Yonsei Med J.
2019 Feb;60(2):216-222. 10.3349/ymj.2019.60.2.216.
Bacterial and Viral Identification Rate in Acute Exacerbation of Chronic Obstructive Pulmonary Disease in Korea
- Affiliations
-
- 1Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea. minkyunghoon@korea.ac.kr
- KMID: 2431639
- DOI: http://doi.org/10.3349/ymj.2019.60.2.216
Abstract
- PURPOSE
The most common cause of acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is respiratory infection. Most studies of bacterial or viral cause in AECOPD have been conducted in Western countries. We investigated bacterial and viral identification rates in AECOPD in Korea.
MATERIALS AND METHODS
We reviewed and analyzed medical records of 736 cases of AECOPD at the Korea University Guro Hospital. We analyzed bacterial and viral identification rates and classified infections according to epidemiological factors, such as Global Initiative for Chronic Obstructive Lung Disease stage, mortality, and seasonal variation.
RESULTS
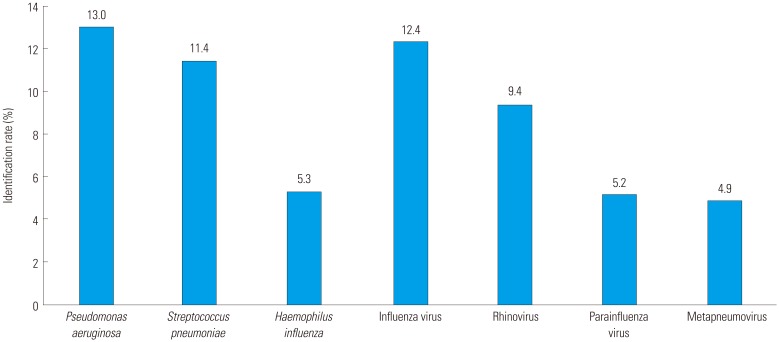
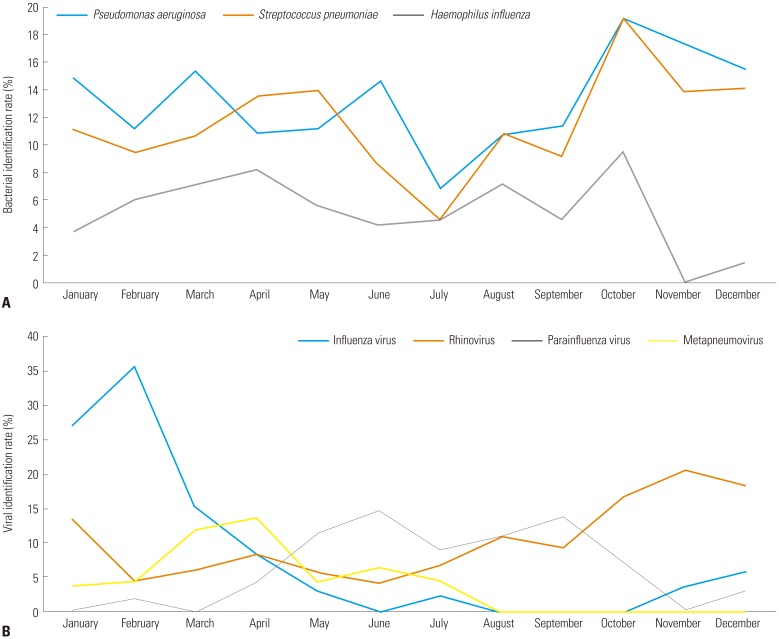
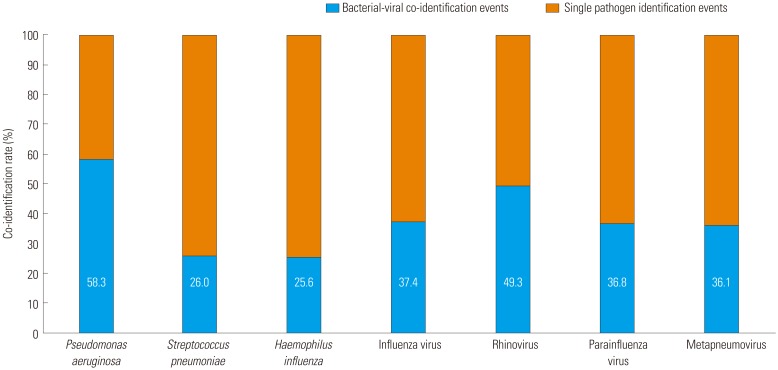
The numbers of AECOPD events involving only bacterial identification, only viral identification, bacterial-viral co-identification, and no identification were 200 (27.2%), 159 (21.6%), 107 (14.5%), and 270 (36.7%), respectively. The most common infectious bacteria identified were Pseudomonas aeruginosa (13.0%), Streptococcus pneumoniae (11.4%), and Haemophilus influenzae (5.3%); the most common viruses identified were influenza virus (12.4%), rhinovirus (9.4%), parainfluenza virus (5.2%), and metapneumovirus (4.9%). The bacterial identification rate tended to be higher at more advanced stages of chronic obstructive pulmonary disease (p=0.020 overall, p=0.011 for P. aeruginosa, p=0.048 for S. pneumoniae). Staphylococcus aureus and Klebsiella pneumoniae were identified more in mortality group (p=0.003 for S. aureus, p=0.009 for K. pneumoniae). All viruses were seasonal (i.e., greater prevalence in a particular season; p < 0.050). Influenza virus and rhinovirus were mainly identified in the winter, parainfluenza virus in the summer, and metapneumovirus in the spring.
