J Breast Cancer.
2018 Dec;21(4):453-462. 10.4048/jbc.2018.21.e62.
Diagnostic Value of Contrast-Enhanced Digital Mammography versus Contrast-Enhanced Magnetic Resonance Imaging for the Preoperative Evaluation of Breast Cancer
- Affiliations
-
- 1Department of Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. shinho.kook@samsung.com
- KMID: 2429825
- DOI: http://doi.org/10.4048/jbc.2018.21.e62
Abstract
- PURPOSE
This study aimed to compare the diagnostic performance of contrast-enhanced digital mammography (CEDM) and contrast-enhanced magnetic resonance imaging (CEMRI) in preoperative evaluations, and to evaluate the effect of each modality on the surgical management of women with breast cancer.
METHODS
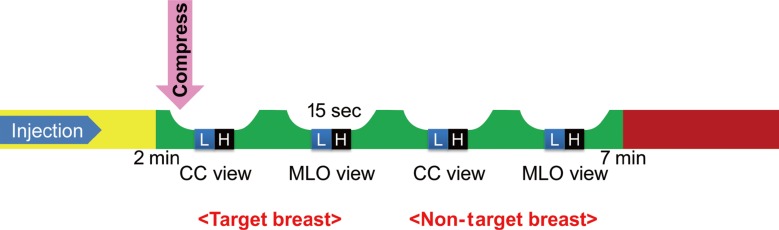
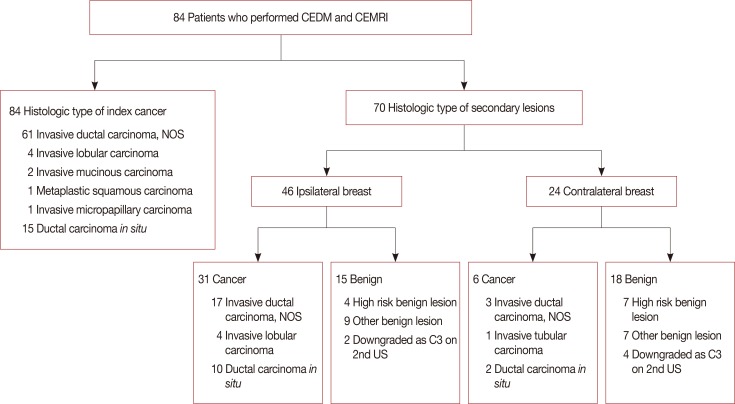
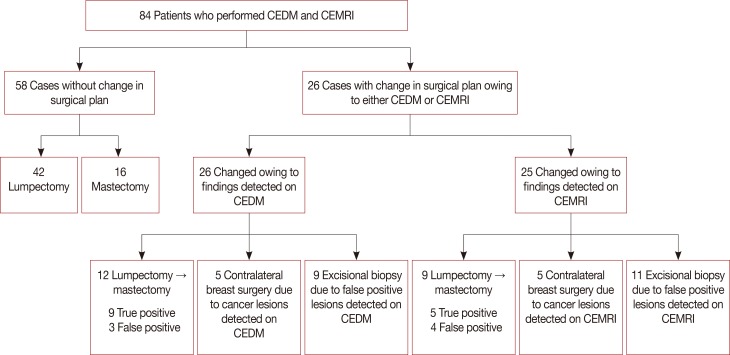
This single-center, prospective study was approved by the Institutional Review Board, and informed consent was obtained from all patients. From November 2016 to October 2017, 84 patients who were diagnosed with invasive carcinoma (69/84) and ductal carcinoma in situ (15/84), and underwent both CEDM and CEMRI, were enrolled. Imaging findings and surgical management were correlated with pathological results and compared. The diagnostic performance of both modalities in the detection of index and secondary cancers (multifocality and multicentricity), and occult cancer in the contralateral breast, was compared. The authors also evaluated whether CEDM or CEMRI resulted in changes in the surgical management of the affected breast due to imaging-detected findings.
