Cancer Res Treat.
2018 Oct;50(4):1316-1323. 10.4143/crt.2017.575.
Breast Conservation Therapy Versus Mastectomy in Patients with T1-2N1 Triple-Negative Breast Cancer: Pooled Analysis of KROG 14-18 and 14-23
- Affiliations
-
- 1Department of Radiation Oncology, Ewha Womans University College of Medicine, Seoul, Korea.
- 2Department of Radiation Oncology, Hanyang University College of Medicine, Seoul, Korea.
- 3Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. radiat@snu.ac.kr
- 4Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wonro.park@samsung.com
- 5Department of Radiation Oncology, Asan Medical Center, Ulsan University College of Medicine, Seoul, Korea.
- 6Proton Therapy Center, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- 7Department of Radiation Oncology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 2424803
- DOI: http://doi.org/10.4143/crt.2017.575
Abstract
- PURPOSE
The aim of this study is to compare the treatment outcomes of breast conserving surgery (BCS) plus radiotherapy (RT) versus mastectomy for patients with pT1-2N1 triple-negative breast cancer (TNBC).
MATERIALS AND METHODS
Using two multicenter retrospective studies on breast cancer, a pooled analysis was performed among 320 patients with pT1-2N1 TNBC. All patients who underwent BCS (n=212) receivedwhole breast RTwith orwithoutregional nodal RT,while nonewho underwent mastectomy (n=108)received it. All patients received taxane-based adjuvant chemotherapy. The median follow-up periods were 65 months in the BCS+RT group, and 74 months in the mastectomy group.
RESULTS
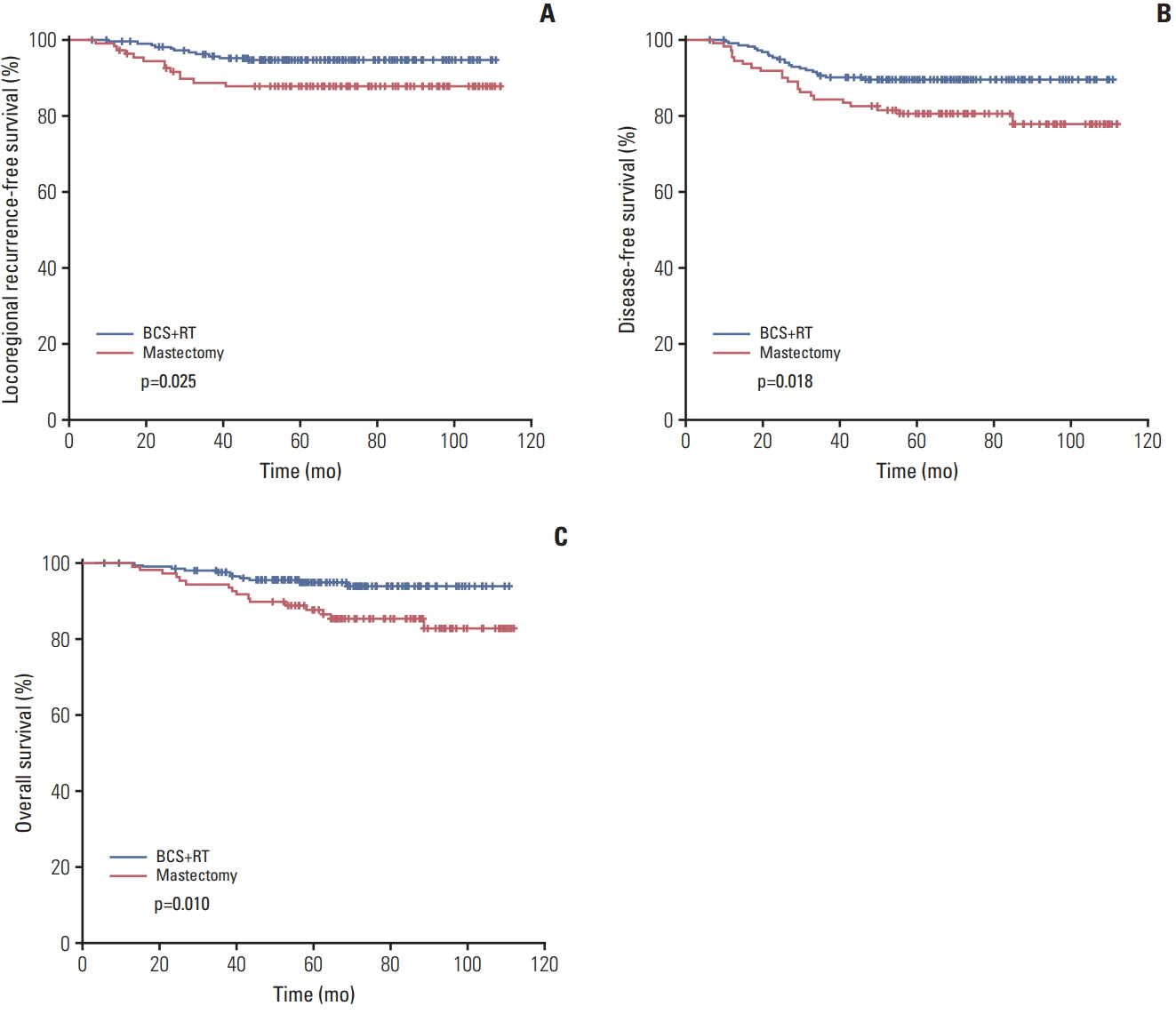
The median age of all patients was 48 years (range, 24 to 70 years). Mastectomy group had more patients with multiple tumors (p < 0.001), no lymphovascular invasion (p=0.001), higher number of involved lymph node (p=0.028), and higher nodal ratio ≥ 0.2 (p=0.037). Other characteristics were not significantly different between the two groups. The 5-year locoregionalrecurrence-free, disease-free, and overall survivalrates of BCS+RT group versus mastectomy group were 94.6% versus 87.7%, 89.5% versus 80.4%, and 95.0% versus 87.8%, respectively, and the differences were statistically significant after adjusting for covariates (p=0.010, p=0.006, and p=0.005, respectively).
