Clin Orthop Surg.
2018 Dec;10(4):413-419. 10.4055/cios.2018.10.4.413.
Factors Affecting the Extent of Graft Tendon Synovialization after Double-Bundle Anterior Cruciate Ligament Reconstruction: Based on Second-Look Arthroscopic Findings
- Affiliations
-
- 1Department of Orthopaedic Surgery, Pohang St. Mary's Hospital, Pohang, Korea. scarpel@ymail.com
- KMID: 2426525
- DOI: http://doi.org/10.4055/cios.2018.10.4.413
Abstract
- BACKGROUND
We aimed to examine the factors that influence synovialization of the grafted tendon after double-bundle anterior cruciate ligament (ACL) reconstruction based on second-look arthroscopic findings.
METHODS
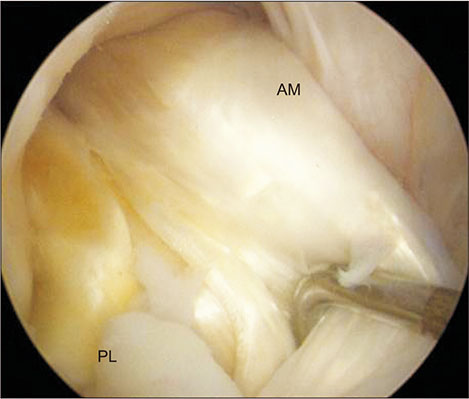
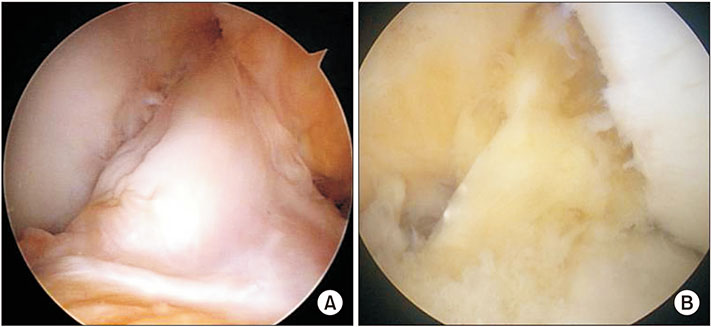
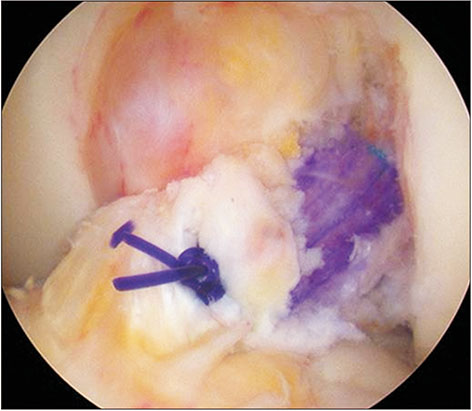
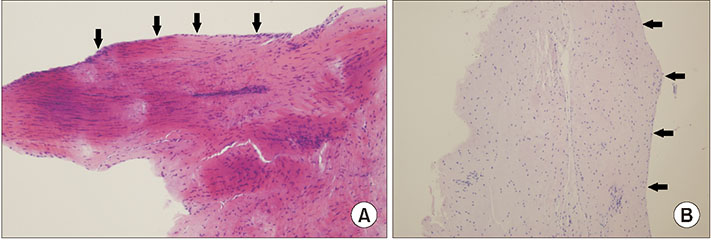
Out of 205 knees that were treated between August 2008 and May 2016 with double-bundle ACL reconstruction using bio-absorbable cross-pins and Endobuttons for femoral tunnel fixation, we enrolled 65 knees (64 patients) that underwent second-look arthroscopy with hardware removal at 1 year postoperatively. Measured clinical outcomes included the Lysholm score and Tegner activity score that were evaluated preoperatively and during the final follow-up. We analyzed the relationship between synovial coverage and patient age, length of the preserved remnant tissue on the tibial side, type of bundle (anteromedial or posterolateral), type of graft (autograft or allograft), and time from injury to surgery.
RESULTS
The area of synovial coverage showed a significant statistical correlation with patient age and the length of the preserved remnant tissue on the tibial side. The average synovial coverage was significantly better for the anteromedial bundle than for the posterolateral bundle, better for the autograft than for the allograft reconstruction, and better when treated in the acute stage than in the chronic stage. However, synovialization of grafted tendon did not correlate to clinical outcomes.
CONCLUSIONS
While we were able to identify several factors influencing synovialization of the grafted tendon after double-bundle ACL reconstruction, including patient age, length of preserved remnant tissue of the torn ACL, type of bundle, type of graft, and time from injury to surgery, we found no evidence that increased synovialization improves clinical outcomes at 1 year postoperatively.