RESULTS
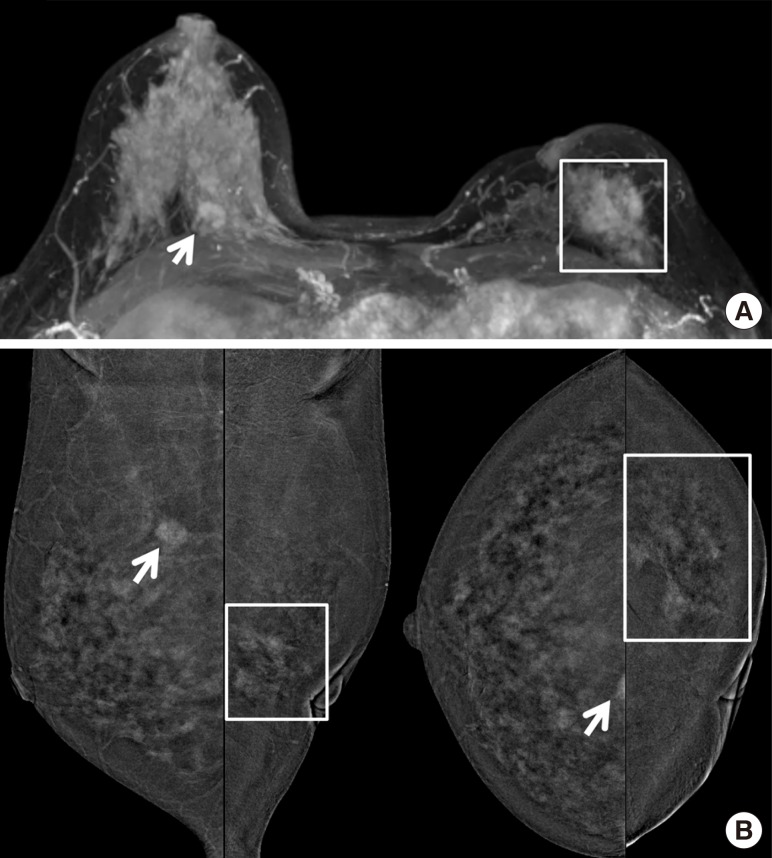
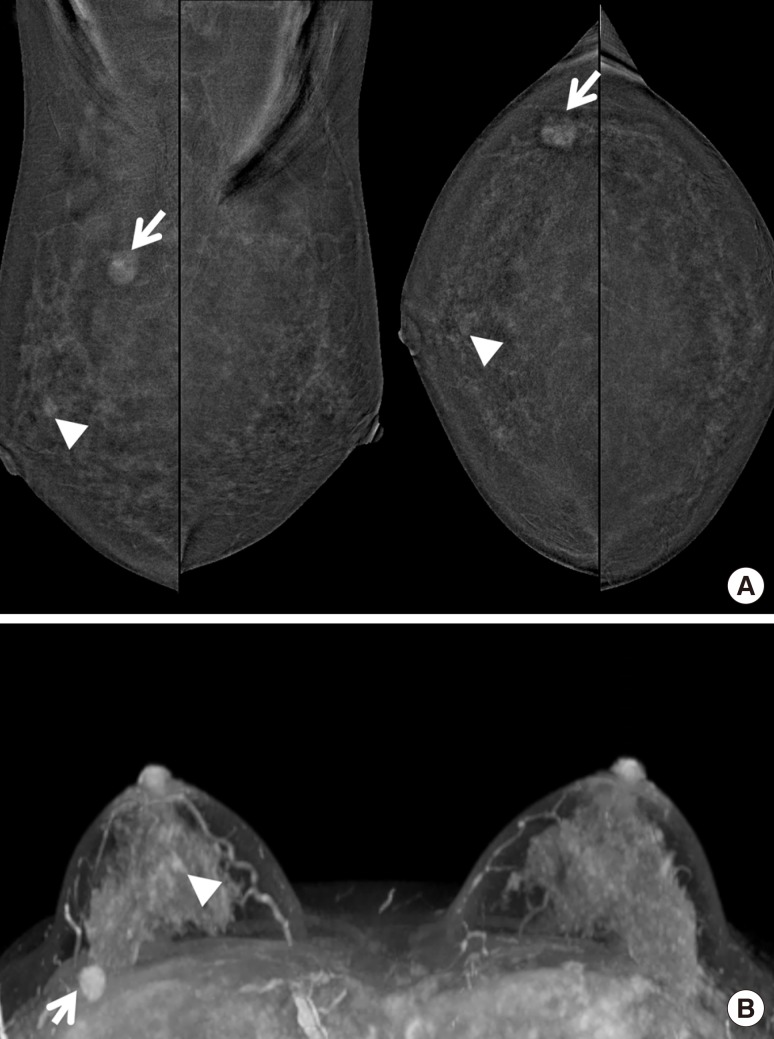
Eighty-four women were included in the analysis. Compared with CEMRI, CEDM demonstrated a similar sensitivity (92.9% [78/84] vs. 95.2% [80/84]) in detecting index cancer (p=0.563). For the detection of secondary cancers in the ipsilateral breast and occult cancer in the contralateral breast, no significant differences were found between CEDM and CEMRI (p=0.999 and p=0.999, respectively). Regarding changes in surgical management, CEDM resulted in similar changes compared with CEMRI (30.9% [26/84] vs. 29.7% [25/84], p=0.610). Regarding changes in surgical management due to false-positive findings, no significant differences were found between CEDM and CEMRI (34.6% [9/26] vs. 44.0% [11/25], p=0.782).
