterior maxilla: clinical study of 660 implants followed for 5 to 12 years. Int J Oral Maxillofac Implants. 2000; 15:646–53. PMID: 11055131.3. Herrmann I, Lekholm U, Holm S, Kultje C. Evaluation of patient and implant characteristics as potential prognostic factors for oral implant failures. Int J Oral Maxillofac Implants. 2005; 20:220–30. PMID: 15839115.4. Naert I, Koutsikakis G, Duyck J, Quirynen M, Jacobs R, van Steenberghe D. Biologic outcome of implant-supported restorations in the treatment of partial edentulism. Part 1: a longitudinal clinical evaluation. Clin Oral Implants Res. 2002; 13:381–9. DOI: 10.1034/j.1600-0501.2002.130406.x. PMID: 12175375.5. Kotsovilis S, Fourmousis I, Karoussis IK, Bamia C. A systematic review and meta-analysis on the effect of implant length on the survival of rough-surface dental implants. J Periodontol. 2009; 80:1700–18. DOI: 10.1902/jop.2009.090107. PMID: 19905941.6. Mangano FG, Shibli JA, Sammons RL, Iaculli F, Piattelli A, Mangano C. Short (8-mm) locking-taper implants supporting single crowns in posterior region: a prospective clinical study with 1-to 10-years of followup. Clin Oral Implants Res. 2014; 25:933–40. DOI: 10.1111/clr.12181. PMID: 23621393.7. Rossi F, Botticelli D, Cesaretti G, De Santis E, Storelli S, Lang NP. Use of short implants (6 mm) in a single-tooth replacement: a 5-year follow-up prospective randomized controlled multicenter clinical study. Clin Oral Implants Res. 2016; 27:458–64. DOI: 10.1111/clr.12564. PMID: 25692556.8. Esposito M, Cannizzaro G, Soardi E, Pellegrino G, Pistilli R, Felice P. A 3-year post-loading report of a randomised controlled trial on the rehabilitation of posterior atrophic mandibles: short implants or longer implants in vertically augmented bone? Eur J Oral Implantol. 2011; 4:301–11. PMID: 22282728.9. Romeo E, Bivio A, Mosca D, Scanferla M, Ghisolfi M, Storelli S. The use of short dental implants in clinical practice: literature review. Minerva Stomatol. 2010; 59:23–31. PMID: 20212407.10. Telleman G, Raghoebar GM, Vissink A, den Hartog L, Huddleston Slater JJ, Meijer HJ. A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. J Clin Periodontol. 2011; 38:667–76. DOI: 10.1111/j.1600-051X.2011.01736.x. PMID: 21564158.11. Grossmann Y, Sadan A. The prosthodontic concept of crown-to-root ratio: a review of the literature. J Prosthet Dent. 2005; 93:559–62. DOI: 10.1016/j.prosdent.2005.03.006. PMID: 15942617.12. Jung RE, Pjetursson BE, Glauser R, Zembic A, Zwahlen M, Lang NP. A systematic review of the 5-year survival and complication rates of implantsupported single crowns. Clin Oral Implants Res. 2008; 19:119–30. DOI: 10.1111/j.1600-0501.2007.01453.x. PMID: 18067597.13. Rosenstiel SF, Land MF, Fujimoto J. Contemporary Fixed Prosthodontics. 4th ed. St. Louis: Elsevier;2006. p. 42–81.14. Schillingburg HT, Hobo S, Whitsett LD, Jacobi R, Brackett SE. Fundamentals of fixed prosthodontics. 3rd ed. Chicago: Quintessence;1997. p. 85–103.15. Pommer B, Heuberer S, Nahler L, Watzek G. How much bone loss can be prevented by alveolar ridge preservation? Systematic literature review and meta-analysis. ImplantNewsPerio. 2012; 9:795–9.16. Simons WF, De Smit M, Duyck J, Coucke W, Quirynen M. The proportion of cancellous bone as predictive factor for early marginal bone loss around implants in the posterior part of the mandible. Clin Oral Implants Res. 2015; 26:1051–9. DOI: 10.1111/clr.12398. PMID: 24750281.17. Weber HP, Crohin CC, Fiorellini JP. A 5-year prospective clinical and radiographic study of nonsubmerged dental implants. Clin Oral Implants Res. 2000; 11:144–53. DOI: 10.1034/j.1600-0501.2000.110207.x.18. