Ann Dermatol.
2019 Feb;31(1):6-13. 10.5021/ad.2019.31.1.6.
The Important Factors Associated with Treatment Response in Laser Treatment of Facial Scars: A Single-Institution Based Retrospective Study
- Affiliations
-
- 1Department of Dermatology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. bell711@hanmail.net
- 2Statistics and Data Center, Samsung Medical Center, Seoul, Korea.
- 3Department of Mathematics, Ajou University, Suwon, Korea.
- 4Department of Medical Device Management & Research, SAIHST, Sungkyunkwan University, Seoul, Korea.
- KMID: 2430795
- DOI: http://doi.org/10.5021/ad.2019.31.1.6
Abstract
- BACKGROUND
There is increased interest in laser treatment of facial scars.
OBJECTIVE
To determine the factors associated with treatment response.
METHODS
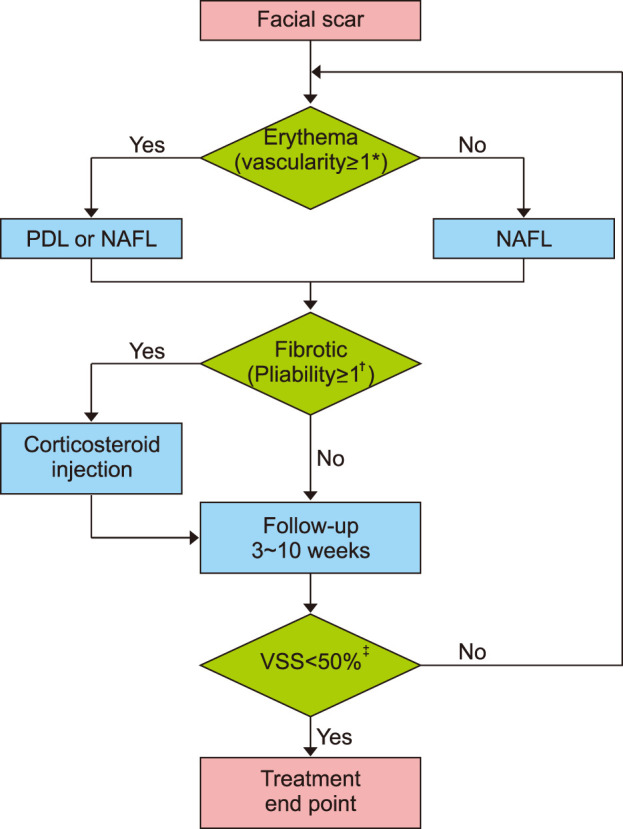
We conducted an institution-based retrospective study by including the patients treated with laser for facial scars from 2012 to 2015. Treatment methods were determined with an algorithm according to individual scar characteristics. In each treatment session, either a 595-nm pulsed-dye laser or a non-ablative fractional laser was used, often in combination with a corticosteroid injection. We evaluated treatment responses based on the number of treatment sessions required to reach the treatment endpoint. Data were analyzed using multinomial logistic regression analysis to examine the association between treatment response and various factors of the scar.
RESULTS
A total of eighty-four scars were analyzed. The onset of treatment (defined as the period between the injury and treatment initiation), used laser modality, and the location of the scar were all found to be significantly associated with treatment responses. Early implementation was more likely to provide better treatment response. Scars on the perioral area were more likely to be associated with worse treatment response.
CONCLUSION
The important factors for the treatment response in facial scars were the location of the scar and the timing of the initiation of treatment. Such information can be used to predict treatment response and tailor the treatment plan to the patient, depending on scar characteristics.
Figure
Reference
-
1. Balaraman B, Geddes ER, Friedman PM. Best reconstructive techniques: improving the final scar. Dermatol Surg. 2015; 41(Suppl 10):S265–S275. PMID: 26418692.2. Bock O, Schmid-Ott G, Malewski P, Mrowietz U. Quality of life of patients with keloid and hypertrophic scarring. Arch Dermatol Res. 2006; 297:433–438. PMID: 16528552.
Article3. Lawrence JW, Mason ST, Schomer K, Klein MB. Epidemiology and impact of scarring after burn injury: a systematic review of the literature. J Burn Care Res. 2012; 33:136–146. PMID: 22138807.4. van Drooge AM, Vrijman C, van der Veen W, Wolkerstorfer A. A randomized controlled pilot study on ablative fractional CO2 laser for consecutive patients presenting with various scar types. Dermatol Surg. 2015; 41:371–377. PMID: 25705952.
Article5. Parry I, Sen S, Palmieri T, Greenhalgh D. Nonsurgical scar management of the face: does early versus late intervention affect outcome? J Burn Care Res. 2013; 34:569–575. PMID: 23816994.6. Gold MH, Berman B, Clementoni MT, Gauglitz GG, Nahai F, Murcia C. Updated international clinical recommendations on scar management: part 1--evaluating the evidence. Dermatol Surg. 2014; 40:817–824. PMID: 25068543.7. Tziotzios C, Profyris C, Sterling J. Cutaneous scarring: pathophysiology, molecular mechanisms, and scar reduction therapeutics part II. Strategies to reduce scar formation after dermatologic procedures. J Am Acad Dermatol. 2012; 66:13–24. quiz 25-26. PMID: 22177632.8. Haedersdal M, Moreau KE, Beyer DM, Nymann P, Alsbjørn B. Fractional nonablative 1540 nm laser resurfacing for thermal burn scars: a randomized controlled trial. Lasers Surg Med. 2009; 41:189–195. PMID: 19291747.
