Ann Rehabil Med.
2018 Apr;42(2):277-285. 10.5535/arm.2018.42.2.277.
Determinants of Hip and Femoral Deformities in Children With Spastic Cerebral Palsy
- Affiliations
-
- 1Department of Rehabilitation Medicine and Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul, Korea. MEDICUS@yuhs.ac
- KMID: 2432198
- DOI: http://doi.org/10.5535/arm.2018.42.2.277
Abstract
OBJECTIVE
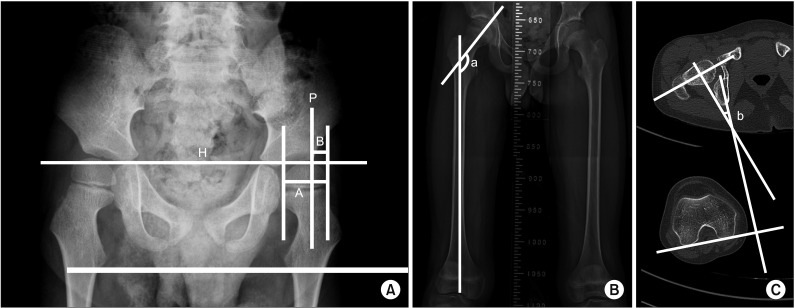
To find factors affecting hip and femoral deformities in children with spastic cerebral palsy (CP) by comparing various clinical findings with imaging studies including plain radiography and computed tomography (CT) imaging.
METHODS
Medical records of 709 children with spastic CP who underwent thorough baseline physical examination and functional assessment between 2 to 6 years old were retrospectively reviewed. Fifty-seven children (31 boys and 26 girls) who had both plain radiography of the hip and three-dimensional CT of the lower extremities at least 5 years after baseline examination were included in this study.
RESULTS
The mean age at physical examination was 3.6 years (SD=1.6; range, 2-5.2 years) and the duration of follow-up imaging after baseline examination was 68.4 months (SD=22.0; range, 60-124 months). The migration percentage correlated with motor impairment and the severity of hip adductor spasticity (R1 angle of hip abduction with knee flexion). The femoral neck and shaft angle correlated with the ambulation ability and severity of hip adductor spasticity (R1 and R2 angles of hip abduction with both knee flexion and extension).
CONCLUSION
Hip subluxation and coxa valga deformity correlated with both dynamic spasticity and shortening of hip adductor muscles. However, we found no correlation between femoral deformities such as femoral anteversion, coxa valga, and hip subluxation.
MeSH Terms
Figure
Reference
-
1. Chang CH, Wang YC, Ho PC, Hwang AW, Kao HK, Lee WC, et al. Determinants of hip displacement in children with cerebral palsy. Clin Orthop Relat Res. 2015; 473:3675–3681. PMID: 26290346.
Article2. Hagglund G, Lauge-Pedersen H, Wagner P. Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskelet Disord. 2007; 8:101. PMID: 17963501.
Article3. Soo B, Howard JJ, Boyd RN, Reid SM, Lanigan A, Wolfe R, et al. Hip displacement in cerebral palsy. J Bone Joint Surg Am. 2006; 88:121–129. PMID: 16391257.
Article4. Miller F. Cerebral palsy. New York: Springer;2005. p. 523–666.5. Sauser DD, Hewes RC, Root L. Hip changes in spastic cerebral palsy. AJR Am J Roentgenol. 1986; 146:1219–1222. PMID: 3486566.
Article6. Choi JY, Jung S, Rha DW, Park ES. Botulinum toxin type a injection for spastic equinovarus foot in children with spastic cerebral palsy: effects on gait and foot pressure distribution. Yonsei Med J. 2016; 57:496–504. PMID: 26847306.
Article7. Moreau M, Cook PC, Ashton B. Adductor and psoas release for subluxation of the hip in children with spastic cerebral palsy. J Pediatr Orthop. 1995; 15:672–676. PMID: 7593584.
Article8. Chung CY, Lee KM, Park MS, Lee SH, Choi IH, Cho TJ. Validity and reliability of measuring femoral anteversion and neck-shaft angle in patients with cerebral palsy. J Bone Joint Surg Am. 2010; 92:1195–1205. PMID: 20439666.
Article9. Gilligan I, Chandraphak S, Mahakkanukrauh P. Femoral neck-shaft angle in humans: variation relating to climate, clothing, lifestyle, sex, age and side. J Anat. 2013; 223:133–151. PMID: 23781912.
Article10. Boese CK, Frink M, Jostmeier J, Haneder S, Dargel J, Eysel P, et al. The modified femoral neck-shaft angle: age- and sex-dependent reference values and reliability analysis. Biomed Res Int. 2016; 2016:8645027. PMID: 28070521.
Article11. Standring S. Gray's anatomy: the anatomical basis of clinical practice. 41th ed. Philadelphia: Elsevier Health Sciences;2015. p. 1376–1382.12. Tardieu G, Shentoub S, Delarue R. Research on a technic for measurement of spasticity. Rev Neurol (Paris). 1954; 91:143–144. PMID: 14358132.13. Boyd RN, Graham HK. Objective measurement of clinical findings in the use of botulinum toxin type A for the management of children with cerebral palsy. Eur J Neurol. 1999; 6(S4):S23–S35.
Article14. Martinsson C, Himmelmann K. Effect of weight-bearing in abduction and extension on hip stability in children with cerebral palsy. Pediatr Phys Ther. 2011; 23:150–157. PMID: 21552077.
