Korean J Radiol.
2017 Apr;18(2):299-308. 10.3348/kjr.2017.18.2.299.
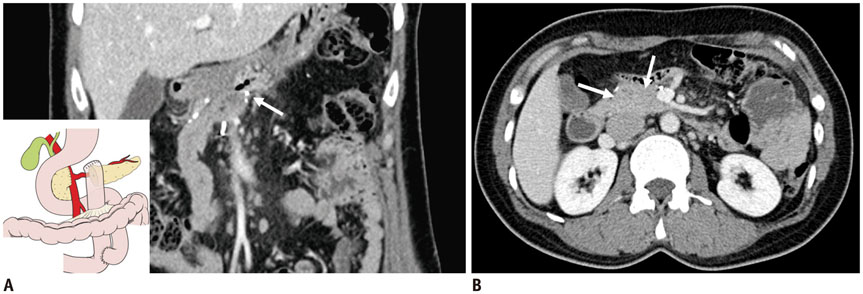
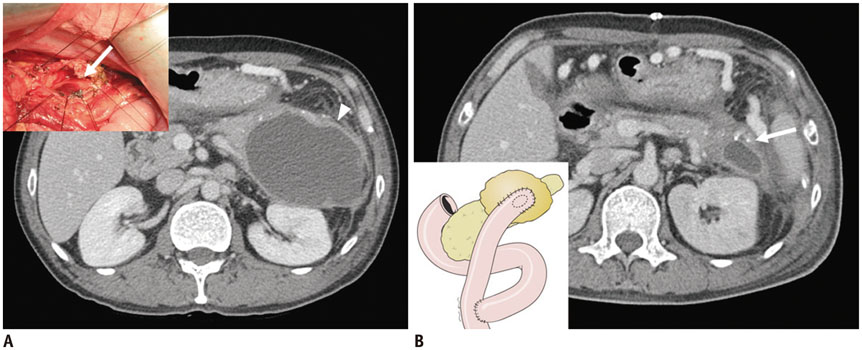
Normal Postoperative Computed Tomography Findings after a Variety of Pancreatic Surgeries
- Affiliations
-
- 1Department of Radiology, Severance Hospital, Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul 03722, Korea. yelv@yuhs.ac
- 2Department of Surgery, Yonsei University College of Medicine, Seoul 03722, Korea.
- KMID: 2427942
- DOI: http://doi.org/10.3348/kjr.2017.18.2.299
Abstract
- Pancreatic surgery remains the only curative treatment for pancreatic neoplasms, and plays an important role in the management of medically intractable diseases. Since the original Whipple operation in the 20th century, surgical techniques have advanced, resulting in decreased postoperative complications and better clinical outcomes. Normal postoperative imaging findings vary greatly depending on the surgical technique used. Radiologists are required to be familiar with the normal postoperative imaging findings, in order to distinguish from postoperative complications or tumor recurrence. In this study, we briefly review a variety of surgical techniques for the pancreas, and present the normal postoperative computed tomography findings.
MeSH Terms
Figure
Cited by 1 articles
-
Measurement of Pancreatic Fat Fraction by CT Histogram Analysis to Predict Pancreatic Fistula after Pancreaticoduodenectomy
Wonju Hong, Hong Il Ha, Jung Woo Lee, Sang Min Lee, Min-Jeong Kim
Korean J Radiol. 2019;20(4):599-608. doi: 10.3348/kjr.2018.0557.
Reference
-
1. Ozawa F, Friess H, Künzli B, Shrikhande SV, Otani T, Makuuchi M, et al. Treatment of pancreatic cancer: the role of surgery. Dig Dis. 2001; 19:47–56.2. Strasberg SM, Drebin JA, Linehan D. Radical antegrade modular pancreatosplenectomy. Surgery. 2003; 133:521–527.3. Roggin KK, Rudloff U, Blumgart LH, Brennan MF. Central pancreatectomy revisited. J Gastrointest Surg. 2006; 10:804–812.4. Ho CK, Kleeff J, Friess H, Büchler MW. Complications of pancreatic surgery. HPB (Oxford). 2005; 7:99–108.5. Casadei R, Ricci C, Antonacci N, Minni F. Indications and technique of central pancreatectomy. In : Siquini W, editor. Surgical treatment of pancreatic disease. Milan: Springer Milan;2009. p. 329–336.6. Kim MJ, Choi JY, Chung YE. Evaluation of biliary malignancies using multidetector-row computed tomography. J Comput Assist Tomogr. 2010; 34:496–505.7. Bhosale P, Fleming J, Balachandran A, Charnsangavej C, Tamm EP. Complications of Whipple surgery: imaging analysis. Abdom Imaging. 2013; 38:273–284.8. Diener MK, Fitzmaurice C, Schwarzer G, Seiler CM, Hüttner FJ, Antes G, et al. Pylorus-preserving pancreaticoduodenectomy (pp Whipple) versus pancreaticoduodenectomy (classic Whipple) for surgical treatment of periampullary and pancreatic carcinoma. Cochrane Database Syst Rev. 2014; (11):CD006053.9. Yamauchi FI, Ortega CD, Blasbalg R, Rocha MS, Jukemura J, Cerri GG. Multidetector CT evaluation of the postoperative pancreas. Radiographics. 2012; 32:743–764.10. Poon RT, Lo SH, Fong D, Fan ST, Wong J. Prevention of pancreatic anastomotic leakage after pancreaticoduodenectomy. Am J Surg. 2002; 183:42–52.11. Kennedy EP, Yeo CJ. Dunking pancreaticojejunostomy versus duct-to-mucosa anastomosis. J Hepatobiliary Pancreat Sci. 2011; 18:769–774.12. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13.13. El Nakeeb A, El Hemaly M, Askr W, Abd Ellatif M, Hamed H, Elghawalby A, et al. Comparative study between duct to mucosa and invagination pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized study. Int J Surg. 2015; 16(Pt A):1–6.14. Bassi C, Falconi M, Molinari E, Mantovani W, Butturini G, Gumbs AA, et al. Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: results of a prospective randomized trial. Surgery. 2003; 134:766–771.15. Raman SP, Horton KM, Cameron JL, Fishman EK. CT after pancreaticoduodenectomy: spectrum of normal findings and complications. AJR Am J Roentgenol. 2013; 201:2–13.16. Ben-Ishay O, Assi Z, Kluger Y. Pancreaticojejunostomy: images of an invagination technique. JOP. 2010; 11:642–643.17. Lepanto L, Gianfelice D, Déry R, Dagenais M, Lapointe R, Roy A. Postoperative changes, complications, and recurrent disease after Whipple's operation: CT features. AJR Am J Roentgenol. 1994; 163:841–846.18. Zhu F, Wang M, Wang X, Tian R, Shi C, Xu M, et al. Modified technique of pancreaticogastrostomy for soft pancreas with two continuous hemstitch sutures: a single-center prospective study. J Gastrointest Surg. 2013; 17:1306–1311.19. Xiong JJ, Tan CL, Szatmary P, Huang W, Ke NW, Hu WM, et al. Meta-analysis of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Br J Surg. 2014; 101:1196–1208.20. Tamm EP, Jones B, Yeo CJ, Maher MM, Cameron JL. Pancreaticogastrostomy and the Whipple procedure: radiographic appearance and complications. Radiology. 1995; 196:251–255.21. Parikh PY, Lillemoe KD. Surgical management of pancreatic cancer--distal pancreatectomy. Semin Oncol. 2015; 42:110–122.22. Trottman P, Swett K, Shen P, Sirintrapun J. Comparison of standard distal pancreatectomy and splenectomy with radical antegrade modular pancreatosplenectomy. Am Surg. 2014; 80:295–300.23. Strasberg SM, Fields R. Left-sided pancreatic cancer: distal pancreatectomy and its variants: radical antegrade modular pancreatosplenectomy and distal pancreatectomy with celiac axis resection. Cancer J. 2012; 18:562–570.24. Warshaw AL. Distal pancreatectomy with preservation of the spleen. J Hepatobiliary Pancreat Sci. 2010; 17:808–812.25. Ferrone CR, Konstantinidis IT, Sahani DV, Wargo JA, Fernandez-del Castillo C, Warshaw AL. Twenty-three years of the Warshaw operation for distal pancreatectomy with preservation of the spleen. Ann Surg. 2011; 253:1136–1139.26. Crippa S, Tamburrino D, Partelli S, Salvia R, Germenia S, Bassi C, et al. Total pancreatectomy: indications, different timing, and perioperative and long-term outcomes. Surgery. 2011; 149:79–86.27. Santoro R. Total pancreatectomy: indications, technique, and postoperative problems. In : Siquini W, editor. Surgical treatment of pancreatic disease. Milan: Springer Milan;2009. p. 337–348.28. Gavazzi F, Zerbi A, Di Carlo V. Indications for surgery and surgical procedures for chronic pancreatitis. In : Siquini W, editor. Surgical treatment of pancreatic disease. Milan: Springer Milan;2009. p. 127–137.29. Aghdassi AA, Mayerle J, Kraft M, Sielenkämper AW, Heidecke CD, Lerch MM. Pancreatic pseudocysts--when and how to treat? HPB (Oxford). 2006; 8:432–441.30. Maithel SK, Fong Y. Technical aspects of performing transduodenal ampullectomy. J Gastrointest Surg. 2008; 12:1582–1585.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Computed Tomography in Traumatic Injury of Pancreas
- Pancreatic Tumors: Emphasis on CT Findings and Pathologic Classification
- CT Findings of Normal Pancreatic Tail: Variety of Morphology and Location
- A Case of Pancreatic Pseudocyst in the Left Hepatic Lobe
- Pancreas Neuroendocrine Tumor and Its Mimics: Review of Cross-Sectional Imaging Findings for Differential Diagnosis