Ann Hepatobiliary Pancreat Surg.
2018 Nov;22(4):359-366. 10.14701/ahbps.2018.22.4.359.
Robot resection of a choledochal cyst with Roux-en-y hepaticojejunostomy in adults: Initial experiences with 22 cases and a comparison with laparoscopic approaches
- Affiliations
-
- 1Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. hbpsurgeon@gmail.com
- KMID: 2427367
- DOI: http://doi.org/10.14701/ahbps.2018.22.4.359
Abstract
- BACKGROUNDS/AIMS
In adult choledochal cysts, complete excision of cyst with Roux-en-Y hepaticojejunostomy by laparoscopy is typically been performed, but there is now a trend towards adopting robot-assisted resection.
METHODS
From January 2014 to December 2017, 22 patients who underwent robotic procedure were classified as Group 1, and 34 patients who underwent the same laparoscopic procedure as Group 2. In addition, from September 2009 to July 2011, 13 patients who underwent laparoscopic procedure were classified as Group 3. The perioperative outcomes and short-term postoperative morbidity levels were evaluated in three groups.
RESULTS
In all groups, there were more women than men, and the mean age and BMI did not differ significantly. Since 2014, jejunojejunostomy was performed extracorporeally and the mean operation time was shorter in Group 1 (258.5±52.9 min) and Group 2 (236.2±62.9 min) than Group 3 (395.2±85.9 min). [p=0.00 (1 vs 3), 0.00 (2 vs 3)] The median hospital stay was 7 days in Group 1 and 2, and shorter than 9 days in Group 3. [p=0.00 (1 vs 3), 0.011 (2 vs 3)] In Group 1, there were three postoperative complications, which included cholangitis, bile leakage and umbilical herniation, respectively). In Group 2, there were seven of postoperative complications, which included choledochojejunostomy site stricture & intrahepatic duct stone, choledochojejunostomy site stone, jejunal branch bleeding, portal vein thrombus, acute pancreatitis, adhesive ileus, and A-loop syndrome. In Group 3, there were three of postoperative complications, which included 2 hepaticojejunostomy site stricture and 1 paralytic ileus.
CONCLUSIONS
Robot-assisted resection of a choledochal cyst with Roux-en-y hepaticojejunostomy is a safe and feasible approach with short-term results that are comparable to those of laparoscopic surgery.
MeSH Terms
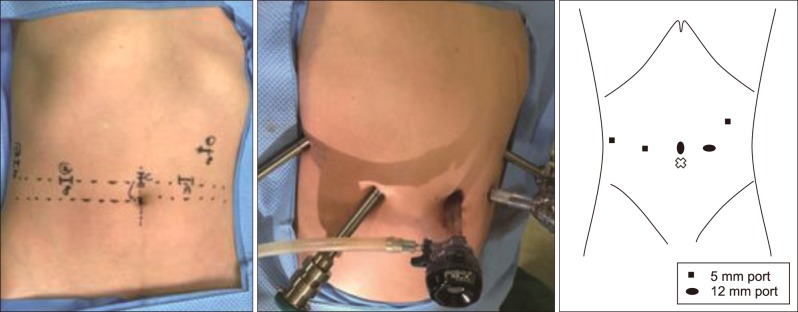
Figure
Cited by 3 articles
-
Minimally invasive surgery for choledochal cysts: Laparoscopic versus robotic approaches
Jong Hwi Yoon, Ho Kyoung Hwang, Woo Jung Lee, Chang Moo Kang
Ann Hepatobiliary Pancreat Surg. 2021;25(1):71-77. doi: 10.14701/ahbps.2021.25.1.71.Development of adenocarcinoma at the remnant intrapancreatic cyst 16 years after resection of the choledochal cyst
Soo Young Oh, Jae Hyun Kwon, Shin Hwang
Ann Hepatobiliary Pancreat Surg. 2019;23(2):192-196. doi: 10.14701/ahbps.2019.23.2.192.A case of laparoscopic excision of choledochal cyst, hepaticojejunostomy, and Roux-en-Y anastomosis using Artisential®
Younghoon Shim, Chang Moo Kang
Ann Hepatobiliary Pancreat Surg. 2024;28(2):266-269. doi: 10.14701/ahbps.23-114.
