J Korean Neurosurg Soc.
2018 Nov;61(6):737-746. 10.3340/jkns.2018.0047.
Cranioplasty Using Autologous Bone versus Porous Polyethylene versus Custom-Made Titanium Mesh : A Retrospective Review of 108 Patients
- Affiliations
-
- 1Department of Neurosurgery, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea. leesb@catholic.ac.kr
- KMID: 2428116
- DOI: http://doi.org/10.3340/jkns.2018.0047
Abstract
OBJECTIVE
The purpose of this study was to compare the cosmetic outcome and complications after cranioplasty (CP) due to three different implant materials, and analyze the mean implant survival and cumulative survival rate based on these results.
METHODS
We reviewed 108 patients retrospectively who underwent CP between January 2014 and November 2016. Autologous bone (AB; 45 patients) and synthetic materials with porous polyethylene (PP; 32 patients) and custom-made 3-dimensional printed titanium mesh (CT; 31 patients) were used as implants.
RESULTS
Regardless of implanted materials, more than 89.8% of the CP patients were satisfied with the cosmetic outcome. No statistically significant difference was observed among the three groups. The overall postoperative complication rates of each group were 31.1% in the AB group, 15.6% in the PP group and 3.2% in the CT group. The CT group showed lower complication rates compared with AB and PP groups (χ2-test : AB vs. PP, p=0.34; AB vs. CT, p=0.00; PP vs. CT, p=0.03). The AB and PP groups demonstrated a higher post-CP infection rate (11.1% and 6.3%) than the CT group (3.2%). However, no significant difference in the incidence of post-CP infection was observed among the three groups. The PP and CT groups demonstrated a higher mean implant survival time and cumulative survival rate than the AB group at the last follow-up (p < 0.05).
CONCLUSION
In comparison with AB and PP, cranioplasty with CT shows benefits in terms of lower post-CP complication, less intraoperative bleeding loss, shorter operation time and in-hospital stay. The PP and CT groups showed higher implant survival time and cumulative survival rate compared with the AB group.
MeSH Terms
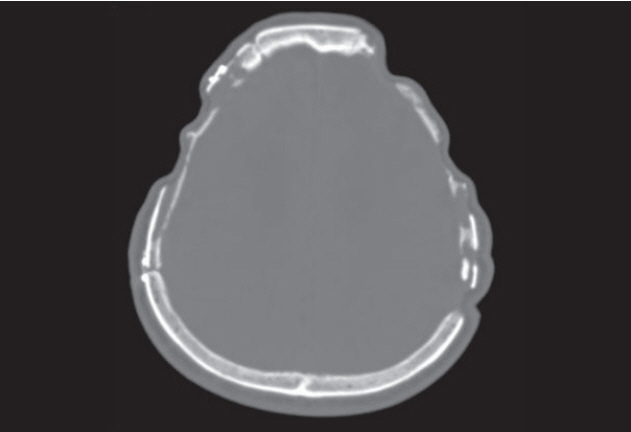
Figure
Cited by 2 articles
-
Risk Factor Analysis of Cryopreserved Autologous Bone Flap Resorption in Adult Patients Undergoing Cranioplasty with Volumetry Measurement Using Conventional Statistics and Machine-Learning Technique
Yohan Son, Jaewoo Chung
J Korean Neurosurg Soc. 2024;67(1):103-114. doi: 10.3340/jkns.2023.0143.Editors’ Pick in January 2024
Hee-Jin Yang
J Korean Neurosurg Soc. 2024;67(1):1-2. doi: 10.3340/jkns.2023.0254.
Reference
-
References
1. Agrawal D, Hussain N. Decompressive craniectomy in cerebral toxoplasmosis. Eur J Clin Microbiol Infect Dis. 24:772–773. 2005.
Article2. Archavlis E, Carvi Y Nievas M. The impact of timing of cranioplasty in patients with large cranial defects after decompressive hemicraniectomy. Acta Neurochir (Wien). 154:1055–1062. 2012.