Article9. Vasily DB, Cerino ME, Ziselman EM, Zeina ST. Non-ablative fractional resurfacing of surgical and post-traumatic scars. J Drugs Dermatol. 2009; 8:998–1005. PMID: 19894367.10. Cervelli V, Gentile P, Spallone D, Nicoli F, Verardi S, Petrocelli M, et al. Ultrapulsed fractional CO2 laser for the treatment of post-traumatic and pathological scars. J Drugs Dermatol. 2010; 9:1328–1331. PMID: 21061753.11. Anderson RR, Donelan MB, Hivnor C, Greeson E, Ross EV, Shumaker PR, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014; 150:187–193. PMID: 24336931.12. Vrijman C, van Drooge AM, Limpens J, Bos JD, van der Veen JP, Spuls PI, et al. Laser and intense pulsed light therapy for the treatment of hypertrophic scars: a systematic review. Br J Dermatol. 2011; 165:934–942. PMID: 21711337.
Article13. Verhaeghe E, Ongenae K, Bostoen J, Lambert J. Nonablative fractional laser resurfacing for the treatment of hypertrophic scars: a randomized controlled trial. Dermatol Surg. 2013; 39:426–434. PMID: 23279702.
Article14. Baryza MJ, Baryza GA. The Vancouver scar scale: an administration tool and its interrater reliability. J Burn Care Rehabil. 1995; 16:535–538. PMID: 8537427.
Article15. Park KY, Oh IY, Seo SJ, Kang KH, Park SJ. Appropriate timing for thyroidectomy scar treatment using a 1,550-nm fractional erbium-glass laser. Dermatol Surg. 2013; 39:1827–1834. PMID: 24299574.
Article16. Jung JY, Jeong JJ, Roh HJ, Cho SH, Chung KY, Lee WJ, et al. Early postoperative treatment of thyroidectomy scars using a fractional carbon dioxide laser. Dermatol Surg. 2011; 37:217–223. PMID: 21272120.
Article17. Jin R, Huang X, Li H, Yuan Y, Li B, Cheng C, et al. Laser therapy for prevention and treatment of pathologic excessive scars. Plast Reconstr Surg. 2013; 132:1747–1758. PMID: 24281600.
Article18. Cooper JS, Lee BT. Treatment of facial scarring: lasers, filler, and nonoperative techniques. Facial Plast Surg. 2009; 25:311–315. PMID: 20024872.
Article19. Atiyeh BS. Nonsurgical management of hypertrophic scars: evidence-based therapies, standard practices, and emerging methods. Aesthetic Plast Surg. 2007; 31:468–492. discussion 493-464. PMID: 17576505.
Article20. Ledon JA, Savas J, Franca K, Chacon A, Nouri K. Intralesional treatment for keloids and hypertrophic scars: a review. Dermatol Surg. 2013; 39:1745–1757. PMID: 24299571.
Article21. Kunishige JH, Katz TM, Goldberg LH, Friedman PM. Fractional photothermolysis for the treatment of surgical scars. Dermatol Surg. 2010; 36:538–541. PMID: 20187893.
Article22. Choe JH, Park YL, Kim BJ, Kim MN, Rho NK, Park BS, et al. Prevention of thyroidectomy scar using a new 1,550-nm fractional erbium-glass laser. Dermatol Surg. 2009; 35:1199–1205. PMID: 19175371.
Article23. Kim HS, Lee JH, Park YM, Lee JY. Comparison of the effectiveness of nonablative fractional laser versus ablative fractional laser in thyroidectomy scar prevention: a pilot study. J Cosmet Laser Ther. 2012; 14:89–93. PMID: 22409153.
Article24. Kim SG, Kim EY, Kim YJ, Lee SI. The efficacy and safety of ablative fractional resurfacing using a 2,940-Nm Er:YAG laser for traumatic scars in the early posttraumatic period. Arch Plast Surg. 2012; 39:232–237. PMID: 22783532.
Article25. Gold MH, McGuire M, Mustoe TA, Pusic A, Sachdev M, Waibel J, et al. Updated international clinical recommendations on scar management: part 2--algorithms for scar prevention and treatment. Dermatol Surg. 2014; 40:825–831. PMID: 25068544.26. Chun Q, ZhiYong W, Fei S, XiQiao W. Dynamic biological changes in fibroblasts during hypertrophic scar formation and regression. Int Wound J. 2016; 13:257–262. PMID: 24802644.
Article27. Agha R, Ogawa R, Pietramaggiori G, Orgill DP. A review of the role of mechanical forces in cutaneous wound healing. J Surg Res. 2011; 171:700–708. PMID: 22005503.
Article28. On HR, Lee SH, Lee YS, Chang HS, Park C, Roh MR. Evaluating hypertrophic thyroidectomy scar outcomes after treatment with triamcinolone injections and copper bromide laser therapy. Lasers Surg Med. 2015; 47:479–484. PMID: 26149958.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combination treatment for post-traumatic facial scars: 1,064-nm Nd:YAG picosecond laser with micro-lens array after fractional ablative CO2 laser
- Resurfacing of Pitted Facial Acne Scars with a Pulsed Erbium: YAG laser
- Port-Wine Stains Confined to a Single Cosmetic Unit than on Multiple Cosmetic Units Respond Better to Pulsed Dye Laser Treatment: A Retrospective Study
- Treatment of Facial Scars with CO3 Laser
- Cutaneous Resurfacing of the Pitted Acne Scars with the Erbium:YAG laser in 100 Patients