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986; 1:11–25. PMID: 3527955.19. Bulaqi HA, Mousavi Mashhadi M, Safari H, Samandari MM, Geramipanah F. Effect of increased crown height on stress distribution in short dental implant components and their surrounding bone: A finite element analysis. J Prosthet Dent. 2015; 113:548–57. DOI: 10.1016/j.prosdent.2014.11.007. PMID: 25794917.20. Toniollo MB, Macedo AP, Rodrigues RC, Ribeiro RF, Mattos Mda G. Three-dimensional finite element analysis of the stress distribution on morse taper implants surface. J Prosthodont Res. 2013; 57:206–12. DOI: 10.1016/j.jpor.2013.02.003. PMID: 23773374.21. Cinar D, Imirzalioglu P. The Effect of Three Different Crown Heights and Two Different Bone Types on Implants Placed in the Posterior Maxilla: Three-Dimensional Finite Element Analysis. Int J Oral Maxillofac Implants. 2016; 31:e1–e10. DOI: 10.11607/jomi.4048. PMID: 27004295.22. Malchiodi L, Cucchi A, Ghensi P, Consonni D, Nocini PF. Influence of crown-implant ratio on implant success rates and crestal bone levels: a 36-month follow-up prospective study. Clin Oral Implants Res. 2014; 25:240–51. DOI: 10.1111/clr.12105. PMID: 23402530.23. Hingsammer L, Watzek G, Pommer B. The influence of crown-to-implant ratio on marginal bone levels around splinted short dental implants: A radiological and clincial short term analysis. Clin Implant Dent Relat Res. 2017; 19:1090–8. DOI: 10.1111/cid.12546. PMID: 29024303.24. Blanes RJ. To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin Oral Implants Res. 2009; 20(Suppl 4):67–72. DOI: 10.1111/j.1600-0501.2009.01762.x. PMID: 19663952.25. Hof M, Pommer B, Zukic N, Vasak C, Lorenzoni M, Zechner W. Influence of prosthetic parameters on peri-implant bone resorption in the first year of loading: a multi-factorial analysis. Clin Implant Dent Relat Res. 2015; 17(Suppl 1):e183–91. DOI: 10.1111/cid.12153. PMID: 24020722.26. Tawil G, Aboujaoude N, Younan R. Influence of prosthetic parameters on the survival and complication rates of short implants. Int J Oral Maxillofac Implants. 2006; 21:275–82. PMID: 16634499.27. Mangano F, Frezzato I, Frezzato A, Veronesi G, Mortellaro C, Mangano C. The Effect of Crownto-Implant Ratio on the Clinical Performance of Extra-Short Locking-Taper Implants. J Craniofac Surg. 2016; 27:675–81. DOI: 10.1097/SCS.0000000000002562. PMID: 27092914.28. Lai HC, Zhuang LF, Zhang ZY. Stability of implants placed in different bone types. Zhonghua Kou Qiang Yi Xue Za Zhi. 2007; 42:292–3. PMID: 17686282.29. Turkyilmaz I, Sennerby L, McGlumphy EA, Tözüm TF. Biomechanical aspects of primary implant stability: a human cadaver study. Clin Implant Dent Relat Res. 2009; 11:113–9. DOI: 10.1111/j.1708-8208.2008.00097.x. PMID: 18422713.30. Östman PO, Hellman M, Wendelhag I, Sennerby L. Resonance frequency analysis measurements of implants at placement surgery. Int J Prosthodont. 2006; 19:77–83. PMID: 16479765.31. Robling AG, Turner CH. Mechanical Signaling for Bone Modeling and Remodeling. Crit Rev Eukaryot Gene Expr. 2009; 19:319–38. DOI: 10.1615/CritRevEukarGeneExpr.v19.i4.50. PMID: 19817708. PMCID: PMC3743123.32. Norton MR. The influence of insertion torque on the survival of immediately placed and restored single-tooth implants. Int J Oral Maxillofac Implants. 2011; 26:1333–43. PMID: 22167441.33. Bornstein MM, Valderrama P, Jones AA, Wilson TG, Seibl R, Cochran DL. Bone apposition around two different sandblasted and acid-etched titanium implant surfaces: a histomorphometric study in canine mandibles. Clin Oral Implants Res. 2008; 19:233–41. DOI: 10.1111/j.1600-0501.2007.01473.x. PMID: 18177427.34. Buser D, Broggini N, Wieland M, Schenk R, Denzer A, Cochran D, Hoffmann B, Lussi A, Steinemann SG. Enhanced bone apposition to a chemically modified SLA titanium surface. J Dent Res. 2004; 83:529–33. DOI: 10.1177/154405910408300704. PMID: 15218041.35. Schwarz F, Herten M, Sager M, Wieland M, Dard M, Becker J. Histological and immunohistochemical analysis of initial and early osseous integration at chemically modified and conventional SLA® titanium implants: preliminary results of a pilot study in dogs. Clin Oral Implants Res. 2007; 18:481–8. DOI: 10.1111/j.1600-0501.2007.01341.x. PMID: 17484737.36. Klokkevold PR, Nishimura RD, Adachi M, Caputo A. Osseointegration enhanced by chemical etching of the titanium surface. A torque removal study in the rabbit. Clin Oral Implants Res. 1997; 8:442–7. DOI: 10.1034/j.1600-0501.1997.080601.x. PMID: 9555202.37. Piattelli A, Manzon L, Scarano A, Paolantonio M, Piattelli M. Histologic and histomorphometric analysis of the bone response to machined and sandblasted titanium implants: an experimental study in rabbits. Int J Oral Maxillofac Implants. 