Clin Orthop Surg.
2018 Dec;10(4):433-438. 10.4055/cios.2018.10.4.433.
The Prevalence of Cervical Foraminal Stenosis on Computed Tomography of a Selected Community-Based Korean Population
- Affiliations
-
- 1Department of Orthopaedic Surgery, Daegu Catholic University Medical Center, Daegu, Korea. bong@cu.ac.kr
- KMID: 2426528
- DOI: http://doi.org/10.4055/cios.2018.10.4.433
Abstract
- BACKGROUND
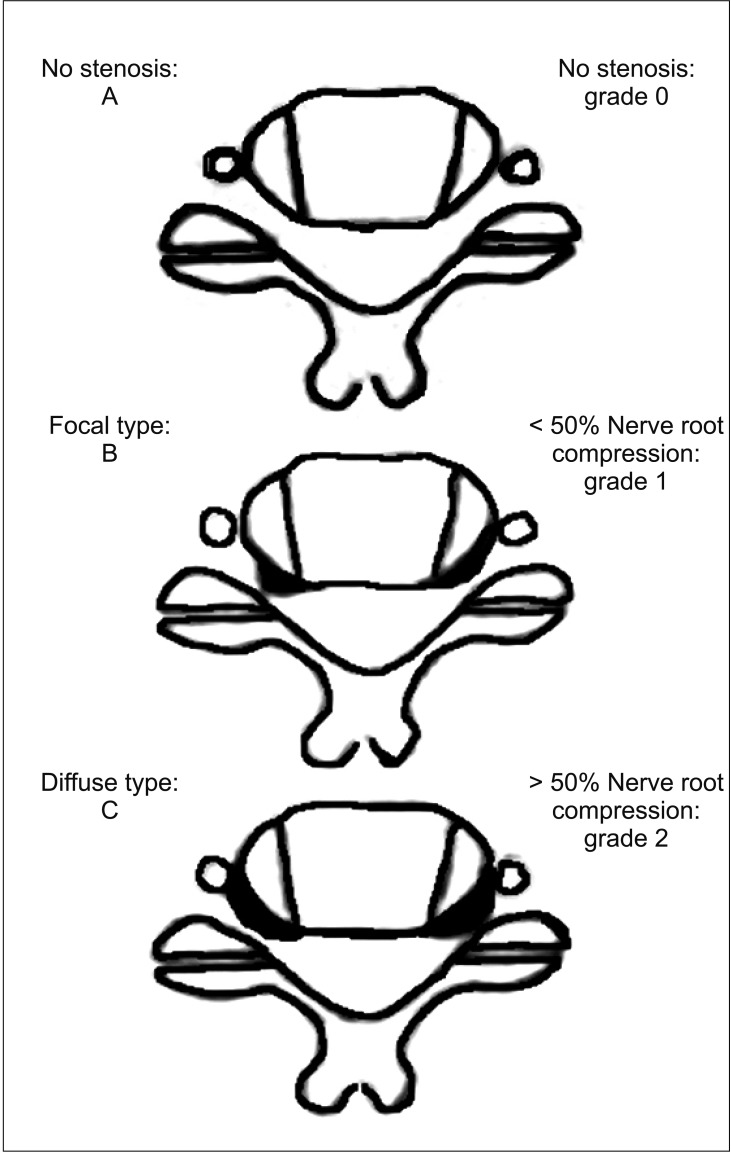
Cervical foraminal stenosis (CFS) is one of the degenerative changes of the cervical spine; however, correlations between the severity of stenosis and that of symptoms are not consistent in the literature. Studies to date on the prevalence of stenosis are based on images obtained from the departments treating cervical lesions, and thus patient selection bias may have occurred. The purpose of this study was to investigate the prevalence of CFS according to the site, extent, and morphology of stenosis using cervical computed tomography (CT) images obtained from patients who were visiting not because of symptoms related to the cervical spine, cervical pain, or upper limb pain.
METHODS
Among patients who underwent CT from January 2016 to March 2016 for reasons other than cervical spine symptoms, a total of 438 subjects were enrolled, and 2,628 cervical disc images (C4-5, C5-6, and C6-7; left and right sides) were examined. Three orthopedic surgeons performed two measurements each at 4-week intervals. Values were used for analysis if matched by more than two surgeons; if no match was found, the median values were used for analysis. The left and right sides on the same axial image were independently classified.
RESULTS
Left C5-6 stenosis was most common (24.66%) among patients. At the left C6-7, there were 20 focal types and 33 diffuse types. At bilateral C4-5 and right C6-7, the focal type was more common, whereas at bilateral C5-6 and left C6-7, the diffuse type was more common. Age and the severity of stenosis showed statistically significant correlation at all cervical levels.
CONCLUSIONS
The prevalence of CFS was highest at the C5-6 level (19.06%). Compared to other levels, focal stenosis was more frequent at C4-5 and diffuse stenosis was more common at C5-6. At C6-7, the incidence of focal stenosis was higher on the right side and that of diffuse stenosis was higher on the left side.
MeSH Terms
Figure
Reference
-
1. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg Am. 1990; 72(3):403–408. PMID: 2312537.
Article2. Matsumoto M, Fujimura Y, Suzuki N, et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998; 80(1):19–24. PMID: 9460946.
Article3. Wilson JR, Barry S, Fischer DJ, et al. Frequency, timing, and predictors of neurological dysfunction in the nonmyelopathic patient with cervical spinal cord compression, canal stenosis, and/or ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976). 2013; 38(22 Suppl 1):S37–S54. PMID: 23963005.
Article4. Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 1986; 11(6):521–524. PMID: 3787320.
