Obstet Gynecol Sci.
2018 Sep;61(5):626-630. 10.5468/ogs.2018.61.5.626.
Salvage para-aortic lymphadenectomy in recurrent cervical cancer after visualization with 3-dimensional computed tomography angiography
- Affiliations
-
- 1Department of Gynecology, National Cancer Center Hospital, Tokyo, Japan.
- 2Department of Radiation Oncology, Catholic University of Daegu, School of Medicine, Daegu, Korea.
- 3Department of Obstetrics and Gynecology, Kyungpook National University Medical Center, Daegu, Korea. chssa02202002@yahoo.co.kr
- KMID: 2426029
- DOI: http://doi.org/10.5468/ogs.2018.61.5.626
Abstract
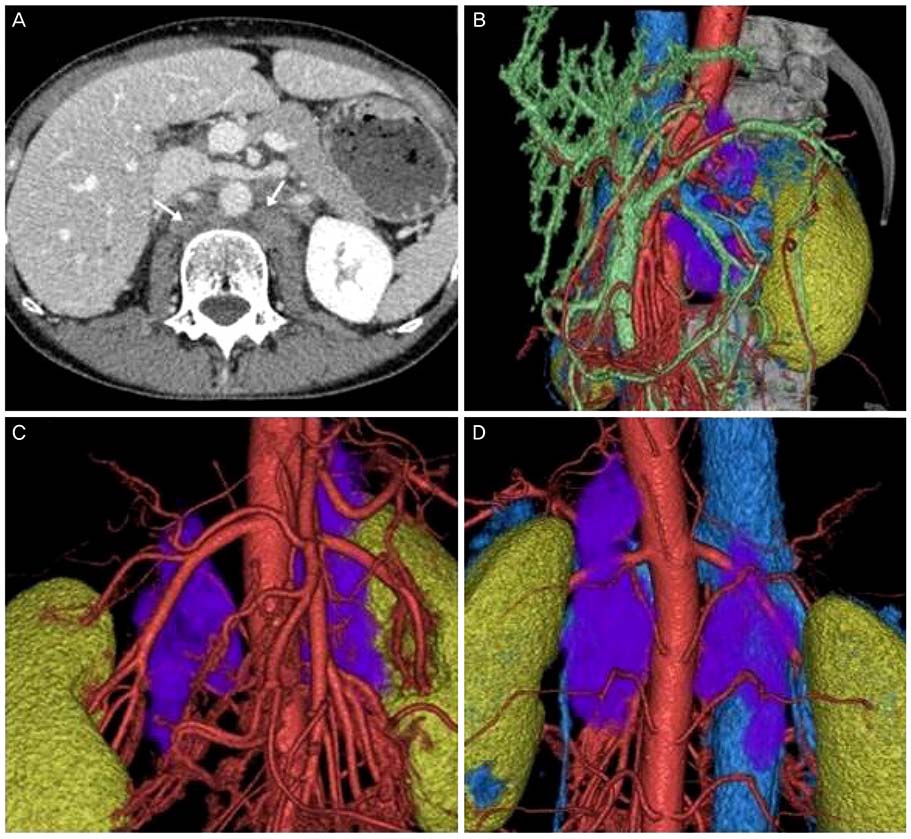
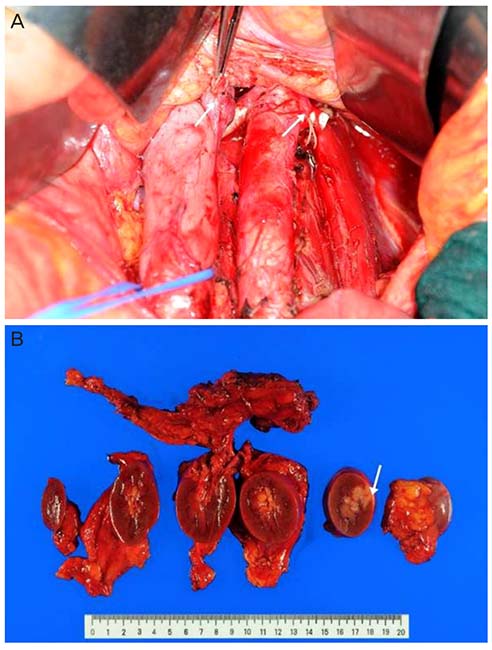
- We report a case of salvage lymphadenectomy for an isolated metastatic lesion in the para-aortic lymph node (LN) in a 49-year old woman with a history of cervical cancer, initially treated with radical hysterectomy and adjuvant radiotherapy. Preoperative 3-dimensional (3D) computed tomography (CT) angiography clearly revealed a huge retro-crural metastatic LN with distinct demarcation. A metastatic lesion, more than 10 cm in size, was located behind the vena cava, aorta, and left kidney, encompassing the left renal and lumbar arteries. The metastatic LN was excised along with the left kidney. On histologic examination, the tumor was found to have invaded the pelvis of the left kidney. Compared with conventional imaging techniques, 3D CT angiography can more clearly visualize such lesions. Thus, 3D CT angiography provides useful anatomical information, such as the exact size and location, and provides clear visualization and demarcation.
