Korean Circ J.
2019 Feb;49(2):160-169. 10.4070/kcj.2018.0208.
Long-term Survival in Korean Elderly Patients with Symptomatic Severe Aortic Stenosis Who Refused Aortic Valve Replacement
- Affiliations
-
- 1Department of Cardiology in Internal Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea. jaehpark@cnu.ac.kr
- 2Division of Cardiology, Department of Internal Medicine, Veterans Health Service Medical Center, Seoul, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Daejeon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Daejeon, Korea.
- KMID: 2432133
- DOI: http://doi.org/10.4070/kcj.2018.0208
Abstract
- BACKGROUND AND OBJECTIVES
Aortic valve replacement (AVR) is the treatment of choice in severe symptomatic aortic stenosis (AS) patients. However, a substantial number of elderly patients refuse AVR and treated medically. We investigated their long-term prognosis.
METHODS
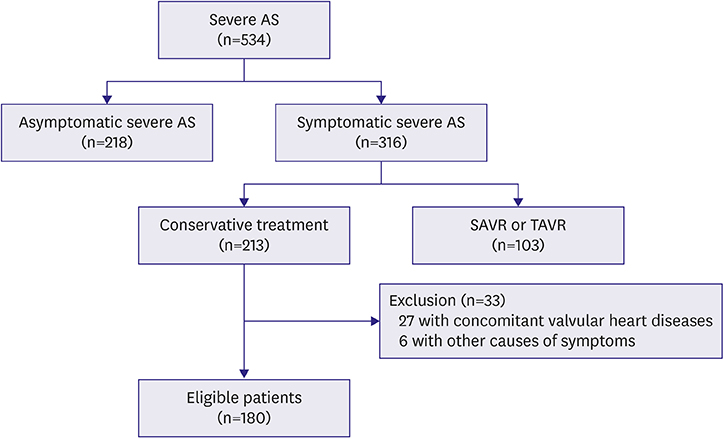
From January 2005 to December 2016, we analyzed elderly patients with severe symptomatic AS who refused to have AVR.
RESULTS
After screening of total 534 patients, we analyzed total 180 severe symptomatic AS patients (78±7 years old, 96 males). Hypertension was the most common cardiovascular risk factor (72%) and the most common symptom was dyspnea (66%). Calculated aortic stenosis area was 0.73±0.20 cm2 and mean left ventricular ejection fraction (LVEF) was 57.8±12.2%. Total 102 patients died during follow-up period (39.1±31.0 months). One-, 3-, and 5-year all-cause mortality rate was 21.1±3.0%, 43.1±3.8%, and 56.5±4.2%, respectively. Of them, 87 died from cardiac causes, and 1-, 3-, and 5-year cardiac mortality rate was 18.0±2.9%, 38.2±3.8%, and 50.7±4.3%, respectively. Their all-cause mortality and cardiac mortality were significantly higher than those of controls. Univariate analysis showed that age, anemia, LVEF, and Log N-terminal pro B-type natriuretic peptide (NT-proBNP) were significant parameters in all-cause mortality (p < 0.001, p=0.001, p=0.039, and p=0.047, respectively) and in cardiac mortality (p < 0.001, p < 0.001, p=0.046, and p=0.026, respectively). Multivariate analysis showed that age and anemia were significant prognostic factors for cardiac and all-cause mortality.
CONCLUSIONS
In elderly severe symptomatic AS patients who treated medically, their 1-, 3- and 5-year all-cause mortality rate was 21.1±3.0%, 43.1±3.8%, and 56.5±4.2%, respectively. Age and anemia were significant prognostic factors for cardiac and all-cause mortality.
Keyword
MeSH Terms
Figure
Reference
-
1. Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006; 368:1005–1011.
Article2. Bach DS, Radeva JI, Birnbaum HG, Fournier AA, Tuttle EG. Prevalence, referral patterns, testing, and surgery in aortic valve disease: leaving women and elderly patients behind? J Heart Valve Dis. 2007; 16:362–369.3. Ross J Jr, Braunwald E. Aortic stenosis. Circulation. 1968; 38:1 Suppl. 61–67.
Article4. Frank S, Johnson A, Ross J Jr. Natural history of valvular aortic stenosis. Br Heart J. 1973; 35:41–46.
Article5. Jang SY, Ju EY, Seo SR, et al. Changes in the etiology of valvular heart disease in the rapidly aging Korean population. Int J Cardiol. 2014; 174:355–359.
Article6. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14.
Article7. Bach DS, Siao D, Girard SE, Duvernoy C, McCallister BD Jr, Gualano SK. Evaluation of patients with severe symptomatic aortic stenosis who do not undergo aortic valve replacement: the potential role of subjectively overestimated operative risk. Circ Cardiovasc Qual Outcomes. 2009; 2:533–539.8. Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010; 363:1597–1607.9. Makkar RR, Fontana GP, Jilaihawi H, et al. Transcatheter aortic-valve replacement for inoperable severe aortic stenosis. N Engl J Med. 2012; 366:1696–1704.
Article10. Ávila-Vanzzini N, Fritche-Salazar JF, Vázquez-Castro NM, et al. Echocardiographic and histologic correlations in patients with severe aortic stenosis: influence of overweight and obesity. J Cardiovasc Ultrasound. 2016; 24:303–311.
Article11. Ng AC, Kong WK, Kamperidis V, et al. Anaemia in patients with aortic stenosis: influence on long-term prognosis. Eur J Heart Fail. 2015; 17:1042–1049.
Article12. Clark MA, Arnold SV, Duhay FG, et al. Five-year clinical and economic outcomes among patients with medically managed severe aortic stenosis: results from a medicare claims analysis. Circ Cardiovasc Qual Outcomes. 2012; 5:697–704.13. Yoon SH, Lefèvre T, Ahn JM, et al. Transcatheter aortic valve replacement with early- and new-generation devices in bicuspid aortic valve stenosis. J Am Coll Cardiol. 2016; 68:1195–1205.14. Yu CW, Kim WJ, Ahn JM, et al. Trends and outcomes of transcatheter aortic valve implantation (TAVI) in Korea: the results of the first cohort of Korean TAVI registry. Korean Circ J. 2018; 48:382–394.
Article15. Shinn SH, Altarabsheh SE, Deo SV, Sabik JH, Markowitz AH, Park SJ. A systemic review and meta-analysis of sutureless aortic valve replacement versus transcatheter aortic valve implantation. Ann Thorac Surg. 2018; 106:924–929.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expanding transcatheter aortic valve replacement into uncharted indications
- Unicommisural Unicuspid Aortic Valve with Very Severe Aortic Stenosis in a 17-Year-Old Female
- Aortic Stenosis and Transcatheter Aortic Valve Implantation: Current Status and Future Directions in Korea
- Aortic Valve Replacement for Aortic Stenosis in Elderly Patients (75 Years or Older)
- Emergency Aortic Valve Replacement for a 95-year-old Patient