CONCLUSION
This information on the epidemiology of respiratory infections in AECOPD will improve the management of AECOPD using antibiotics and other treatments in Korea.
MeSH Terms
-
Anti-Bacterial Agents
Bacteria
Epidemiology
Haemophilus influenzae
Klebsiella pneumoniae
Korea*
Medical Records
Metapneumovirus
Mortality
Orthomyxoviridae
Paramyxoviridae Infections
Prevalence
Pseudomonas aeruginosa
Pulmonary Disease, Chronic Obstructive*
Respiratory Tract Infections
Rhinovirus
Seasons
Staphylococcus aureus
Streptococcus pneumoniae
Anti-Bacterial Agents
Figure
Reference
-
1. Martin P, Glasgow H, Patterson J. Chronic obstructive pulmonary disease (COPD): smoking remains the most important cause. N Z Med J. 2005; 118:U1409. PMID: 15843838.2. Bloemsma LD, Hoek G, Smit LAM. Panel studies of air pollution in patients with COPD: systematic review and meta-analysis. Environ Res. 2016; 151:458–468. PMID: 27565881.
Article3. Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007; 370:786–796. PMID: 17765528.
Article4. Seemungal TA, Hurst JR, Wedzicha JA. Exacerbation rate, health status and mortality in COPD--a review of potential interventions. Int J Chron Obstruct Pulmon Dis. 2009; 4:203–223. PMID: 19554195.5. Spencer S, Calverley PM, Burge PS, Jones PW. Impact of preventing exacerbations on deterioration of health status in COPD. Eur Respir J. 2004; 23:698–702. PMID: 15176682.
Article6. McManus TE, Marley AM, Baxter N, Christie SN, O'Neill HJ, Elborn JS, et al. Respiratory viral infection in exacerbations of COPD. Respir Med. 2008; 102:1575–1580. PMID: 18672353.
Article7. Papi A, Bellettato CM, Braccioni F, Romagnoli M, Casolari P, Caramori G, et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med. 2006; 173:1114–1121. PMID: 16484677.
Article8. De Serres G, Lampron N, La Forge J, Rouleau I, Bourbeau J, Weiss K, et al. Importance of viral and bacterial infections in chronic obstructive pulmonary disease exacerbations. J Clin Virol. 2009; 46:129–133. PMID: 19665425.
Article9. Mohan A, Chandra S, Agarwal D, Guleria R, Broor S, Gaur B, et al. Prevalence of viral infection detected by PCR and RT-PCR in patients with acute exacerbation of COPD: a systematic review. Respirology. 2010; 15:536–542. PMID: 20415983.
Article10. Lin SH, Kuo PH, Hsueh PR, Yang PC, Kuo SH. Sputum bacteriology in hospitalized patients with acute exacerbation of chronic obstructive pulmonary disease in Taiwan with an emphasis on Klebsiella pneumoniae and Pseudomonas aeruginosa. Respirology. 2007; 12:81–87. PMID: 17207030.
Article11. Li XJ, Li Q, Si LY, Yuan QY. Bacteriological differences between COPD exacerbation and community-acquired pneumonia. Respir Care. 2011; 56:1818–1824. PMID: 21605476.