MeSH Terms
Figure
Reference
-
1. van Meir H, Kenter GG, Burggraaf J, Kroep JR, Welters MJ, Melief CJ, et al. The need for improvement of the treatment of advanced and metastatic cervical cancer, the rationale for combined chemo-immunotherapy. Anticancer Agents Med Chem. 2014; 14:190–203.2. Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013; 49:1374–1403.
Article3. Singh AK, Grigsby PW, Rader JS, Mutch DG, Powell MA. Cervix carcinoma, concurrent chemoradiotherapy, and salvage of isolated paraaortic lymph node recurrence. Int J Radiat Oncol Biol Phys. 2005; 61:450–455.
Article4. Koh WJ, Greer BE, Abu-Rustum NR, Apte SM, Campos SM, Cho KR, et al. Cervical cancer, version 2.2015. J Natl Compr Canc Netw. 2015; 13:395–404.
Article5. Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1991; 21:109–122.
Article6. Huang YT, Wang CC, Tsai CS, Lai CH, Chang TC, Chou HH, et al. Long-term outcome and prognostic factors for adenocarcinoma/adenosquamous carcinoma of cervix after definitive radiotherapy. Int J Radiat Oncol Biol Phys. 2011; 80:429–436.
Article7. Gouy S, Morice P, Narducci F, Uzan C, Gilmore J, Kolesnikov-Gauthier H, et al. Nodal-staging surgery for locally advanced cervical cancer in the era of PET. Lancet Oncol. 2012; 13:e212–20.
Article8. Hong JH, Choi JS, Lee JH, Bae JW, Eom JM, Kim JT, et al. Laparoscopic lymphadenectomy for isolated lymph node recurrence in gynecologic malignancies. J Minim Invasive Gynecol. 2012; 19:188–195.
Article9. Ramirez PT. Laparoscopic surgery for isolated nodal recurrence: appropriate for all patients or only a select few? J Minim Invasive Gynecol. 2012; 19:146–147.
Article10. Kramer M, Schwab SA, Nkenke E, Eller A, Kammerer F, May M, et al. Whole body magnetic resonance angiography and computed tomography angiography in the vascular mapping of head and neck: an intraindividual comparison. Head Face Med. 2014; 10:16.
Article11. Fujioka H, Kato T, Sone M, Horita T, Sugawara S, Tsukagoshi S. Study of preoperative 3D-CT angiography of uterine artery in patients with uterine cervical cancer. Nippon Hoshasen Gijutsu Gakkai Zasshi. 2017; 73:112–119.
Article12. Li Y, Zheng Y, Lin J, Cai A, Zhou X, Wei X, et al. Evaluation of the relationship between extremity soft tissue sarcomas and adjacent major vessels using contrast-enhanced multidetector CT and three-dimensional volume-rendered CT angiography: a preliminary study. Acta Radiol. 2013; 54:966–972.
Article13. Panici PB, Calcagno M, Plotti F, Arrivi C, Di Donato V, Montera R, et al. Aortic lymphadenectomy in cervical cancer: anatomy, classification and technique. Gynecol Oncol. 2007; 107:S30–S32.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic pelvic and para-aortic lymphadenectomy
- Laparoscopy-assisted gastrectomy with para-aortic lymphadenectomy after palliative chemotherapy for advanced gastric cancer with isolated para-aortic lymph node metastasis
- A new technique of laparoscopic para-aortic lymphadenectomy optimizes perioperative outcome
- The Role of the Para-aortic Lymphadenectomy in Epithelial Ovarian Cancer
- Single-port laparoscopic transperitoneal infrarenal para-aortic lymphadenectomy as part of staging operation for early ovarian cancer and high grade endometrial cancer