Arch Hand Microsurg.
2018 Dec;23(4):290-295. 10.12790/ahm.2018.23.4.290.
Survival of Neuro-Venous Flap without Perforator due to Accidental Division of Perforator
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea. medi619@hanmail.net
- KMID: 2427397
- DOI: http://doi.org/10.12790/ahm.2018.23.4.290
Abstract
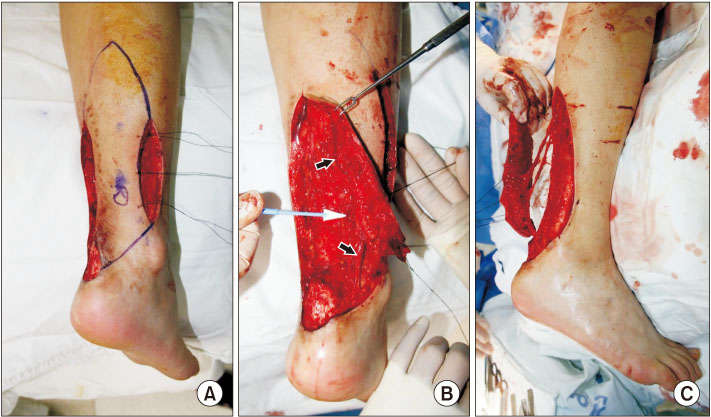
- Author planed peroneal artery perforator flap for ankle reconstruction and experienced successful result using sural neuro-lesser saphenous venous flap due to an unexpected event. A male Asian patient, 24 years old, had a history of recurrent operation wound disruption in the ankle region. Under general anesthesia, peroneal perforator and saphenous vein, as well as the sural nerve branches, were identified and preserved. In the process of flap rotation, an accidental division of peroneal artery perforator has occurred. Despite the division of the perforator, circulation was normal. The patient experienced no complication after the surgery. Some study reported that accompanying arteries and the vascular plexus around the sural nerve communicate. In conclusion, sufficient blood supply was possible only with the accompanying artery of the sural nerve without peroneal perforator. So, it is essential to always preserve not only perforator but also neurovascular bundles at any circumstances and any location.
MeSH Terms
Figure
Reference
-
1. Guiraldo RPA, Cabral CM, Nora RT, Gasques JAL, Bozola AR. Severe lower limb trauma. Rev Bras Cir Plást. 2013; 28:320–323.2. Khurram MF, Ahmad I, Nanda M. Soft tissue reconstruction of foot and ankle defects: free vs pedicled flaps with the use of 6 different flaps in 50 cases of road traffic accidents. Austin J Surg. 2014; 1:1031.3. Pontén B. The fasciocutaneous flap: its use in soft tissue defects of the lower leg. Br J Plast Surg. 1981; 34:215–220.
Article4. Harrison DH, Morgan BD. The instep island flap to resurface plantar defects. Br J Plast Surg. 1981; 34:315–318.
Article5. Masquelet AC, Romanan MC, Wolf G. Skin island flap supplied by the vascular axis of the sensitive superficial nerves: anatomic study and clinical experience in the leg. Plast Reconstr Surg. 1992; 89:1115–1121.6. Yilmaz M, Karatas O, Barutcu A. The distally based superficial sural artery island flap: clinical experiences and modifications. Plast Reconstr Surg. 1998; 102:2358–2367.
Article7. Serafin D, Georgiade NG, Smith DH. Comparison of free flap with pedicled flaps for coverage of defects of the leg or foot. Plast Reconstr Surg. 1977; 59:492–499.8. Sladjana UZ, Ivan JD, Ljiljana VP, Natalija SJ, Predrag KT, Vesna SR. Neurovascular stalk of the superficial sural flap: human fetus anatomical study. Plast Reconstr Surg. 2005; 116:546–550.
Article9. Oberlin C, Azoulay B, Bhatia A. The posterolateral malleolar flap of the ankle: a distally based sural neurocutaneous flap--report of 14 cases. Plast Reconstr Surg. 1995; 96:400–405. discussion 406-7.10. Lee HI, Ha SH, Yu SO, Park MJ, Chae SH, Lee GJ. Reverse sural artery island flap with skin extension along the pedicle. J Foot Ankle Surg. 2016; 55:470–475.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Flap thinning: Defatting after conventional elevation
- Dual Perforator Flap for Reconstruction of Large Sacral Defects: Superior Gluteal Artery Perforator Super-Flap with Parasacral Perforator
- Reconstruction of the Soft Tissue Defect Using Thoracodorsal Artery Perforator Skin Flap
- Bilateral Vulvar Reconstruction Using Two Different Types of Perforator Flap: A Case Report
- Perforator Reconstruction to Salvage the Jeopardized Flaps