J Korean Soc Spine Surg.
2018 Dec;25(4):175-179. 10.4184/jkss.2018.25.4.175.
Loss of Disc Height after Spontaneous Regression of a Herniated Lumbar Disc: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Bumin Hospital, Seoul, Korea. esshappy@daum.net
- KMID: 2430143
- DOI: http://doi.org/10.4184/jkss.2018.25.4.175
Abstract
- STUDY DESIGN: Case report.
OBJECTIVES
We report 3 cases of loss of disc height after spontaneous regression of a herniated lumbar disc. SUMMARY OF LITERATURE REVIEW: Reports of spontaneous regression of a herniated lumbar disc were identified.
MATERIALS AND METHODS
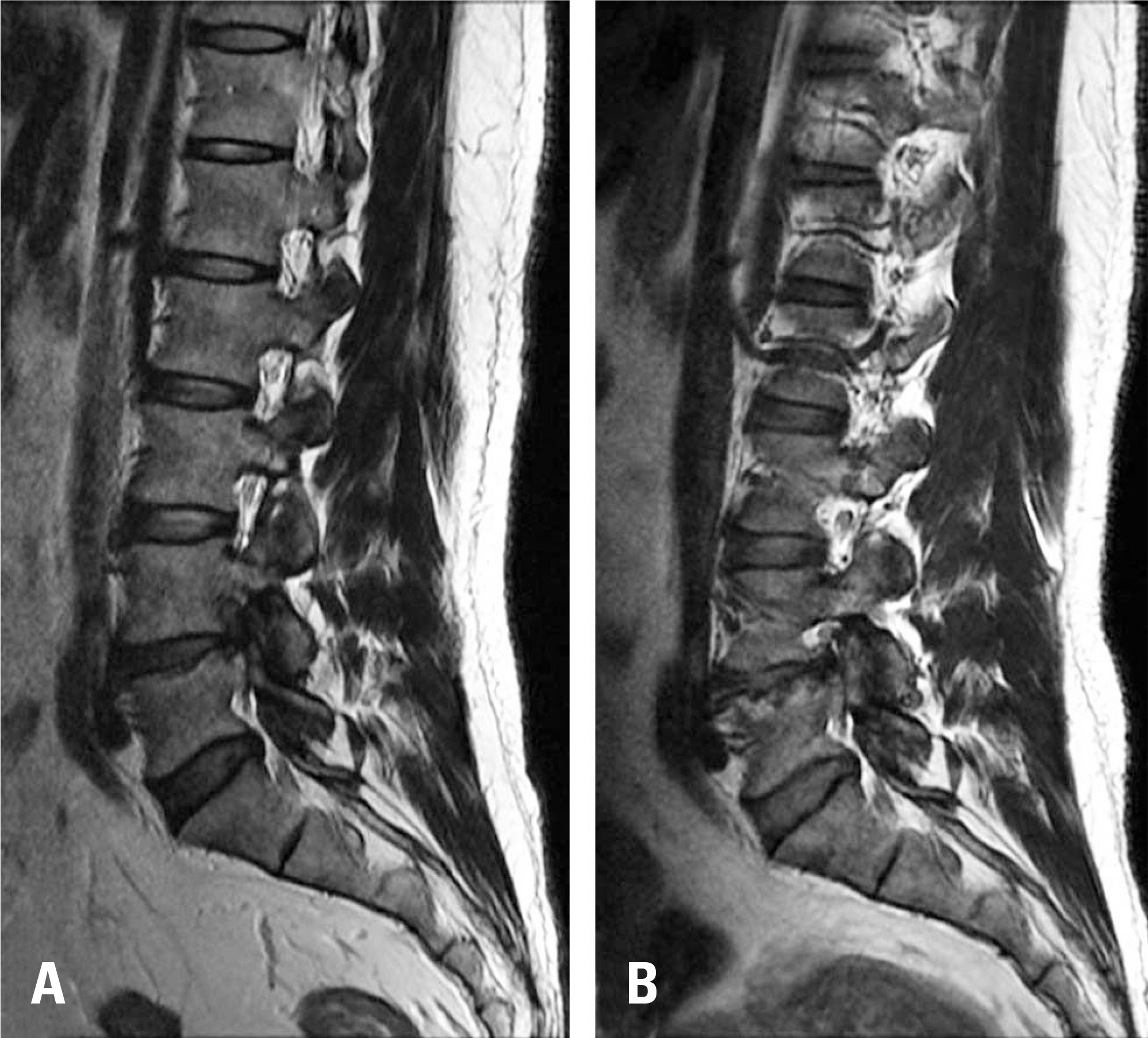
We conservatively treated 3 patients who were diagnosed with a herniated lumbar disc. During outpatient follow-up, radiating pain improved in all patients, but they complained of chronic lower back pain. Magnetic resonance imaging (MRI) was performed for diagnostic purposes.
