J Menopausal Med.
2018 Apr;24(1):17-28. 10.6118/jmm.2018.24.1.17.
Insomnia with Musculoskeletal Pain in Postmenopause: Associations with Symptoms, Mood, and Quality of Life
- Affiliations
-
- 1Department of Psychobiology, Universidade Federal de São Paulo, São Paulo, Brazil. helenahachul@gmail.com
- 2Department of Gynecology, Universidade Federal de São Paulo, São Paulo, Brazil.
- 3Department of Gynecology, Casa de Saúde Santa Marcelina, São Paulo, Brazil.
- KMID: 2429216
- DOI: http://doi.org/10.6118/jmm.2018.24.1.17
Abstract
OBJECTIVES
To investigate the relationship between insomnia (INS) combined with chronic musculoskeletal pain (MSP) in postmenopausal women and its characteristics regarding MSP, menopausal and mood symptoms, sleep and quality of life (QOL).
METHODS
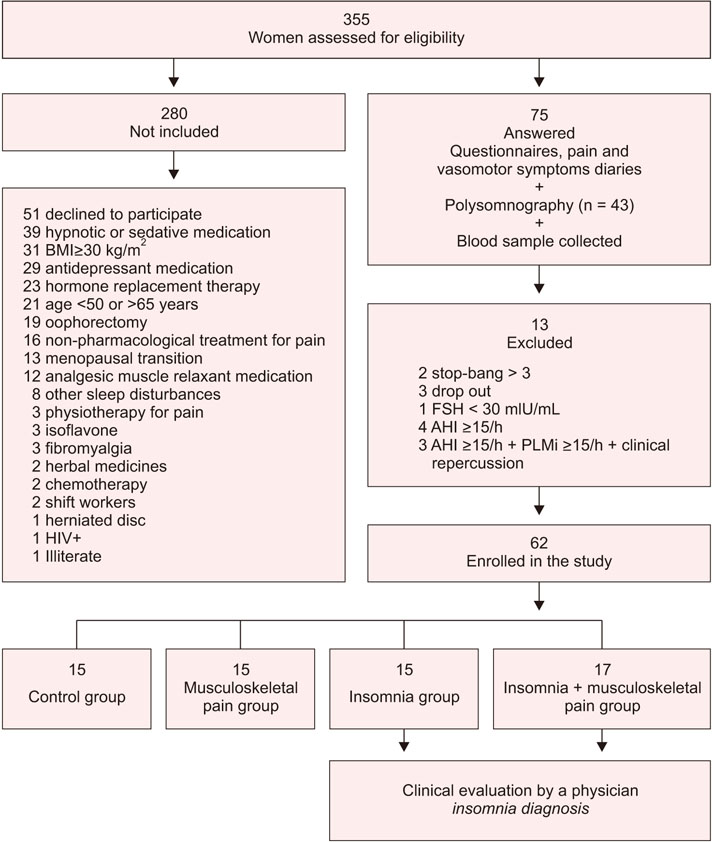
A cross-sectional control study in 4 groups of postmenopausal women: control (n = 15), MSP (n = 15), INS (n =15) and INS + MSP (n = 17). Sixty-two participants completed questionnaires and had blood collected, and 43 underwent polysomnography.
RESULTS
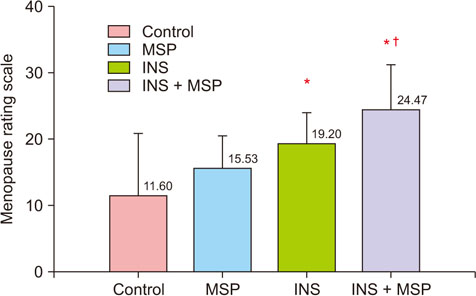
INS was associated with increased anxiety (P = 0.04) and sleep fragmentation (P = 0.02); worse MSP severity (P = 0.00), MSP interference with daily function (P = 0.00), higher pain intensity at midday (P = 0.02) and menopausal symptoms (P = 0.00); and reduced QOL (P = 0.00). MSP was associated with increased anxiety (P = 0.02) and menopausal symptoms (P = 0.00), and reduced QOL (P = 0.05). In the whole sample, depression symptoms were higher but no statistical differences were found between groups (P = 0.47). Worse QOL was associated with both higher depressive symptoms (P = 0.01) and worse pain interference (P = 0.02)
CONCLUSIONS
INS + MSP was related to higher menopausal and anxiety symptoms, more sleep fragmentation and complaints of MSP severity and interference, more pain sites and worse QOL. The presence of INS was associated to more MSP. Sleep management is essential in women who have developed chronic MSP.