Article15. Hoffer MM, Stein GA, Koffman M, Prietto M. Femoral varus-derotation osteotomy in spastic cerebral palsy. J Bone Joint Surg Am. 1985; 67:1229–1235. PMID: 4055848.
Article16. Lee KM, Kang JY, Chung CY, Kwon DG, Lee SH, Choi IH, et al. Clinical relevance of valgus deformity of proximal femur in cerebral palsy. J Pediatr Orthop. 2010; 30:720–725. PMID: 20864860.
Article17. Singh P, Joshua AM, Ganeshan S, Suresh S. Intra-rater reliability of the modified Tardieu scale to quantify spasticity in elbow flexors and ankle plantar flexors in adult stroke subjects. Ann Indian Acad Neurol. 2011; 14:23–26. PMID: 21633610.
Article18. Davids JR, Benfanti P, Blackhurst DW, Allen BL. Assessment of femoral anteversion in children with cerebral palsy: accuracy of the trochanteric prominence angle test. J Pediatr Orthop. 2002; 22:173–178. PMID: 11856924.
Article19. Joseph B. Factors associated with internal hip rotation gait in patients with cerebral palsy. J Pediatr Orthop. 2007; 27:970. PMID: 18209626.20. Robin J, Graham HK, Selber P, Dobson F, Smith K, Baker R. Proximal femoral geometry in cerebral palsy: a population-based cross-sectional study. J Bone Joint Surg Br. 2008; 90:1372–1379. PMID: 18827250.21. Ruwe PA, Gage JR, Ozonoff MB, DeLuca PA. Clinical determination of femoral anteversion. A comparison with established techniques. J Bone Joint Surg Am. 1992; 74:820–830. PMID: 1634572.
Article22. Jiang N, Peng L, Al-Qwbani M, Xie GP, Yang QM, Chai Y, et al. Femoral version, neck-shaft angle, and acetabular anteversion in Chinese Han population: a retrospective analysis of 466 healthy adults. Medicine (Baltimore). 2015; 94:e891. PMID: 26020398.23. Schutte LM, Hayden SW, Gage JR. Lengths of hamstrings and psoas muscles during crouch gait: effects of femoral anteversion. J Orthop Res. 1997; 15:615–621. PMID: 9379273.
Article24. Lamb DW, Pollock GA. Hip deformities in cerebral palsy and their treatment. Dev Med Child Neurol. 1962; 4:488–498. PMID: 13928230.
Article25. Morrell DS, Pearson JM, Sauser DD. Progressive bone and joint abnormalities of the spine and lower extremities in cerebral palsy. Radiographics. 2002; 22:257–268. PMID: 11896216.
Article26. Massaad A, Assi A, Bakouny Z, Sauret C, Khalil N, Skalli W, et al. Three-dimensional evaluation of skeletal deformities of the pelvis and lower limbs in ambulant children with cerebral palsy. Gait Posture. 2016; 49:102–107. PMID: 27395450.
Article27. Howard CB, McKibbin B, Williams LA, Mackie I. Factors affecting the incidence of hip dislocation in cerebral palsy. J Bone Joint Surg Br. 1985; 67:530–532. PMID: 4030844.
Article28. Pountney T, Mandy A, Green E, Gard P. Management of hip dislocation with postural management. Child Care Health Dev. 2002; 28:179–185. PMID: 11952654.
Article29. Pountney TE, Mandy A, Green E, Gard PR. Hip subluxation and dislocation in cerebral palsy - a prospective study on the effectiveness of postural management programmes. Physiother Res Int. 2009; 14:116–127. PMID: 19194957.
Article30. Park ES, Rha DW, Lee WC, Sim EG. The effect of obturator nerve block on hip lateralization in low functioning children with spastic cerebral palsy. Yonsei Med J. 2014; 55:191–196. PMID: 24339306.
Article31. Larnert P, Risto O, Hagglund G, Wagner P. Hip displacement in relation to age and gross motor function in children with cerebral palsy. J Child Orthop. 2014; 8:129–134. PMID: 24595560.
Article32. Himmelmann K, Beckung E, Hagberg G, Uvebrant P. Gross and fine motor function and accompanying impairments in cerebral palsy. Dev Med Child Neurol. 2006; 48:417–423. PMID: 16700930.
Article33. Givon U. Management of the spastic hip in cerebral palsy. Curr Opin Pediatr. 2017; 29:65–69. PMID: 27798427.
Article34. Penner M, Xie WY, Binepal N, Switzer L, Fehlings D. Characteristics of pain in children and youth with cerebral palsy. Pediatrics. 2013; 132:e407–e413. PMID: 23858420.
Article35. Mall V, Heinen F, Siebel A, Bertram C, Hafkemeyer U, Wissel J, et al. Treatment of adductor spasticity with BTX-A in children with CP: a randomized, doubleblind, placebo-controlled study. Dev Med Child Neurol. 2006; 48:10–13. PMID: 16359588.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Analysis on Split Posterior Tibial Tendon Transfers for Spastic Equinovarus Deformity in Cerebral Palsy
- Changes of Kinematic Parameters on Transverse Plane after Orthopaedic Surgery in Children with Spastic Diplegic Cerebral Palsy
- Surgical treatment for adduction contracture of hip in spastic cerebral palsy
- Gait Patterns According to the Transverse Plane Deformities in Spastic Diplegia: A Preliminary Report
- Common Gait Abnormalities of Each Joint in Children with Spastic Cerebral Palsy