Adv Pediatr Surg.
2018 Dec;24(2):86-94. 10.13029/aps.2018.24.2.86.
Long-Term Outcome of Patients Undergoing Total Proctocolectomy with Ileal Pouch-Anal Anastomosis in Childhood
- Affiliations
-
- 1Department of Pediatric Surgery, Seoul National University College of Medicine, Seoul, Korea. spkhy02@snu.ac.kr
- 2Department of Surgery, Korea University Anam Hospital, Seoul, Korea.
- 3Department of Pediatric Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 4Department of Surgery, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Surgery, Chung-Ang University Hospital, Seoul, Korea.
- KMID: 2429805
- DOI: http://doi.org/10.13029/aps.2018.24.2.86
Abstract
- PURPOSE
Total proctocolectomy with ileal pouch-anal anastomosis (T-IPAA) in childhood is a surgical procedure mainly applied to familial adenomatous polyposis (FAP) or ulcerative colitis (UC), but it can be applied to non-FAP/non-UC disease (NFNU). Studies regarding the role of T-IPAA who underwent the operation in childhood, especially in terms of long-term gastrointestinal function, complications, and quality of life (QOL) are limited. The aim of this study was to evaluate the characteristics of patients receiving T-IPAA and to compare their bowel function outcomes and QOL.
METHODS
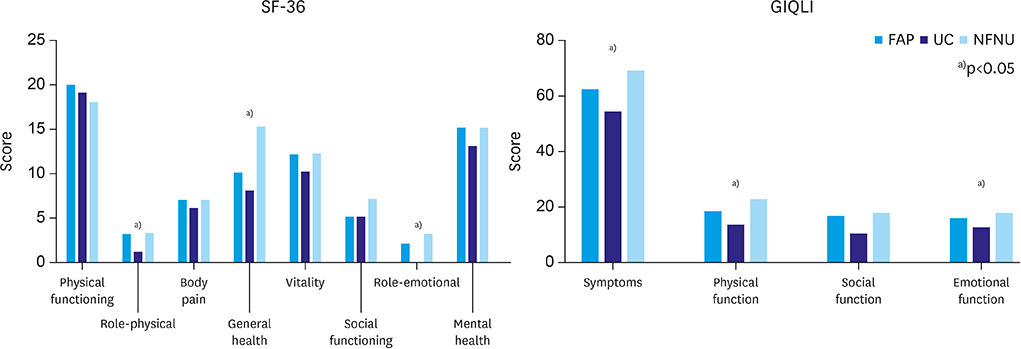
Patients aged ≤18 years at the time of T-IPAA were included. Their medical records were retrospectively reviewed. Krickenbeck classification, Cleveland Clinic Incontinence (CCI) score, 36-item Short-form Health Survey Questionnaire, and Gastrointestinal Quality of Life Index were used for the evaluation of bowel function and QOL. The median follow-up period was 9.8 years.
RESULTS
Of the 25 patients, 9 had FAP, 9 had UC, and 7 had NFNU. NFNU include 3 of Hirschsprung disease, 2 of intestinal neuronal dysplasia, and 2 of imperforate anus. The median age at T-IPAA was 17.8, 14.2, and 9.3 years for FAP, UC, and NFNU, respectively (p=0.001). Bowel function was satisfactory in terms of voluntary bowel movement (VBM), soiling, and constipation. VBM and constipation were not different between the groups, but soiling was most in NFNU (100%, p=0.047). However, QOL was best in the NFNU group in surveys (p=0.034 and 0.004, respectively).
CONCLUSION
T-IPAA could be safely applied not only for FAP and UC but also for other diseases in selective cases, with caution.
Keyword
MeSH Terms
Figure
Reference
-
1. Tudyka VN, Clark SK. Surgical treatment in familial adenomatous polyposis. Ann Gastroenterol. 2012; 25:201–206.2. Ross H, Steele SR, Varma M, Dykes S, Cima R, Buie WD, et al. Practice parameters for the surgical treatment of ulcerative colitis. Dis Colon Rectum. 2014; 57:5–22.
Article3. Fazio VW, Kiran RP, Remzi FH, Coffey JC, Heneghan HM, Kirat HT, et al. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg. 2013; 257:679–685.4. Hahnloser D, Pemberton JH, Wolff BG, Larson DR, Crownhart BS, Dozois RR. Results at up to 20 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Br J Surg. 2007; 94:333–340.
Article5. Tekkis PP, Lovegrove RE, Tilney HS, Smith JJ, Sagar PM, Shorthouse AJ, et al. Long-term failure and function after restorative proctocolectomy - a multi-centre study of patients from the UK National Ileal Pouch Registry. Colorectal Dis. 2010; 12:433–441.
