Are Lung Imaging Reporting and Data System Categories Clear to Radiologists? A Survey of the Korean Society of Thoracic Radiology Members on Ten Difficult-to-Classify Scenarios
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 06591, Korea.
- 2Department of Radiology, Seoul National University College of Medicine, Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul 03080, Korea.
- 3Cancer Research Institute, Seoul National University, Seoul 03080, Korea.
- 4Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul 06973, Korea.
- KMID: 2427953
- DOI: http://doi.org/10.3348/kjr.2017.18.2.402
Abstract
OBJECTIVE
To evaluate possible variability in chest radiologists' interpretations of the Lung Imaging Reporting and Data System (Lung-RADS) on difficult-to-classify scenarios.
MATERIALS AND METHODS
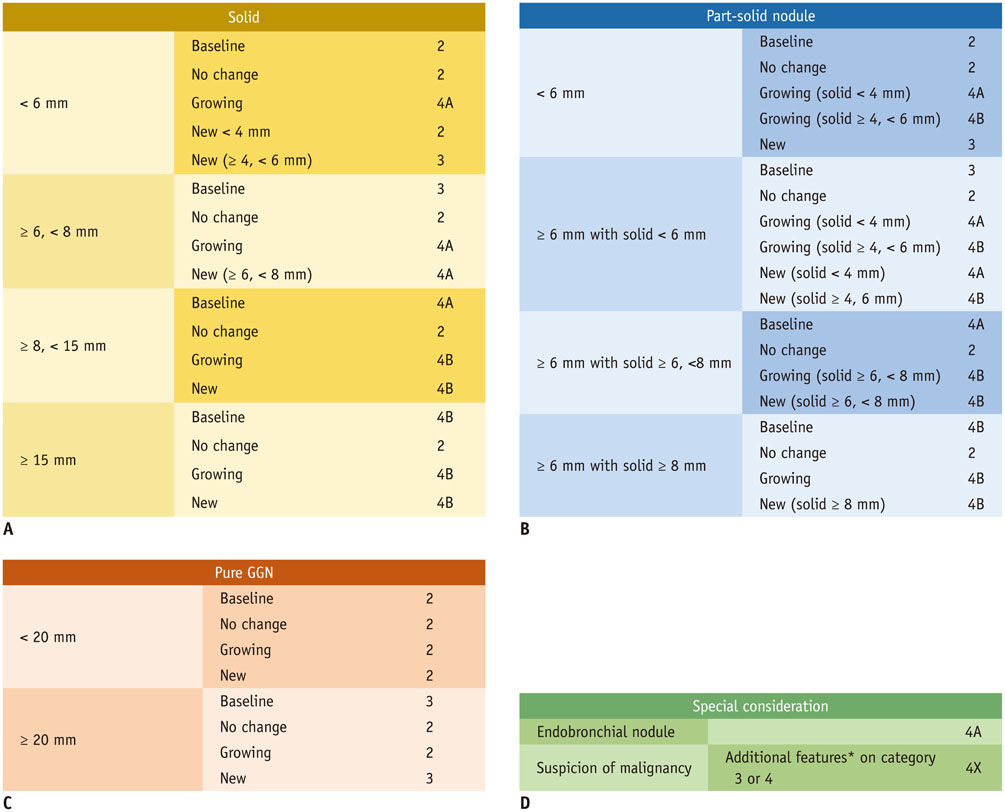
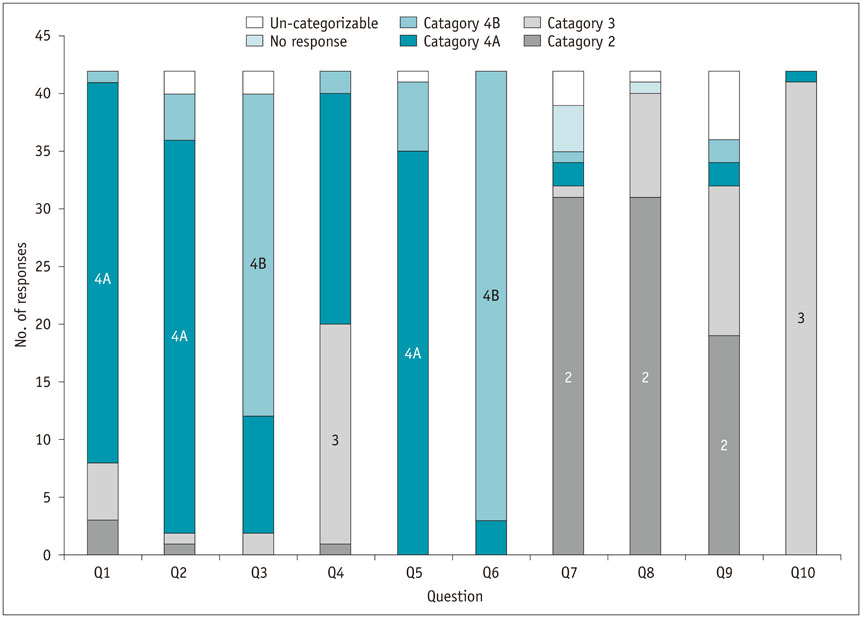
Ten scenarios of difficult-to-classify imaginary lung nodules were prepared as an online survey that targeted Korean Society of Thoracic Radiology members. In each question, a description was provided of the size, consistency, and interval change (new or growing) of a lung nodule observed using annual repeat computed tomography, and the respondent was instructed to choose one answer from five choices: category 2, 3, 4A, or 4B, or "un-categorizable." Consensus answers were established by members of the Korean Imaging Study Group for Lung Cancer.