Reference
-
1. Dumitrascu T, Lupescu I, Ionescu M. The Todani classification for bile duct cysts: an overview. Acta Chir Belg. 2012; 112:340–345. PMID: 23175921.
Article2. Kim OH, Chung HJ, Choi BG. Imaging of the choledochal cyst. Radiographics. 1995; 15:69–88. PMID: 7899614.
Article3. Wiseman K, Buczkowski AK, Chung SW, Francoeur J, Schaeffer D, Scudamore CH. Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg. 2005; 189:527–531. PMID: 15862490.
Article4. Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, et al. Choledochal cysts: presentation, clinical differentiation, and management. J Am Coll Surg. 2014; 219:1167–1180. PMID: 25442379.
Article5. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977; 134:263–269. PMID: 889044.6. Huang CS, Huang CC, Chen DF. Choledochal cysts: differences between pediatric and adult patients. J Gastrointest Surg. 2010; 14:1105–1110. PMID: 20422306.
Article7. Stain SC, Guthrie CR, Yellin AE, Donovan AJ. Choledochal cyst in the adult. Ann Surg. 1995; 222:128–133. PMID: 7639580.
Article8. Song HK, Kim MH, Myung SJ, Lee SK, Kim HJ, Yoo KS, et al. Choledochal cyst associated the with anomalous union of pancreaticobiliary duct (AUPBD) has a more grave clinical course than choledochal cyst alone. Korean J Intern Med. 1999; 14:1–8.
Article9. Jan YY, Chen HM, Chen MF. Malignancy in choledochal cysts. Hepatogastroenterology. 2002; 49:100–103. PMID: 11941929.10. Tsai MS, Lin WH, Hsu WM, Lai HS, Lee PH, Chen WJ. Clinicopathological feature and surgical outcome of choledochal cyst in different age groups: the implication of surgical timing. J Gastrointest Surg. 2008; 12:2191–2195. PMID: 18677540.
Article11. Farello GA, Cerofolini A, Rebonato M, Bergamaschi G, Ferrari C, Chiappetta A. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc. 1995; 5:354–358. PMID: 8845978.12. Ballantyne GH, Moll F. The da Vinci telerobotic surgical system: the virtual operative field and telepresence surgery. Surg Clin North Am. 2003; 83:1293–1304. vii. PMID: 14712866.
Article13. Lanfranco AR, Castellanos AE, Desai JP, Meyers WC. Robotic surgery: a current perspective. Ann Surg. 2004; 239:14–21. PMID: 14685095.14. Okada A, Hasegawa T, Oguchi Y, Nakamura T. Recent advances in pathophysiology and surgical treatment of congenital dilatation of the bile duct. J Hepatobiliary Pancreat Surg. 2002; 9:342–351. PMID: 12353145.
Article15. Kimura W. Congenital dilatation of the common bile duct and pancreaticobiliary maljunction: clinical implications. Langenbecks Arch Surg. 2009; 394:209–213. PMID: 18712411.16. Hwang DW, Lee JH, Lee SY, Song DK, Hwang JW, Park KM, et al. Early experience of laparoscopic complete en bloc excision for choledochal cysts in adults. Surg Endosc. 2012; 26:3324–3329. PMID: 22549376.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Initial Experience of Robot-assisted Resection of Choledochal Cyst in Children
- A case of laparoscopic excision of choledochal cyst, hepaticojejunostomy, and Roux-en-Y anastomosis using Artisential®
- Comparison of surgical outcomes of intracorporeal hepaticojejunostomy in the excision of choledochal cysts using laparoscopic versus robot techniques
- Robot-assisted Excision of a Huge Choledochal Cyst and Roux-en-Y Hepaticojejunostomy using the da Vinci(TM) Surgical System
- Long-term Results of Roux-en-Y Procedure in Choledochal Cyst and in Cholelithiasis