Article12. Chang CH, Tsao KC, Hu HC, Huang CC, Kao KC, Chen NH, et al. Procalcitonin and C-reactive protein cannot differentiate bacterial or viral infection in COPD exacerbation requiring emergency department visits. Int J Chron Obstruct Pulmon Dis. 2015; 10:767–774. PMID: 25926728.
Article13. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007; 176:532–555. PMID: 17507545.14. Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000; 117(5 Suppl 2):398S–401S. PMID: 10843984.
Article15. Sethi S. Infectious etiology of acute exacerbations of chronic bronchitis. Chest. 2000; 117(5 Suppl 2):380S–385S. PMID: 10843981.
Article16. Sethi S, Murphy TF. Bacterial infection in chronic obstructive pulmonary disease in 2000: a state-of-the-art review. Clin Microbiol Rev. 2001; 14:336–363. PMID: 11292642.
Article17. Boixeda R, Almagro P, Díez-Manglano J, Cabrera FJ, Recio J, Martin-Garrido I, et al. Bacterial flora in the sputum and comorbidity in patients with acute exacerbations of COPD. Int J Chron Obstruct Pulmon Dis. 2015; 10:2581–2591. PMID: 26664106.18. Biancardi E, Fennell M, Rawlinson W, Thomas PS. Viruses are frequently present as the infecting agent in acute exacerbations of chronic obstructive pulmonary disease in patients presenting to hospital. Intern Med J. 2016; 46:1160–1165. PMID: 27515577.
Article19. Frickmann H, Jungblut S, Hirche TO, Groß U, Kuhns M, Zautner AE. The influence of virus infections on the course of COPD. Eur J Microbiol Immunol (Bp). 2012; 2:176–185. PMID: 24688763.
Article20. Kwak HJ, Park DW, Kim JE, Park MK, Koo GW, Park TS, et al. Prevalence and risk factors of respiratory viral infections in exacerbations of chronic obstructive pulmonary disease. Tohoku J Exp Med. 2016; 240:131–139. PMID: 27725531.
Article21. Jin J, Yu W, Li S, Lu L, Liu X, Sun Y. Factors associated with bronchiectasis in patients with moderate-severe chronic obstructive pulmonary disease. Medicine (Baltimore). 2016; 95:e4219. PMID: 27442646.
Article22. Gamba-Sanchez N, Rodriguez-Martinez CE, Sossa-Briceño MP. Epidemic activity of respiratory syncytial virus is related to temperature and rainfall in equatorial tropical countries. Epidemiol Infect. 2016; 144:2057–2063. PMID: 26888544.
Article23. Paynter S. Humidity and respiratory virus transmission in tropical and temperate settings. Epidemiol Infect. 2015; 143:1110–1118. PMID: 25307020.
Article24. Goktas S, Sirin MC. Prevalence and seasonal distribution of respiratory viruses during the 2014 - 2015 season in Istanbul. Jundishapur J Microbiol. 2016; 9:e39132. PMID: 27800148.
Article25. Hendricks MR, Lashua LP, Fischer DK, Flitter BA, Eichinger KM, Durbin JE, et al. Respiratory syncytial virus infection enhances Pseudomonas aeruginosa biofilm growth through dysregulation of nutritional immunity. Proc Natl Acad Sci U S A. 2016; 113:1642–1647. PMID: 26729873.26. Bellinghausen C, Gulraiz F, Heinzmann AC, Dentener MA, Savelkoul PH, Wouters EF, et al. Exposure to common respiratory bacteria alters the airway epithelial response to subsequent viral infection. Respir Res. 2016; 17:68. PMID: 27259950.
Article27. Rejman J, Di Gioia S, Bragonzi A, Conese M. Pseudomonas aeruginosa infection destroys the barrier function of lung epithelium and enhances polyplex-mediated transfection. Hum Gene Ther. 2007; 18:642–652. PMID: 17638571.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship between Airway Inflammation and Exacerbation in Chronic Obstructive Pulmonary Disease
- Bacterial etiology of acute exacerbations of chronic obstructive pulmonary disease in hospitalized patients
- The Clinical Study of Clarithromycin for the Treatment of Acute Exacerbation of Chronic Obstructive Pulmonary Disease
- Pulmonary Strongyloidiasis Masquerading as Exacerbation of Chronic Obstructive Pulmonary Disease
- Desaturaton due to Acute Exacerbation of Chronic Obstructive Pulmonary Disease in the Patient Who Underwent the Cephalic Vein Bypass Surgery under Epidural Anesthesia