Yonsei Med J.
2005 Dec;46(6):851-858.
Pineal Cavernous Malformations: Report of Two Cases
- Affiliations
-
- 1Department of Neurosurgery, Brain Research Institute, Yonsei University College of Medicine, Seoul, Korea.
Abstract
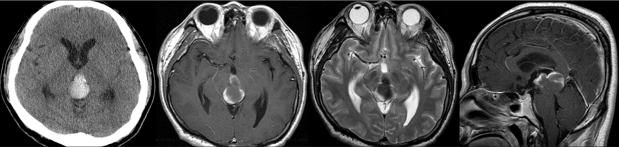
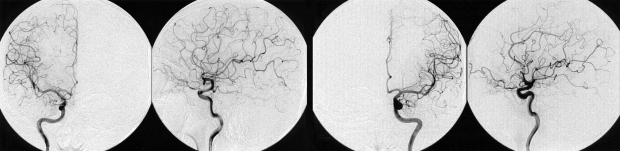
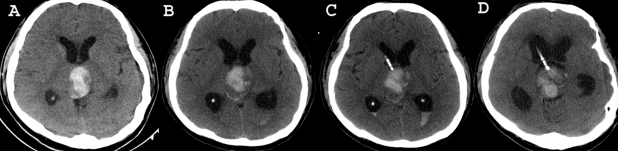
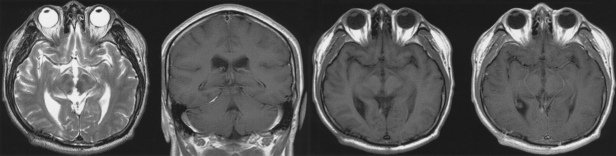
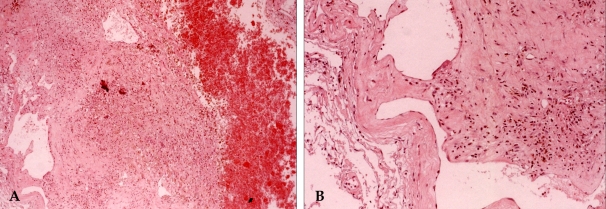
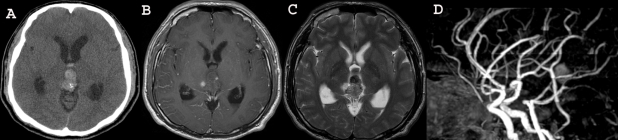
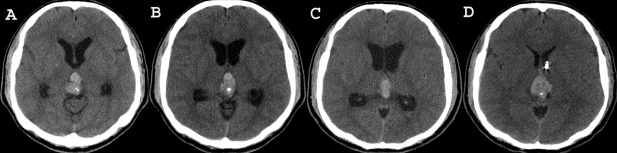
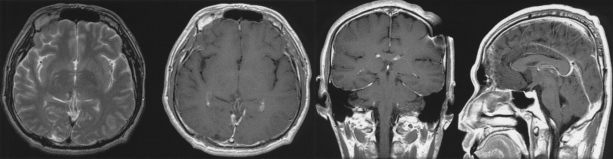
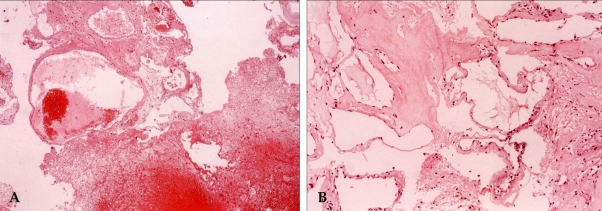
- Pineal hemorrhage only occurs in rare cases, and this known to have several different causes such as germ cell tumors, pineal cysts and vascular malformations, including the cavernous malformations. Pineal cavernous malformations are extremely rare: to date only fifteen cases have been reported worldwide. Although the diagnosis of pineal cavernous malformation is not easy because of the extreme rareness of this condition, the presence of this lesion can be suspected based on its typical radiological findings. Case 1. A 42-year- old man presented with a limitation in his upward gazing. Radiologic examinations showed acute hemorrhage in the pineal region. He underwent ventriculo-peritoneal (VP) shunting but the patient's condition deteriorated after the shunting surgery. We operated and totally removed the tumor and the hemorrhages via an occipital-transtentorial approach. Case 2. A 37-year-old man presented with diplopia. Radiologic examinations showed acute hemorrhage in the third ventricle. He underwent VP shunting, and after this procedure the diplopia was aggravated. We operated and totally removed the tumor and the hemorrhages via an occipital-transtentorial approach. If there is no doubt about the pineal cavernous malformation on MR imaging, we strongly recommend early surgical intervention without performing a risky biopsy. In this study, we describe our experiences for the diagnosis of cavernous malformations in the pineal region with special emphasis on the radiological aspects and the clinical course of this disease.