Article3. Beauchamp KM, Kashuk J, Moore EE, Bolles G, Rabb C, Seinfeld J, et al. Cranioplasty after postinjury decompressive craniectomy: is timing of the essence? J Trauma. 69:270–274. 2010.
Article4. Bruce JN, Bruce SS. Preservation of bone flaps in patients with postcraniotomy infections. J Neurosurg. 98:1203–1207. 2003.
Article5. Cabraja M, Klein M, Lehmann TN. Long-term results following titanium cranioplasty of large skull defects. Neurosurg Focus. 26:E10. 2009.
Article6. Chang V, Hartzfeld P, Langlois M, Mahmood A, Seyfried D. Outcomes of cranial repair after craniectomy. J Neurosurg. 112:1120–1124. 2010.
Article7. Cronquist AB, Jakob K, Lai L, Della Latta P, Larson EL. Relationship between skin microbial counts and surgical site infection after neurosurgery. Clin Infect Dis. 33:1302–1308. 2001.
Article8. Dujovny M, Aviles A, Agner C, Fernandez P, Charbel FT. Cranioplasty: cosmetic or therapeutic? Surg Neurol. 47:238–241. 1997.
Article9. Dünisch P, Walter J, Sakr Y, Kalff R, Waschke A, Ewald C. Risk factors of aseptic bone resorption: a study after autologous bone flap reinsertion due to decompressive craniotomy. J Neurosurg. 118:1141–1147. 2013.
Article10. Ferro JM, Crassard I, Coutinho JM, Canhão P, Barinagarrementeria F, Cucchiara B, et al. Decompressive surgery in cerebrovenous thrombosis: a multicenter registry and a systematic review of individual patient data. Stroke. 42:2825–2831. 2011.11. Fisher CM, Ojemann RG. Bilateral decompressive craniectomy for worsening coma in acute subarachnoid hemorrhage. Observations in support of the procedure. Surg Neurol. 41:65–74. 1994.
Article12. Gooch MR, Gin GE, Kenning TJ, German JW. Complications of cranioplasty following decompressive craniectomy: analysis of 62 cases. Neurosurg Focus. 26:E9. 2009.
Article13. Grant GA, Jolley M, Ellenbogen RG, Roberts TS, Gruss JR, Loeser JD. Failure of autologous bone-assisted cranioplasty following decompressive craniectomy in children and adolescents. J Neurosurg. 100 (2 Suppl Pediatrics):163–168. 2004.
Article14. Honeybul S. Complications of decompressive craniectomy for head injury. J Clin Neurosci. 17:430–435. 2010.
Article15. Honeybul S, Ho KM. How “successful” is calvarial reconstruction using frozen autologous bone? Plast Reconstr Surg. 130:1110–1117. 2012.
Article16. Honeybul S, Ho KM. Long-term complications of decompressive craniectomy for head injury. J Neurotrauma. 28:929–935. 2011.
Article17. Honeybul S, Ho KM. The current role of decompressive craniectomy in the management of neurological emergencies. Brain Inj. 27:979–991. 2013.
Article18. Kim BJ, Hong KS, Park KJ, Park DH, Chung YG, Kang SH. Customized cranioplasty implants using three-dimensional printers and polymethylmethacrylate casting. J Korean Neurosurg Soc. 52:541–546. 2012.
Article19. Lee SC, Wu CT, Lee ST, Chen PJ. Cranioplasty using polymethyl methacrylate prostheses. J Clin Neurosci. 16:56–63. 2009.
Article20. Malis LI. Titanium mesh and acrylic cranioplasty. Neurosurgery. 25:351–355. 1989.
Article21. Marbacher S, Andres RH, Fathi AR, Fandino J. Primary reconstruction of open depressed skull fractures with titanium mesh. J Craniofac Surg. 19:490–495. 2008.
