J Periodontal Implant Sci.
2018 Dec;48(6):347-359. 10.5051/jpis.2018.48.6.347.
Periodontal pathogens and the association between periodontitis and rheumatoid arthritis in Korean adults
- Affiliations
-
- 1Department of Periodontology, Seoul National University School of Dentistry, Seoul, Korea. ymlee@snu.ac.kr
- 2Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea.
- 3Department of Molecular Medicine and Biopharmaceutical Sciences, Seoul National University, Seoul, Korea.
- 4Dental Research Institute, Seoul National University School of Dentistry, Seoul, Korea.
- 5Department of Internal Medicine, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2429863
- DOI: http://doi.org/10.5051/jpis.2018.48.6.347
Abstract
- PURPOSE
Periodontitis and rheumatoid arthritis (RA) share a similar inflammatory pathogenesis. Porphyromonas gingivalis (Pg) can induce anticyclic-citrullinated peptide autoantibodies (anti-CCP antibodies), a key factor in the development of RA. This study aimed at evaluating the relationships between the 2 diseases and identifying the clinical implications thereof, with a focus on periodontal pathogens in Korean adults.
METHODS
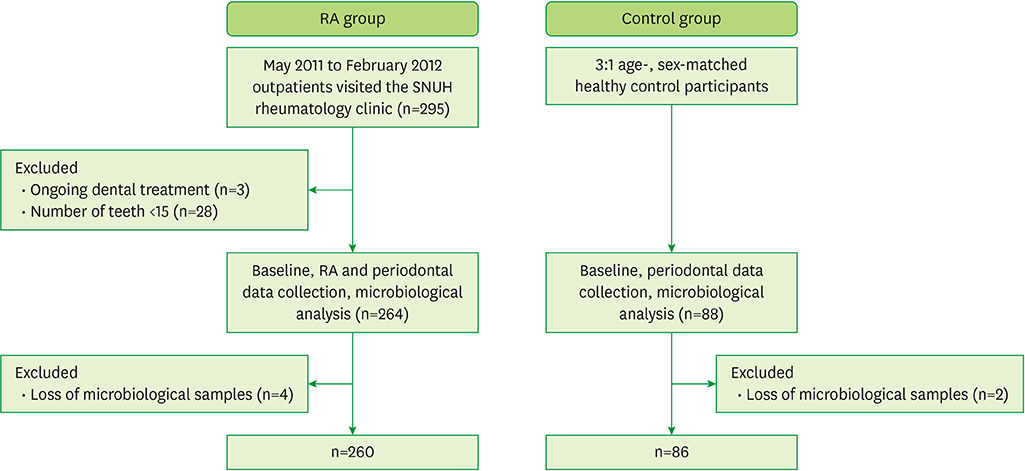
A total of 260 RA patients and 86 age- and sex-matched control patients without arthritis were enrolled in this prospective cross-sectional study. Periodontal indices and the prevalence and amount of periodontal pathogens were compared between the groups. Correlations between periodontal and RA indices were examined, as were correlations between 9 periodontal pathogens and RA indices.
RESULTS
The RA group had significantly higher values than the control group for all investigated periodontal indices (P < 0.05) except the number of teeth. The gingival index (GI) was correlated with the disease activity score 28 (DAS28) (r = 0.125, P = 0.049), RA disease duration (r = 0.253, P < 0.001), erythrocyte sedimentation rate (ESR) (r = 0.162, P = 0.010), and anti-CCP antibody titer (r = 0.205, P = 0.004). Probing pocket depth (PPD) was correlated with ESR (r = 0.139, P = 0.027) and anti-Pg antibody titer (r = 0.203, P = 0.001). Bleeding on probing (BOP) was correlated with DAS28 (r = 0.137, P = 0.030), RA disease duration (r = 0.202, P = 0.001), ESR (r = 0.136, P = 0.030), anti-Pg antibody titer (r = 0.177, P = 0.005), and anti-CCP antibody titer (r = 0.188, P = 0.007). Clinical attachment level (CAL) and periodontitis severity were correlated with anti-Pg antibody titer (the former r = 0.201, P = 0.002; the latter r = 0.175, P = 0.006). The quantity of Pg was positively correlated with the serum anti-Pg antibody titer (r = 0.148, P = 0.020).
CONCLUSIONS
The GI, BOP, and PPD showed positive relationships with several RA indices. The anti-Pg antibody titer had positive relationships with PPD, BOP, CAL, and periodontitis severity. Thus, increasing values of periodontal indices could be used as a risk indicator of disease development in RA patients, and an increasing anti-Pg antibody titer could be considered as a warning sign in RA patients suffering with periodontitis.