Keyword
MeSH Terms
Figure
Reference
-
1. Al-Shahi R, Bhattacharya JJ, Currie DG, Papanastassiou V, Ritchie V, Roberts RC, et al. Prospective, population-based detection of intracranial vascular malformations in adults: the Scottish Intracranial Vascular Malformation Study (SIVMS). Stroke. 2003; 34:1163–1169. PMID: 12702837.2. Hang Z, Shi Y, Wei Y. A pathological analysis of 180 cases of vascular malformation of brain. Zhonghua Bing Li Xue Za Zhi. 1996; 25:135–138. Chinese. PMID: 9275664.3. Kim DS, Park YG, Choi JU, Chung SS, Lee KC. An analysis of the natural history of cavernous malformations. Surg Neurol. 1997; 48:9–18. PMID: 9199678.
Article4. Mazza C, Scienza R, Beltramello A, Da Pian R. Cerebral cavernous malformations (cavernomas) in the pediatric age-group. Childs Nerv Syst. 1991; 7:139–146. PMID: 1878867.
Article5. McNeely PD, Howes WJ, Mehta V. Pineal apoplexy: is it a facilitator for the development of pineal cysts? Can J Neurol Sci. 2003; 30:67–71. PMID: 12619788.
Article6. Kobayashi S, Kamagata M, Nakamura M, Nakazato Y, Sasaki T. Pineal apoplexy due to massive hemorrhage associated with cavernous angioma: case report. Surg Neurol. 2001; 55:365–371. PMID: 11483199.7. Lombardi D, Scheithauer BW, Villani RM, Giovanelli M, de Tribolet N. Cavernous haemangioma of the pineal region. Acta Neurochir (Wien). 1996; 138:678–683. PMID: 8836282.
Article8. Hung YC, Lee EJ, Wang LC, Chen HH, Yan JJ, Yu CY. Mixed germ cell tumor presenting as intratumoral hemorrhage: report of a case originated from the pineal region. Kaohsiung J Med Sci. 1999; 15:498–503. PMID: 10518367.9. Maruki C, Takara K, Abe K, Tsunoda A, Ebato M, Ikeya F. Primary pineal embryonal carcinoma occurring in a middle aged man. No Shinkei Geka. 2000; 28:909–912. Japanese. PMID: 11070913.10. Nogueira K, Liberman B, Pimentel-Filho FR, Goldman J, Silva ME, Vieira JO, et al. hCG-secreting pineal teratoma causing precocious puberty: report of two patients and review of the literature. J Pediatr Endocrinol Metab. 2002; 15:1195–1201. PMID: 12387519.
Article11. Sakurada K, Kayama T, Kawakami K, Saino M, Sato S. A successfully operated case of choriocarcinoma with recurrent intratumoral hemorrhage. No Shinkei Geka. 2000; 28:67–72. Japanese. PMID: 10642996.12. Kida Y, Banno M, Kanzaki M, Kobayashi T, Kageyama N. Pineal choriocarcinoma presenting massive ventricular hemorrhage--a case report. No Shinkei Geka. 1985; 13:641–645. Japanese. PMID: 3840234.13. Wakai S, Yamakawa K, Manaka S, Takakura K. Spontaneous intracranial hemorrhage caused by brain tumor: its incidence and clinical significance. Neurosurgery. 1982; 10:437–444. PMID: 7099393.14. Fujii T, Itakura T, Hayashi S, Komai N, Nakamine H, Saito K. Primary pineal choriocarcinoma with hemorrhage monitored by computerized tomography. Case report. J Neurosurg. 1981; 55:484–487. PMID: 7196441.15. Mukherjee KK, Banerji D, Sharma R. Pineal cyst presenting with intracystic and subarachnoid haemorrhage: report of a case and review of the literature. Br J Neurosurg. 1999; 13:189–192. PMID: 10616590.
Article16. Mena H, Armonda RA, Ribas JL, Ondra SL, Rushing EJ. Nonneoplastic pineal cysts: a clinicopathologic study of twenty-one cases. Ann Diagn Pathol. 1997; 1:11–18. PMID: 9869821.