Keyword
MeSH Terms
Figure
Reference
-
1. Yasuda K, Tanabe Y, Kondo E, Kitamura N, Tohyama H. Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2010; 26:9 Suppl. S21–S34.
Article2. Ochi M, Abouheif MM, Kongcharoensombat W, Nakamae A, Adachi N, Deie M. Double bundle arthroscopic anterior cruciate ligament reconstruction with remnant preserving technique using a hamstring autograft. Sports Med Arthrosc Rehabil Ther Technol. 2011; 3:30.
Article3. Kondo E, Yasuda K, Onodera J, Kawaguchi Y, Kitamura N. Effects of remnant tissue preservation on clinical and arthroscopic results after anatomic double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2015; 43(8):1882–1892.
Article4. Ahn JH, Choi SH, Wang JH, Yoo JC, Yim HS, Chang MJ. Outcomes and second-look arthroscopic evaluation after double-bundle anterior cruciate ligament reconstruction with use of a single tibial tunnel. J Bone Joint Surg Am. 2011; 93(20):1865–1872.
Article5. Noh JH, Kyung HS, Roh YH, Kang TS. Remnant-preserving and re-tensioning technique to cover the graft in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017; 25(4):1205–1210.
Article6. Takahashi T, Kondo E, Yasuda K, et al. Effects of remnant tissue preservation on the tendon graft in anterior cruciate ligament reconstruction: a biomechanical and histological study. Am J Sports Med. 2016; 44(7):1708–1716.
Article7. Tajima T, Chosa E, Yamaguchi N, Taniguchi N, Ishida Y. Remnant-preserving, selective single-bundle augmentation of the anterior cruciate ligament using a bone-patellar tendon-bone autograft: a technical note. Knee. 2016; 23(3):554–558.
Article8. Lee BI, Kwon SW, Choi HS, Chun DI, Kim YB, Kim BM. Anatomic single-bundle anterior cruciate ligament reconstruction with remnant preservation using outside-in technique. Arthrosc Tech. 2015; 4(4):e331–e334.
Article9. Schultz RA, Miller DC, Kerr CS, Micheli L. Mechanoreceptors in human cruciate ligaments: a histological study. J Bone Joint Surg Am. 1984; 66(7):1072–1076.
Article10. Ochi M, Iwasa J, Uchio Y, Adachi N, Sumen Y. The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 1999; 81(5):902–906.
Article11. Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I. The long-term followup of primary anterior cruciate ligament repair: defining a rationale for augmentation. Am J Sports Med. 1991; 19(3):243–255.
Article12. Schutte MJ, Dabezies EJ, Zimny ML, Happel LT. Neural anatomy of the human anterior cruciate ligament. J Bone Joint Surg Am. 1987; 69(2):243–247.
Article13. Lee BI, Kwon SW, Kim JB, Choi HS, Min KD. Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy. 2008; 24(5):560–568.
Article14. Ochi M, Adachi N, Deie M, Kanaya A. Anterior cruciate ligament augmentation procedure with a 1-incision technique: anteromedial bundle or posterolateral bundle reconstruction. Arthroscopy. 2006; 22(4):463.e1–463.e5.
Article15. Crain EH, Fithian DC, Paxton EW, Luetzow WF. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005; 21(1):19–24.
Article16. Fremerey RW, Lobenhoffer P, Zeichen J, Skutek M, Bosch U, Tscherne H. Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study. J Bone Joint Surg Br. 2000; 82(6):801–806.17. Ahn GY, Nam IH, Moon GH, Lee YH, Choi SP, Yoo JY. The effect of a tibial remnant preservation technique on the synovialization of the graft tendon in anterior cruciate ligament reconstruction: based on the second look arthroscopic findings. J Korean Arthrosc Soc. 2013; 17(1):11–17.18. Rice RS, Waterman BR, Lubowitz JH. Allograft versus autograft decision for anterior cruciate ligament reconstruction: an expected-value decision analysis evaluating hypothetical patients. Arthroscopy. 2012; 28(4):539–547.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of a Tibial Remnant Preservation Technique on the Synovialization of the Graft Tendon in Anterior Cruciate Ligament Reconstruction: Based on the Second Look Arthroscopic Findings
- What Has Been Learned in Anterior Cruciate Ligament Reconstruction during the Past 20 Years?
- Current Trends in Anterior Cruciate Ligament Reconstruction
- Relationship between the Synovialization and the Clinical Results after Anterior Cruciate Ligament Reconstruction Using Tibialis Tendon Allograft
- Double-Bundle Anterior Cruciate Ligament Reconstruction