Article22. Matsuno A, Tanaka H, Iwamuro H, Takanashi S, Miyawaki S, Nakashima M, et al. Analyses of the factors influencing bone graft infection after delayed cranioplasty. Acta Neurochir (Wien). 148:535–540. discussion 540. 2006.
Article23. Piedra MP, Nemecek AN, Ragel BT. Timing of cranioplasty after decompressive craniectomy for trauma. Surg Neurol Int. 5:25. 2014.
Article24. Polin RS, Shaffrey ME, Bogaev CA, Tisdale N, Germanson T, Bocchicchio B, et al. Decompressive bifrontal craniectomy in the treatment of severe refractory posttraumatic cerebral edema. Neurosurgery. 41:84–92. discussion 92-94. 1997.
Article25. Reddy S, Khalifian S, Flores JM, Bellamy J, Manson PN, Rodriguez ED, et al. Clinical outcomes in cranioplasty: risk factors and choice of reconstructive material. Plast Reconstr Surg. 133:864–873. 2014.26. Riordan MA, Simpson VM, Hall WA. Analysis of factors contributing to infections after cranioplasty: a single-institution retrospective chart review. World Neurosurg. 87:207–213. 2016.
Article27. Schuss P, Vatter H, Oszvald A, Marquardt G, Imöhl L, Seifert V, et al. Bone flap resorption: risk factors for the development of a long-term complication following cranioplasty after decompressive craniectomy. J Neurotrauma. 30:91–95. 2013.
Article28. Schwab S, Steiner T, Aschoff A, Schwarz S, Steiner HH, Jansen O, et al. Early hemicraniectomy in patients with complete middle cerebral artery infarction. Stroke. 29:1888–1893. 1998.
Article29. Segal DH, Oppenheim JS, Murovic JA. Neurological recovery after cranioplasty. Neurosurgery. 34:729–731. discussion 731. 1994.
Article30. Sundseth J, Sundseth A, Berg-Johnsen J, Sorteberg W, Lindegaard KF. Cranioplasty with autologous cryopreserved bone after decompressive craniectomy: complications and risk factors for developing surgical site infection. Acta Neurochir (Wien). 156:805–811. discussion 811. 2014.
Article31. Thavarajah D, De Lacy P, Hussien A, Sugar A. The minimum time for cranioplasty insertion from craniectomy is six months to reduce risk of infection--a case series of 82 patients. Br J Neurosurg. 26:78–80. 2012.
Article32. Wiggins A, Austerberry R, Morrison D, Ho KM, Honeybul S. Cranioplasty with custom-made titanium plates--14 years experience. Neurosurgery. 72:248–256. discussion 256. 2013.
Article33. Wind JJ, Ohaegbulam C, Iwamoto FM, Black PM, Park JK. Immediate titanium mesh cranioplasty for treatment of postcraniotomy infections. World Neurosurg. 79:207. e11-e13. 2013.
Article34. Yadla S, Campbell PG, Chitale R, Maltenfort MG, Jabbour P, Sharan AD. Effect of early surgery, material, and method of flap preservation on cranioplasty infections: a systematic review. Neurosurgery. 68:1124–1129. discussion 1130. 2011.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Temporal Hollowing Augmentation with Titanium Mesh after Autologous Cranioplasty in Temporal Muscle Resected Case: A Case Report
- Outcomes of Cranioplasty Using Autologous Bone or 3D-Customized Titanium Mesh Following Decompressive Craniectomy for Traumatic Brain Injury: Differences in Complications
- Efficacy of 3D-Printed Titanium Mesh-Type Patient-Specific Implant for Cranioplasty
- Comparison of Porous Polyethylene Sheet(Medpor(R)) with Titanium Dynamic Mesh in the Treatment of Blow Out Fracture
- Repetitive Exposure of Titanium Mesh after Cranioplasty: A Case Report