Article5. Kang Y, Lee JW, Koh YH, et al. New MRI grading system for the cervical canal stenosis. AJR Am J Roentgenol. 2011; 197(1):W134–W140. PMID: 21700974.
Article6. Bednarik J, Kadanka Z, Dusek L, et al. Presymptomatic spondylotic cervical myelopathy: an updated predictive model. Eur Spine J. 2008; 17(3):421–431.
Article7. de Oliveira Vilaca C, Orsini M, Leite MA, et al. Cervical spondylotic myelopathy: what the neurologist should know. Neurol Int. 2016; 8(4):6330. PMID: 27994827.
Article8. Sheikh Taha AM, Shue J, Lebl D, Girardi F. Considerations for prophylactic surgery in asymptomatic severe cervical stenosis: review article. HSS J. 2015; 11(1):31–35. PMID: 25737666.9. Fassett DR, Jeyamohan S, Harrop J. Asymptomatic cervical stenosis: to operate or not? Semin Spine Surg. 2007; 19(1):47–50.
Article10. Lee SH, Park SY, Wang JC, Kang KC, Hwang SP, Jang S. A comprehensive MRI classification system for cervical foraminal stenosis. Spine J. 2015; 15(10):S203.
Article11. Tanaka N, Fujimoto Y, An HS, Ikuta Y, Yasuda M. The anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spine. Spine (Phila Pa 1976). 2000; 25(3):286–291. PMID: 10703098.
Article12. Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy: a population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994; 117(Pt 2):325–335. PMID: 8186959.13. Kuijper B, Tans JT, Schimsheimer RJ, et al. Degenerative cervical radiculopathy: diagnosis and conservative treatment. A review. Eur J Neurol. 2009; 16(1):15–20. PMID: 19087147.
Article14. Kuijper B, Tans JT, van der, Nollet F, Lycklama A, de Visser M. Root compression on MRI compared with clinical findings in patients with recent onset cervical radiculopathy. J Neurol Neurosurg Psychiatry. 2011; 82(5):561–563. PMID: 21047885.
Article15. Nakashima H, Yukawa Y, Suda K, Yamagata M, Ueta T, Kato F. Abnormal findings on magnetic resonance images of the cervical spines in 1211 asymptomatic subjects. Spine (Phila Pa 1976). 2015; 40(6):392–398. PMID: 25584950.
Article16. Shigematsu H, Cheung JP, Mak KC, Bruzzone M, Luk KD. Cervical spinal canal stenosis first presenting after spinal cord injury due to minor trauma: an insight into the value of preventive decompression. J Orthop Sci. 2017; 22(1):22–26. PMID: 27713009.
Article17. Jensen MV, Tuchsen F, Orhede E. Prolapsed cervical intervertebral disc in male professional drivers in Denmark, 1981-1990: a longitudinal study of hospitalizations. Spine (Phila Pa 1976). 1996; 21(20):2352–2355. PMID: 8915070.18. van Rijn JC, Klemetso N, Reitsma JB, et al. Observer variation in the evaluation of lumbar herniated discs and root compression: spiral CT compared with MRI. Br J Radiol. 2006; 79(941):372–377. PMID: 16632616.
Article19. van Rijn JC, Klemetso N, Reitsma JB, et al. Observer variation in MRI evaluation of patients suspected of lumbar disk herniation. AJR Am J Roentgenol. 2005; 184(1):299–303. PMID: 15615992.
Article20. Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg Am. 1990; 72(8):1178–1184. PMID: 2398088.
Article21. Fortin J, Riethmiller DW, Vilensky JA. No clear winner in differing imaging modalities for cervical radiculopathy. Pain Physician. 2002; 5(3):285–287. PMID: 16902655.
Article22. Bartlett RJ, Hill CR, Gardiner E. A comparison of T2 and gadolinium enhanced MRI with CT myelography in cervical radiculopathy. Br J Radiol. 1998; 71(841):11–19. PMID: 9534693.
Article23. Birchall D, Connelly D, Walker L, Hall K. Evaluation of magnetic resonance myelography in the investigation of cervical spondylotic radiculopathy. Br J Radiol. 2003; 76(908):525–531. PMID: 12893693.
Article24. Kaiser JA, Holland BA. Imaging of the cervical spine. Spine (Phila Pa 1976). 1998; 23(24):2701–2712. PMID: 9879096.
Article25. Teresi LM, Lufkin RB, Reicher MA, et al. Asymptomatic degenerative disk disease and spondylosis of the cervical spine: MR imaging. Radiology. 1987; 164(1):83–88. PMID: 3588931.
Article26. Roh JS, Teng AL, Yoo JU, Davis J, Furey C, Bohlman HH. Degenerative disorders of the lumbar and cervical spine. Orthop Clin North Am. 2005; 36(3):255–262. PMID: 15950685.
Article27. Shim JH, Park CK, Lee JH, et al. A comparison of angled sagittal MRI and conventional MRI in the diagnosis of herniated disc and stenosis in the cervical foramen. Eur Spine J. 2009; 18(8):1109–1116. PMID: 19294432.
Article28. Bogduk N, Mercer S. Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech (Bristol, Avon). 2000; 15(9):633–648.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Imaging Grading Systems for Central Canal and Neural Foraminal Stenoses of the Lumbar and Cervical Spines With a Focus on the Lee Grading System
- Impact of Severe Cervical Foraminal Stenosis on Contralateral C7 Nerve Transfer Outcomes
- Comparison of the Morphometric Changes in the Cervical Foramen: Anterior Cervical Discectomy and Fusion versus Posterior Foraminotomy
- Novel Foraminal Expansion Technique
- Detection of Cervical Foraminal Stenosis from Oblique Radiograph Using Convolutional Neural Network Algorithm