1998; 13:805–10. PMID: 9857591.38. Yeo IS, Han JS, Yang JH. Biomechanical and histomorphometric study of dental implants with different surface characteristics. J Biomed Mater Res B Appl Biomater. 2008; 87:303–11. DOI: 10.1002/jbm.b.31104. PMID: 18435399.39. Kim JH, Yang JY, Kim YK, Heo YK, Yeo IS. Retrospective results of implants for partially edentulous posterior jaws according to time points of early loading. Int J Oral Maxillofac Implants. 2013; 28:1293–9. DOI: 10.11607/jomi.2884. PMID: 24066320.40. Kumar ABT, Khalia N, Gayathri GV, Kumar BHD, Mehta DS. Peri-implant crestal bone preservation: Where do we stand? Int J Oral Implantol Clin Res. 2013; 4:72–7. DOI: 10.5005/JP-Journals-10012-1096.41. Ryu HS, Namgung C, Lee JH, Lim YJ. The influence of thread geometry on implant osseointegration under immediate loading: a literature review. J Adv Prosthodont. 2014; 6:547–54. DOI: 10.4047/jap.2014.6.6.547. PMID: 25551016. PMCID: PMC4279055.42. Langer B, Langer L, Herrmann I, Jorneus L. The wide fixture: a solution for special bone situations and a rescue for the compromised implant. Part 1. Int J Oral Maxillofac Implants. 1993; 8:400–8. PMID: 8270308.43. Renouard F, Arnoux JP, Sarment DP. Five-mmdiameter implants without a smooth surface collar: report on 98 consecutive placements. Int J Oral Maxillofac Implants. 1999; 14:101–7. PMID: 10074759.44. Horwitz J, Zuabi O, Peled M. Resonance frequency analysis in immediate loading of dental implants. Refuat Hapeh Vehashinayim (1993). 2003; 20:80–8. –104. PMID: 14515631.45. Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length, diameter, and geometry on stress distribution: a finite element analysis. Int J Periodontics Restorative Dent. 2010; 30:89–95. PMID: 20224835.46. Baggi L, Di Girolamo M, Vairo G, Sannino G. Comparative Evaluation of Osseointegrated Dental Implants Based on Platform-Switching Concept: Influence of Diameter, Length, Thread Shape, and In-Bone Positioning Depth on Stress-Based Performance. Comput Math Methods Med 2013. 2013; 250929. DOI: 10.1155/2013/250929. PMID: 23861722. PMCID: PMC3703879.47. Simunek A, Strnad J, Kopecka D, Brazda T, Pilathadka S, Chauhan R, Slezak R, Capek L. Changes in stability after healing of immediately loaded dental implants. Int J Oral Maxillofac Implants. 2010; 25:1085–92. PMID: 21197483.48. Dominiak M, Gedrange T. New perspectives in the diagnostic of gingival recession. Adv Clin Exp Med. 2014; 23:857–63. DOI: 10.17219/acem/27907. PMID: 25618109.49. Yazicioglu D, Bayram B, Oguz Y, Cinar D, Uckan S. Stress Distribution on Short Implants at Maxillary Posterior Alveolar Bone Model with Different Bone-to-Implant Contact Ratio: Finite Element Analysis. J Oral Implantol. 2016; 42:26–33. DOI: 10.1563/aaid-doi-D-14-00003. PMID: 26867093.50. Zietek M, Gedrange T, Mikulewicz M. Long term evaluation of biomaterial application in surgical treatment of periodontosis. J Physiol Pharmacol. 2008; 59(Suppl 5):81–6. PMID: 19075328.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of crown-to-implant ratio on periimplant marginal bone loss in the posterior region: a five-year retrospective study
- Effect of the vertical implant position relative to the adjacent cementoenamel junction on peri-implantation bone loss
- Marginal bone level changes in association with different vertical implant positions: a 3-year retrospective study
- The study on success rate of single implant replacing the mandibular first and second molars
- Radiographic evaluation of the proximal bone level between two implants: A 3-year comparative study between Branemark and ITI implants in the mandibular posterior region