RESULTS
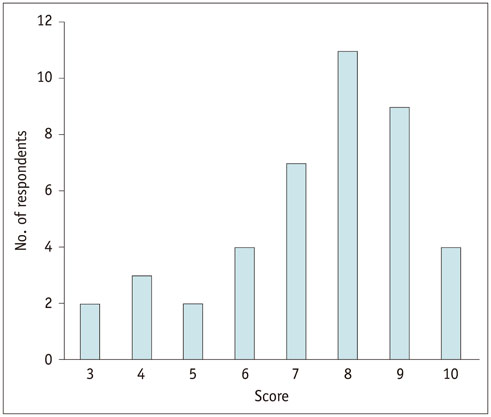
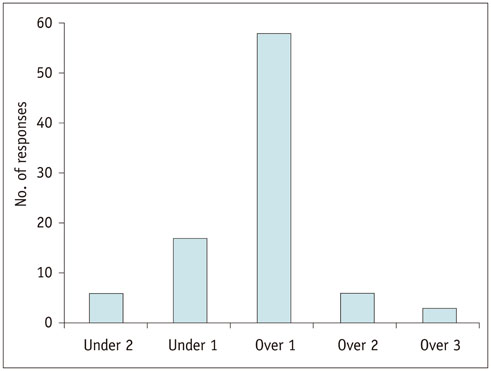
Of the 420 answers from 42 respondents (excluding multiple submissions), 310 (73.8%) agreed with the consensus answers; eleven (26.2%) respondents agreed with the consensus answers to six or fewer questions. Assigning the imaginary nodules to categories higher than the consensus answer was more frequent (16.0%) than assigning them to lower categories (5.5%), and the agreement rate was below 50% for two scenarios.
CONCLUSION
When given difficult-to-classify scenarios, chest radiologists showed large variability in their interpretations of the Lung-RADS categories, with high frequencies of disagreement in some specific scenarios.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Radiological Report of Pilot Study for the Korean Lung Cancer Screening (K-LUCAS) Project: Feasibility of Implementing Lung Imaging Reporting and Data System
Ji Won Lee, Hyae Young Kim, Jin Mo Goo, Eun Young Kim, Soo Jung Lee, Tae Jung Kim, Yeol Kim, Juntae Lim
Korean J Radiol. 2018;19(4):803-808. doi: 10.3348/kjr.2018.19.4.803.A Survey of Institutions with Sixteen Detector-Rows or More CT Scanners for the Introduction of National Lung Cancer Screening Program Using Low-Dose Chest CT
Jae Gu Oh, Sang Hyun Paik, Beom Suck Kim, Jae Myeong Lee, Jin Mo Goo
J Korean Soc Radiol. 2017;77(6):404-411. doi: 10.3348/jksr.2017.77.6.404.National Lung Cancer Screening in Korea: Introduction and Imaging Quality Control
Hyae Young Kim
J Korean Soc Radiol. 2019;80(5):826-836. doi: 10.3348/jksr.2019.80.5.826.
Reference
-
1. National Lung Screening Trial Research Team. Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011; 365:395–409.2. Jaklitsch MT, Jacobson FL, Austin JH, Field JK, Jett JR, Keshavjee S, et al. The American Association for Thoracic Surgery guidelines for lung cancer screening using low-dose computed tomography scans for lung cancer survivors and other high-risk groups. J Thorac Cardiovasc Surg. 2012; 144:33–38.3. Detterbeck FC, Mazzone PJ, Naidich DP, Bach PB. Screening for lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143:5 Suppl. e78S–e92S.4. Canadian Task Force on Preventive Health Care. Lewin G, Morissette K, Dickinson J, Bell N, Bacchus M, et al. Recommendations on screening for lung cancer. CMAJ. 2016; 188:425–432.5. Wood DE. National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines for Lung Cancer Screening. Thorac Surg Clin. 2015; 25:185–197.6. de Koning HJ, Meza R, Plevritis SK, ten Haaf K, Munshi VN, Jeon J, et al. Benefits and harms of computed tomography lung cancer screening strategies: a comparative modeling study for the US Preventive Services Task Force. Ann Intern Med. 2014; 160:311–320.7. Decision Memo for Screening for Lung Cancer with Low Dose Computed Tomography (LDCT) (CAG-00439N). Web site. Accessed June 3, 2016. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=274.8. Lung CT Screening Reporting and Data System (Lung-RADS™). Web site. Accessed June 3, 2016. https://www.acr.org/Quality-Safety/Resources/LungRADS.9. Pinsky PF, Gierada DS, Black W, Munden R, Nath H, Aberle D, et al. Performance of Lung-RADS in the National Lung Screening Trial: a retrospective assessment. Ann Intern Med. 2015; 162:485–491.10. McKee BJ, Regis SM, McKee AB, Flacke S, Wald C. Performance of ACR Lung-RADS in a clinical CT lung screening program. J Am Coll Radiol. 2015; 12:273–276.11. Grimshaw JM, Hutchinson A. Clinical practice guidelines--do they enhance value for money in health care? Br Med Bull. 1995; 51:927–940.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lung Imaging Reporting and Data System (Lung-RADS) in Radiology: Strengths, Weaknesses and Improvement
- Breast Imaging Reporting and Data System (BI-RADS): Advantages and Limitations
- Thyroid Imaging Reporting and Data System (TIRADS)
- Liver imaging reporting and data system (LI-RADS) version 2014: understanding and application of the diagnostic algorithm
- National Lung Cancer Screening in Korea: Introduction and Imaging Quality Control