Article6. Tulchinsky H, Hawley PR, Nicholls J. Long-term failure after restorative proctocolectomy for ulcerative colitis. Ann Surg. 2003; 238:229–234.
Article7. Uchino M, Ikeuchi H, Sugita A, Futami K, Watanabe T, Fukushima K, et al. Pouch functional outcomes after restorative proctocolectomy with ileal-pouch reconstruction in patients with ulcerative colitis: Japanese multi-center nationwide cohort study. J Gastroenterol. 2018; 53:642–651.
Article8. Lillehei CW, Leichtner A, Bousvaros A, Shamberger RC. Restorative proctocolectomy and ileal pouch-anal anastomosis in children. Dis Colon Rectum. 2009; 52:1645–1649.
Article9. Ozdemir Y, Kiran RP, Erem HH, Aytac E, Gorgun E, Magnuson D, et al. Functional outcomes and complications after restorative proctocolectomy and ileal pouch anal anastomosis in the pediatric population. J Am Coll Surg. 2014; 218:328–335.
Article10. Stavlo PL, Libsch KD, Rodeberg DA, Moir CR. Pediatric ileal pouch-anal anastomosis: functional outcomes and quality of life. J Pediatr Surg. 2003; 38:935–939.
Article11. Fonkalsrud EW. Long-term results after colectomy and ileoanal pull-through procedure in children. Arch Surg. 1996; 131:881–885.
Article12. Hukkinen M, Koivusalo A, Rintala RJ, Pakarinen MP. Restorative proctocolectomy with J-pouch ileoanal anastomosis for total colonic aganglionosis among neonates and infants. J Pediatr Surg. 2014; 49:570–574.
Article13. Rintala RJ, Lindahl HG. Proctocolectomy and J-pouch ileo-anal anastomosis in children. J Pediatr Surg. 2002; 37:66–70.
Article14. Holschneider A, Hutson J, Peña A, Beket E, Chatterjee S, Coran A, et al. Preliminary report on the International Conference for the Development of Standards for the Treatment of Anorectal Malformations. J Pediatr Surg. 2005; 40:1521–1526.
Article15. Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993; 36:77–97.
Article16. Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmülling C, Neugebauer E, et al. Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg. 1995; 82:216–222.
Article17. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992; 30:473–483.18. Puri P, Gosemann JH. Variants of Hirschsprung disease. Semin Pediatr Surg. 2012; 21:310–318.
Article19. Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. BMJ. 1978; 2:85–88.
Article20. Coran AG. A personal experience with 100 consecutive total colectomies and straight ileoanal endorectal pull-throughs for benign disease of the colon and rectum in children and adults. Ann Surg. 1990; 212:242–248.
Article21. Nyam DC, Brillant PT, Dozois RR, Kelly KA, Pemberton JH, Wolff BG. Ileal pouch-anal canal anastomosis for familial adenomatous polyposis: early and late results. Ann Surg. 1997; 226:514–521.22. Rintala RJ, Lindahl H. Restorative proctocolectomy for ulcerative colitis in children--is the J-pouch better than straight pull-through? J Pediatr Surg. 1996; 31:530–533.23. Diederen K, Sahami SS, Tabbers MM, Benninga MA, Kindermann A, Tanis PJ, et al. Outcome after restorative proctocolectomy and ileal pouch-anal anastomosis in children and adults. Br J Surg. 2017; 104:1640–1647.
Article24. Tan Tanny SP, Yoo M, Hutson JM, Langer JC, King SK. Current surgical practice in pediatric ulcerative colitis: a systematic review. J Pediatr Surg. 2018; Sep. 07. [Epub]. DOI: 10.1016/j.jpedsurg.2018.08.050.
Article25. Dalal RL, Shen B, Schwartz DA. Management of pouchitis and other common complications of the pouch. Inflamm Bowel Dis. 2018; 24:989–996.
Article26. Raviram S, Rajan R, Sindhu RS, Bonny N, Kuruvilla AP, Subhalal N. Quality of life, social impact and functional outcome following ileal pouch-anal anastomosis for ulcerative colitis and familial adenomatous polyposis. Indian J Gastroenterol. 2015; 34:252–255.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adenocarcinoma in Ileal Pouch after Proctocolectomy for Familial Adenomatous Polyposis: Report of A Case
- Carcinoma in an Ileal Pouch after Proctocolectomy, with Ileal Pouch-Anal
- The Clinical Results of a Total Proctocolectomy with an Ileal Pouch-Anal Anastomosis: 12 Cases
- Two Cases of Multiple Adenomas in the Ileal Pouch after Total Proctocolectomy in Patients with Familial Adenomatous Polyposis
- Open Versus Laparoscopic Total Proctocolectomy with Ileal Pouch Anal Anastomosis for FAP