MeSH Terms
Figure
Reference
-
1. Page RC, Kornman KS. The pathogenesis of human periodontitis: an introduction. Periodontol 2000. 1997; 14:9–11.
Article2. Armitage GC, Research S. Research, Science and Therapy Committee of the American Academy of Periodontology. Diagnosis of periodontal diseases. J Periodontol. 2003; 74:1237–1247.3. Mercado FB, Marshall RI, Bartold PM. Inter-relationships between rheumatoid arthritis and periodontal disease. A review. J Clin Periodontol. 2003; 30:761–772.
Article4. Rutger Persson G. Rheumatoid arthritis and periodontitis - inflammatory and infectious connections. Review of the literature. J Oral Microbiol. 2012; 4:4.5. Kaur S, White S, Bartold PM. Periodontal disease and rheumatoid arthritis: a systematic review. J Dent Res. 2013; 92:399–408.6. Golub LM, Payne JB, Reinhardt RA, Nieman G. Can systemic diseases co-induce (not just exacerbate) periodontitis? A hypothetical “two-hit” model. J Dent Res. 2006; 85:102–105.
Article7. Rosenstein ED, Greenwald RA, Kushner LJ, Weissmann G. Hypothesis: the humoral immune response to oral bacteria provides a stimulus for the development of rheumatoid arthritis. Inflammation. 2004; 28:311–318.
Article8. Martinez-Martinez RE, Abud-Mendoza C, Patiño-Marin N, Rizo-Rodríguez JC, Little JW, Loyola-Rodríguez JP. Detection of periodontal bacterial DNA in serum and synovial fluid in refractory rheumatoid arthritis patients. J Clin Periodontol. 2009; 36:1004–1010.
Article9. McGraw WT, Potempa J, Farley D, Travis J. Purification, characterization, and sequence analysis of a potential virulence factor from Porphyromonas gingivalis, peptidylarginine deiminase. Infect Immun. 1999; 67:3248–3256.
Article10. Bartold PM, Marshall RI, Haynes DR. Periodontitis and rheumatoid arthritis: a review. J Periodontol. 2005; 76:2066–2074.
Article11. Ziebolz D, Pabel SO, Lange K, Krohn-Grimberghe B, Hornecker E, Mausberg RF. Clinical periodontal and microbiologic parameters in patients with rheumatoid arthritis. J Periodontol. 2011; 82:1424–1432.
Article12. Schmickler J, Rupprecht A, Patschan S, Patschan D, Müller GA, Haak R, et al. Cross-sectional evaluation of periodontal status and microbiologic and rheumatoid parameters in a large cohort of patients with rheumatoid arthritis. J Periodontol. 2017; 88:368–379.
Article13. Choi IA, Kim JH, Kim YM, Lee JY, Kim KH, Lee EY, et al. Periodontitis is associated with rheumatoid arthritis: a study with longstanding rheumatoid arthritis patients in Korea. Korean J Intern Med. 2016; 31:977–986.
Article14. Lee JY, Choi IA, Kim JH, Kim KH, Lee EY, Lee EB, et al. Association between anti-Porphyromonas gingivalis or anti-α-enolase antibody and severity of periodontitis or rheumatoid arthritis (RA) disease activity in RA. BMC Musculoskelet Disord. 2015; 16:190.
Article15. Vander Cruyssen B, Van Looy S, Wyns B, Westhovens R, Durez P, Van den Bosch F, et al. DAS28 best reflects the physician’s clinical judgment of response to infliximab therapy in rheumatoid arthritis patients: validation of the DAS28 score in patients under infliximab treatment. Arthritis Res Ther. 2005; 7:R1063–R1071.16. Silness J, Loe H. Periodontal disease in pregnancy. Ii. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964; 22:121–135.
Article17. Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963; 21:533–551.
Article18. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999; 4:1–6.
Article19. Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL Jr. Microbial complexes in subgingival plaque. J Clin Periodontol. 1998; 25:134–144.
Article20. Papapanou PN. Periodontal diseases: epidemiology. Ann Periodontol. 1996; 1:1–36.
Article21. Ortiz P, Bissada NF, Palomo L, Han YW, Al-Zahrani MS, Panneerselvam A, et al. Periodontal therapy reduces the severity of active rheumatoid arthritis in patients treated with or without tumor necrosis factor inhibitors. J Periodontol. 2009; 80:535–540.
Article22. Mirrielees J, Crofford LJ, Lin Y, Kryscio RJ, Dawson DR 3rd, Ebersole JL, et al. Rheumatoid arthritis and salivary biomarkers of periodontal disease. J Clin Periodontol. 2010; 37:1068–1074.
Article23. Biyikoğlu B, Buduneli N, Kardeşler L, Aksu K, Pitkala M, Sorsa T. Gingival crevicular fluid MMP-8 and -13 and TIMP-1 levels in patients with rheumatoid arthritis and inflammatory periodontal disease. J Periodontol. 2009; 80:1307–1314.