CONCLUSION
CEDM demonstrated a diagnostic performance comparable with CEMRI in depicting index cancers, secondary cancers, and occult cancer in the contralateral breast. CEDM demonstrated similar changes in surgical management compared with CEMRI.
MeSH Terms
Figure
Reference
-
1. Miller BT, Abbott AM, Tuttle TM. The influence of preoperative MRI on breast cancer treatment. Ann Surg Oncol. 2012; 19:536–540. PMID: 21751044.
Article2. Houssami N, Hayes DF. Review of preoperative magnetic resonance imaging (MRI) in breast cancer: should MRI be performed on all women with newly diagnosed, early stage breast cancer? CA Cancer J Clin. 2009; 59:290–302. PMID: 19679690.
Article3. Houssami N, Ciatto S, Macaskill P, Lord SJ, Warren RM, Dixon JM, et al. Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systematic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol. 2008; 26:3248–3258. PMID: 18474876.
Article4. Dromain C, Thibault F, Diekmann F, Fallenberg EM, Jong RA, Koomen M, et al. Dual-energy contrast-enhanced digital mammography: initial clinical results of a multireader, multicase study. Breast Cancer Res. 2012; 14:R94. PMID: 22697607.
Article5. Lewin JM, Isaacs PK, Vance V, Larke FJ. Dual-energy contrast-enhanced digital subtraction mammography: feasibility. Radiology. 2003; 229:261–268. PMID: 12888621.
Article6. Fallenberg EM, Dromain C, Diekmann F, Engelken F, Krohn M, Singh JM, et al. Contrast-enhanced spectral mammography versus MRI: initial results in the detection of breast cancer and assessment of tumour size. Eur Radiol. 2014; 24:256–264. PMID: 24048724.
Article7. Dromain C, Thibault F, Muller S, Rimareix F, Delaloge S, Tardivon A, et al. Dual-energy contrast-enhanced digital mammography: initial clinical results. Eur Radiol. 2011; 21:565–574. PMID: 20839001.
Article8. Bilimoria KY, Cambic A, Hansen NM, Bethke KP. Evaluating the impact of preoperative breast magnetic resonance imaging on the surgical management of newly diagnosed breast cancers. Arch Surg. 2007; 142:441–445. PMID: 17515485.
Article9. Lee-Felker SA, Tekchandani L, Thomas M, Gupta E, Andrews-Tang D, Roth A, et al. Newly diagnosed breast cancer: comparison of contrastenhanced spectral mammography and breast MR imaging in the evaluation of extent of disease. Radiology. 2017; 285:389–400. PMID: 28654337.
Article10. Ali-Mucheru M, Pockaj B, Patel B, Pizzitola V, Wasif N, Stucky CC, et al. Contrast-enhanced digital mammography in the surgical management of breast cancer. Ann Surg Oncol. 2016; 23(Suppl 5):649–655. PMID: 27638679.
Article11. The Korean Society of Radiology. The Korean Academy of Asthma, Allergy and Clinical Immunology. Korean Clinical Practice Guideline for Adverse Reactions to Injectable Iodinated Contrast Agent and Gadolinium-Based Contrast Agent Injection for MRI. 2nd ed. Seoul: The Korean Society of Radiology;2016.12. Ren B, Ruth C, Zhang Y, Smith A, Kennedy D, O'Keefe B, et al. Dual energy iodine contrast imaging with mammography and tomosynthesis. Bellingham: The International Society for Optics and Photonics;2013. p. 9.13. American College of Radiology, BI-RADS Committee. ACR BI-RADS Atlas: Breast Imaging Reporting and Data System. 5th ed. Reston: American College of Radiology;2013.14. Diekmann F, Freyer M, Diekmann S, Fallenberg EM, Fischer T, Bick U, et al. Evaluation of contrast-enhanced digital mammography. Eur J Radiol. 2011; 78:112–121. PMID: 19931350.