MeSH Terms
Figure
Reference
-
1. Davis SR, Lambrinoudaki I, Lumsden M, Mishra GD, Pal L, Rees M, et al. Menopause. Nat Rev Dis Primers. 2015; 1:15004.
Article2. Neslihan Carda S, Bilge SA, Ozturk TN, Oya G, Ece O, Hamiyet B. The menopausal age, related factors and climacteric symptoms in Turkish women. Maturitas. 1998; 30:37–40.
Article3. Monterrosa-Castro A, Marrugo-Flórez M, Romero-Pérez I, Chedraui P, Fernández-Alonso AM, Pérez-López FR. Prevalence of insomnia and related factors in a large midaged female Colombian sample. Maturitas. 2013; 74:346–351.
Article4. Generaal E, Vogelzangs N, Penninx BW, Dekker J. Insomnia, sleep duration, depressive symptoms, and the onset of chronic multisite musculoskeletal pain. Sleep. 2017; 40.5. Woods NF, Hohensee C, Carpenter JS, Cohen L, Ensrud K, Freeman EW, et al. Symptom clusters among MsFLASH clinical trial participants. Menopause. 2016; 23:158–165.
Article6. Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008; 108:812–821.7. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001; 2:297–307.
Article8. Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012; 97:1159–1168.
Article9. Celik EC, Yalcinkaya EY, Atamaz F, Karatas M, Ones K, Sezer T, et al. Validity and reliability of a Turkish Brief Pain Inventory Short Form when used to evaluate musculoskeletal pain. J Back Musculoskelet Rehabil. 2017; 30:229–233.
Article10. Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983; 17:45–56.
Article11. Heinemann LA, Potthoff P, Schneider HP. International versions of the Menopause Rating Scale (MRS). Health Qual Life Outcomes. 2003; 1:28.12. Skevington SM, Lotfy M, O'Connell KA. The World Health Organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004; 13:299–310.
Article13. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988; 56:893–897.
Article14. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961; 4:561–571.
Article15. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28:193–213.
Article16. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991; 14:540–545.
Article17. Iber C, Ancoli-Israel S, Chesson A, Quan SF. The AASM manual for the scoring of sleep and associated events: Rules, terminology and technical specifications. Westchester, IL: American Academy of Sleep Medicine;2007.18. Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987; 18:233–237.
Article19. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Arlington, VA: American Psychiatric Association;2013.20. Tang NK, Goodchild CE, Sanborn AN, Howard J, Salkovskis PM. Deciphering the temporal link between pain and sleep in a heterogeneous chronic pain patient sample: a multilevel daily process study. Sleep. 2012; 35:675–687a.
Article21. Van Cauter E, Tasali E. Endocrine physiology in relation to sleep and sleep disturbances. In : Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 6th ed. Philadelphia, PA: Elsevier;2017. p. 202–219.22. Roehrs T, Carskadon MA, Dement WC, Roth T. Daytime sleepiness and alertness. In : Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 6th ed. Philadelphia, PA: Elsevier;2017. p. 39–48.23. Davies KA, Macfarlane GJ, Nicholl BI, Dickens C, Morriss R, Ray D, et al. Restorative sleep predicts the resolution of chronic widespread pain: results from the EPIFUND study. Rheumatology (Oxford). 2008; 47:1809–1813.
Article24. Kravitz HM, Ganz PA, Bromberger J, Powell LH, Sutton-Tyrrell K, Meyer PM. Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition. Menopause. 2003; 10:19–28.25. Terauchi M, Hiramitsu S, Akiyoshi M, Owa Y, Kato K, Obayashi S, et al. Associations between anxiety, depression and insomnia in peri- and post-menopausal women. Maturitas. 2012; 72:61–65.
Article26. Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007; 30:213–218.
Article27. Bjurstrom MF, Irwin MR. Polysomnographic characteristics in nonmalignant chronic pain populations: A review of controlled studies. Sleep Med Rev. 2016; 26:74–86.
Article28. Lampio L, Saaresranta T, Polo O, Polo-Kantola P. Subjective sleep in premenopausal and postmenopausal women during workdays and leisure days: a sleep diary study. Menopause. 2013; 20:655–660.29. Mirhaghjou SN, Niknami M, Moridi M, Pakseresht S, Kazemnejad E. Quality of life and its determinants in postmenopausal women: a population-based study. Appl Nurs Res. 2016; 30:252–256.
Article30. The WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998; 46:1569–1585.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationships among Mood Status, Social Support, Symptom Experience and Quality of Life in Colorectal Cancer Patients - based on the Theory of Unpleasant Symptoms
- Moderating Effect of Inner Strength between Mood Status and Quality of Life in Female Patients with Lung Cancer
- Mediation Effect of Insomnia Symptoms on Relation Between Stress and Quality of Life
- Risk Factors Associated with Clinical Insomnia in Chronic Low Back Pain: A Retrospective Analysis in a University Hospital in Korea
- Diagnosis and Treatment of Menopause-Related Depressio