Article24. Joseph R, Rajappan S, Nath SG, Paul BJ. Association between chronic periodontitis and rheumatoid arthritis: a hospital-based case-control study. Rheumatol Int. 2013; 33:103–109.
Article25. Harvey GP, Fitzsimmons TR, Dhamarpatni AA, Marchant C, Haynes DR, Bartold PM. Expression of peptidylarginine deiminase-2 and -4, citrullinated proteins and anti-citrullinated protein antibodies in human gingiva. J Periodontal Res. 2013; 48:252–261.
Article26. Bozkurt FY, Yetkin Ay Z, Berker E, Tepe E, Akkuş S. Anti-inflammatory cytokines in gingival crevicular fluid in patients with periodontitis and rheumatoid arthritis: a preliminary report. Cytokine. 2006; 35:180–185.
Article27. Ishi EP, Bertolo MB, Rossa C Jr, Kirkwood KL, Onofre MA. Periodontal condition in patients with rheumatoid arthritis. Braz Oral Res. 2008; 22:72–77.
Article28. Garib BT, Qaradaxi SS. Temporomandibular joint problems and periodontal condition in rheumatoid arthritis patients in relation to their rheumatologic status. J Oral Maxillofac Surg. 2011; 69:2971–2978.
Article29. Gleissner C, Willershausen B, Kaesser U, Bolten WW. The role of risk factors for periodontal disease in patients with rheumatoid arthritis. Eur J Med Res. 1998; 3:387–392.30. Kässer UR, Gleissner C, Dehne F, Michel A, Willershausen-Zönnchen B, Bolten WW. Risk for periodontal disease in patients with longstanding rheumatoid arthritis. Arthritis Rheum. 1997; 40:2248–2251.
Article31. Pischon N, Pischon T, Kröger J, Gülmez E, Kleber BM, Bernimoulin JP, et al. Association among rheumatoid arthritis, oral hygiene, and periodontitis. J Periodontol. 2008; 79:979–986.
Article32. Konig MF, Abusleme L, Reinholdt J, Palmer RJ, Teles RP, Sampson K, et al. Aggregatibacter actinomycetemcomitans-induced hypercitrullination links periodontal infection to autoimmunity in rheumatoid arthritis. Sci Transl Med. 2016; 8:369ra176.
Article33. Mikuls TR, Payne JB, Reinhardt RA, Thiele GM, Maziarz E, Cannella AC, et al. Antibody responses to Porphyromonas gingivalis (P. gingivalis) in subjects with rheumatoid arthritis and periodontitis. Int Immunopharmacol. 2009; 9:38–42.
Article34. Hitchon CA, Chandad F, Ferucci ED, Willemze A, Ioan-Facsinay A, van der Woude D, et al. Antibodies to porphyromonas gingivalis are associated with anticitrullinated protein antibodies in patients with rheumatoid arthritis and their relatives. J Rheumatol. 2010; 37:1105–1112.
Article35. Naito Y, Okuda K, Takazoe I, Watanabe H, Ishikawa I. The relationship between serum IgG levels to subgingival gram-negative bacteria and degree of periodontal destruction. J Dent Res. 1985; 64:1306–1310.
Article36. Lamster IB, Kaluszhner-Shapira I, Herrera-Abreu M, Sinha R, Grbic JT. Serum IgG antibody response to Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis: implications for periodontal diagnosis. J Clin Periodontol. 1998; 25:510–516.
Article37. Okada M, Kobayashi T, Ito S, Yokoyama T, Komatsu Y, Abe A, et al. Antibody responses to periodontopathic bacteria in relation to rheumatoid arthritis in Japanese adults. J Periodontol. 2011; 82:1433–1441.
Article38. Heliövaara M, Aho K, Aromaa A, Knekt P, Reunanen A. Smoking and risk of rheumatoid arthritis. J Rheumatol. 1993; 20:1830–1835.39. Silman AJ, Newman J, MacGregor AJ. Cigarette smoking increases the risk of rheumatoid arthritis. Results from a nationwide study of disease-discordant twins. Arthritis Rheum. 1996; 39:732–735.
Article40. Dougados M, Soubrier M, Antunez A, Balint P, Balsa A, Buch MH, et al. Prevalence of comorbidities in rheumatoid arthritis and evaluation of their monitoring: results of an international, cross-sectional study (COMORA). Ann Rheum Dis. 2014; 73:62–68.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of rheumatoid arthritis on periodontitis: a historical cohort study
- Microbiological links between periodontitis and systemic diseases: a brief review
- Effect of anti-rheumatic agents on periodontal parameters and biomarkers of inflammation: a systematic review and meta-analysis
- Rheumatoid arthritis is associated with early tooth loss: results from Korea National Health and Nutrition Examination Survey V to VI
- Periodontitis is associated with rheumatoid arthritis: a study with longstanding rheumatoid arthritis patients in Korea