RESULTS
On MRI, spontaneous regression of the herniated lumbar discs was observed, but loss of disc height was also found.
CONCLUSIONS
A herniated lumbar disc may be a risk factor for loss of disc height. It is important to recognize that a patient with a herniated lumbar disc can struggle with chronic lower back pain even if spontaneous regression of the herniated lumbar disc occurs.
Figure
Reference
-
1. Boden SD, McCowin PR, Davis DO, et al. Abnormal mag-netic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990 Sep; 72(8):1178–84. DOI: 10.2106/00004623-199072080-00008.
Article2. Sabuncuoglu H, Ozdogan S, Timurkaynak E. Spontaneous regression of extruded lumbar disc herniation: report of two illustrative case and review of the literature. Turk Neurosurg. 2008 Oct; 18(4):392–6.3. Guinto FC Jr., Hashim H, Stumer M. CT demonstration of disk regression after conservative therapy. AJNR Am J Neuroradiol. 1984 Sep-Oct; 5(5):632–3.4. Benoist M. The natural history of lumbar disc herniation and radiculopathy. Joint Bone Spine. 2002 Mar; 69(2):155–60. DOI: 10.1016/S1297-319X(02)00385-8.
Article5. Komori H, Shinomiya K, Nakai O, et al. The natural history of herniated nucleus pulposus with radiculopathy. Spine (Phila Pa 1976). 1996 Jan; 21(2):225–9. DOI: 10.1097/00007632-199601150-00013.
Article6. Teplick JG, Haskin ME. Spontaneous regression of herniated nucleus pulposus. AJR Am J Roentgenol. 1985 Aug; 145(2):371–5. DOI: 10.2214/ajr.145.2.371.
Article7. Slavin KV, Raja A, Thornton J, et al. Spontaneous regression of a large lumbar disc herniation: report of an illustrative case. Surg Neurol. 2001 Nov; 56(5):333–6. DOI: 10.1016/S0090-3019 (01)00607-3.8. Henmi T, Sairyo K, Nakano S, et al. Natural history of extruded lumbar intervertebral disc herniation. J Med Invest. 2002 Feb; 49(1-2):40–3.9. Autio RA, Karppinen J, Niinimä ki J, et al. Determinants of spontaneous resorption of intervertebral disc herniations. Spine (Phila Pa 1976). 2006 May; 31(11):1247–52. DOI: 10.1097/01.brs.0000217681.83524.4a.
Article10. Barth M, Diepers M, Weiss C, et al. Two-year outcome after lumbar microdiscectomy versus microscopic seques-trectomy: part 2: radiographic evaluation and correlation with clinical outcome. Spine (Phila Pa 1976). 2008 Feb; 33(3):273–9. DOI: 10.1097/BRS.0b013e31816201a6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Regression of a Large Lumbar Disc Extrusion
- The Spontaneous Resorption of Herniated Lumbar Disc: A case report
- The Change of Intervertebtal Disc Space Height after Discectomy at Long Term Follw-up
- Historical Changes of Extruded Lumbar Intervertebral Disc : A case report
- Comparative study of the intervertebral spaces in the normal and the disc patients