Article15. Salgado R, Aftimos P, Sotiriou C, Desmedt C. Evolving paradigms in multifocal breast cancer. Semin Cancer Biol. 2015; 31:111–118. PMID: 25066860.
Article16. Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver MJ. WHO Classification of Tumours of the Breast. 4th ed. Lyon: International Agency for Research on Cancer;2014.17. Kiluk JV, Acs G, Hoover SJ. High-risk benign breast lesions: current strategies in management. Cancer Control. 2007; 14:321–329. PMID: 17914332.
Article18. Moran MS, Schnitt SJ, Giuliano AE, Harris JR, Khan SA, Horton J, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. J Clin Oncol. 2014; 32:1507–1515. PMID: 24516019.
Article19. Hobbs MM, Taylor DB, Buzynski S, Peake RE. Contrast-enhanced spectral mammography (CESM) and contrast enhanced MRI (CEMRI): patient preferences and tolerance. J Med Imaging Radiat Oncol. 2015; 59:300–305. PMID: 25900704.
Article20. Heywang-Köbrunner SH, Beck R. Contrast-Enhanced MRI of the Breast. 2nd ed. Berlin: Springer;1996.22. Bazzocchi M, Zuiani C, Panizza P, Del Frate C, Soldano F, Isola M, et al. Contrast-enhanced breast MRI in patients with suspicious microcalcifications on mammography: results of a multicenter trial. AJR Am J Roentgenol. 2006; 186:1723–1732. PMID: 16714666.
Article23. Jochelson MS, Dershaw DD, Sung JS, Heerdt AS, Thornton C, Moskowitz CS, et al. Bilateral contrast-enhanced dual-energy digital mammography: feasibility and comparison with conventional digital mammography and MR imaging in women with known breast carcinoma. Radiology. 2013; 266:743–751. PMID: 23220903.
Article24. Nadler M, Al-Attar H, Warner E, Martel AL, Balasingham S, Zhang L, et al. MRI surveillance for women with dense breasts and a previous breast cancer and/or high risk lesion. Breast. 2017; 34:77–82. PMID: 28527397.
Article25. Bleicher RJ, Ciocca RM, Egleston BL, Sesa L, Evers K, Sigurdson ER, et al. Association of routine pretreatment magnetic resonance imaging with time to surgery, mastectomy rate, and margin status. J Am Coll Surg. 2009; 209:180–187. PMID: 19632594.
Article26. Delille JP, Slanetz PJ, Yeh ED, Kopans DB, Garrido L. Physiologic changes in breast magnetic resonance imaging during the menstrual cycle: perfusion imaging, signal enhancement, and influence of the T1 relaxation time of breast tissue. Breast J. 2005; 11:236–241. PMID: 15982388.
Article27. King V, Gu Y, Kaplan JB, Brooks JD, Pike MC, Morris EA. Impact of menopausal status on background parenchymal enhancement and fibroglandular tissue on breast MRI. Eur Radiol. 2012; 22:2641–2647. PMID: 22752463.
Article28. King V, Brooks JD, Bernstein JL, Reiner AS, Pike MC, Morris EA. Background parenchymal enhancement at breast MR imaging and breast cancer risk. Radiology. 2011; 260:50–60. PMID: 21493794.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Value of Contrast-Enhanced Digital Mammography Versus Contrast-Enhanced MRI for Detecting Residual Disease After Neoadjuvant Chemotherapy for Breast Cancer
- A Suspicious Breast Lesion Detected by Dynamic Contrast-Enhanced MRI and Pathologically Confirmed as Capillary Hemangioma: a Case Report and Literature Review
- Use of Abbreviated Magnetic Resonance Imaging in Breast Cancer Screening
- Recent development of diagnostic imaging of hepatocellular carcinoma
- Abbreviated Breast Magnetic Resonance Imaging: Background, Evidence From Studies, and Future Considerations