Article17. Vallee B, Meriot P, Dam Hieu P, Person H. Benign hemorrhagic cyst of the pineal region. Treatment by stereotactic puncture. 4-year follow-up. Neurochirurgie. 1997; 43:303–307. French. PMID: 9686235.18. Tekkok IH, Ventureyra EC. Spontaneous intracranial hemorrhage of structural origin during the first year of life. Childs Nerv Syst. 1997; 13:154–165. PMID: 9137857.19. Matsumoto K, Imaoka T, Tomita S, Ohmoto T. Pineocytoma with massive intratumoral hemorrhage after ventriculoperitoneal shunt- case report. Neurol Med Chir (Tokyo). 1997; 37:911–915. PMID: 9465590.
Article20. Ohba S, Kurisu K, Arita K, Sugiyama K, Inoue T, Satoh H, et al. Falcotentorial meningioma accompanied by temporal lobe hematoma. Hiroshima J Med Sci. 2001; 50:75–77. PMID: 11720166.21. Cervoni L, Artico M, Salvati M, Bristot R, Wierzbicki V, Gagliardi FM. Haemangiopericytoma and meningioma presenting clinically with intracranial haemorrhage: report of three cases and review of the literature. Zentralbl Neurochir. 1993; 54:20–23. PMID: 8493835.22. Vaquero J, Martinez R, Magallon R, Ramiro J. Intracranial metastases to the pineal region. Report of three cases. J Neurosurg Sci. 1991; 35:55–57. PMID: 1890463.23. Swaroop GR, Whittle IR. Pineal apoplexy: an occurrence with no diagnostic clinicopathological features. Br J Neurosurg. 1998; 12:274–276. PMID: 11013695.24. Decq P, Le Guerinel C, Sakka L, Roujeau T, Sol J, Palfi S, et al. Endoscopic surgery of third ventricle lesions. Neurochirurgie. 2000; 46:286–294. PMID: 10854986.25. Koenigsberg RA, Faro S, Marino R, Turz A, Goldman W. Imaging of pineal apoplexy. Clin Imaging. 1996; 20:91–94. PMID: 8744815.
Article26. Osborn RE, Deen HG, Kerber CW, Glass RF. A case of hemorrhagic pineal cyst: MR/CT correlation. Neuroradiology. 1989; 31:187–189. PMID: 2747899.
Article27. Richardson JK, Hirsch CS. Sudden, unexpected death due to "pineal apoplexy". Am J Forensic Med Pathol. 1986; 7:64–68. PMID: 3728423.
Article28. Merhemic Z, Kadenic Z, Sulejmanpasic G. Magnetic resonance and magnetic resonance angiography in the diagnosis of vascular anomalies in childhood. Med Arh. 2000; 58:114–116. Bosnian. PMID: 15137223.29. Vishteh AG, Nadkarni T, Spetzler RF. Cavernous malformation of the pineal region: short report and review of the literature. Br J Neurosurg. 2000; 14:147–151. PMID: 10889892.30. Slavin KV, Dujovny M, McDonald LW, Camras LR, Ausman JI. Pineal region: rare location of a cavernous haemangioma. Neurol Res. 1994; 16:133–136. PMID: 7913998.
Article31. Porter PJ, Willinsky RA, Harper W, Wallace MC. Cerebral cavernous malformations: natural history and prognosis after clinical deterioration with or without hemorrhage. J Neurosurg. 1997; 87:190–197. PMID: 9254081.
Article32. Chang HS, Hongo K, Nakagawa H, Tsuge T. Surgical decision-making on cerebral cavernous malformations. J Clin Neurosci. 2001; 8:416–420. PMID: 11535007.
Article33. Ruiz-Sandoval JL, Cantu C, Barinagarrementeria F. Intracerebral hemorrhage in young people: analysis of risk factors, location, causes, and prognosis. Stroke. 1999; 30:537–541. PMID: 10066848.34. Amin-Hanjani S, Ogilvy CS, Ojemann RG, Crowell RM. Risks of surgical management for cavernous malformations of the nervous system. Neurosurgery. 1998; 42:1220–1228. PMID: 9632179.
Article35. Braun V, Antoniadis G, Rath S, Richter HP. Cavernoma. Indications for surgical removal and outcome. Nervenarzt. 1996; 67:301–305. German. PMID: 8684508.