CONCLUSION
In pT1-2N1 TNBC, breast conservation therapy achieved better locoregional recurrencefree, disease-free, and overall survival rates compared with mastectomy.
MeSH Terms
Figure
Reference
-
References
1. Lowery AJ, Kell MR, Glynn RW, Kerin MJ, Sweeney KJ. Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat. 2012; 133:831–41.
Article2. Ihemelandu CU, Naab TJ, Mezghebe HM, Makambi KH, Siram SM, Leffall LD Jr, et al. Treatment and survival outcome for molecular breast cancer subtypes in black women. Ann Surg. 2008; 247:463–9.
Article3. Parker CC, Ampil F, Burton G, Li BD, Chu QD. Is breast conservation therapy a viable option for patients with triplereceptor negative breast cancer? Surgery. 2010; 148:386–91.
Article4. Adkins FC, Gonzalez-Angulo AM, Lei X, Hernandez-Aya LF, Mittendorf EA, Litton JK, et al. Triple-negative breast cancer is not a contraindication for breast conservation. Ann Surg Oncol. 2011; 18:3164–73.
Article5. Ahn KJ, Park J, Choi Y. Lymphovascular invasion as a negative prognostic factor for triple-negative breast cancer after surgery. Radiat Oncol J. 2017; 35:332–9.
Article6. Wang J, Xie X, Wang X, Tang J, Pan Q, Zhang Y, et al. Locoregional and distant recurrences after breast conserving therapy in patients with triple-negative breast cancer: a meta-analysis. Surg Oncol. 2013; 22:247–55.
Article7. Hwang ES, Lichtensztajn DY, Gomez SL, Fowble B, Clarke CA. Survival after lumpectomy and mastectomy for early stage invasive breast cancer: the effect of age and hormone receptor status. Cancer. 2013; 119:1402–11.8. Agarwal S, Pappas L, Neumayer L, Kokeny K, Agarwal J. Effect of breast conservation therapy vs mastectomy on disease-specific survival for early-stage breast cancer. JAMA Surg. 2014; 149:267–74.
Article9. Hartmann-Johnsen OJ, Karesen R, Schlichting E, Nygard JF. Survival is better after breast conserving therapy than mastectomy for early stage breast cancer: a registry-based follow-up study of Norwegian women primary operated between 1998 and 2008. Ann Surg Oncol. 2015; 22:3836–45.
Article10. van Maaren MC, de Munck L, de Bock GH, Jobsen JJ, van Dalen T, Linn SC, et al. 10 year survival after breast-conserving surgery plus radiotherapy compared with mastectomy in early breast cancer in the Netherlands: a population-based study. Lancet Oncol. 2016; 17:1158–70.
Article11. Kang JK, Kim MS, Jang WI, Seo YS, Kim HJ, Cho CK, et al. The clinical utilization of radiation therapy in Korea between 2009 and 2013. Radiat Oncol J. 2016; 34:88–95.
Article12. Lee JA, Kim KI, Bae JW, Jung YH, An H, Lee ES, et al. Triple negative breast cancer in Korea-distinct biology with different impact of prognostic factors on survival. Breast Cancer Res Treat. 2010; 123:177–87.
Article13. Kim H, Park W, Yu JI, Choi DH, Huh SJ, Kim YJ, et al. Prognostic impact of elective supraclavicular nodal irradiation for patients with N1 breast cancer after lumpectomy and anthracycline plus taxane-based chemotherapy (KROG 1418): a multicenter case-controlled study. Cancer Res Treat. 2017; 49:970–80.14. Park HJ, Shin KH, Kim JH, Ahn SD, Kim JY, Park W, et al. Incorporating risk factors to identify the indication of postmastectomy radiotherapy in N1 breast cancer treated with optimal systemic therapy: a multicenter analysis in Korea (KROG 14-23). Cancer Res Treat. 2017; 49:739–47.
Article15. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002; 347:1233–41.
Article16. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002; 347:1227–32.
Article17. Abdulkarim BS, Cuartero J, Hanson J, Deschenes J, Lesniak D, Sabri S. Increased risk of locoregional recurrence for women with T1-2N0 triple-negative breast cancer treated with modified radical mastectomy without adjuvant radiation therapy compared with breast-conserving therapy. J Clin Oncol. 2011; 29:2852–8.
Article18. Zumsteg ZS, Morrow M, Arnold B, Zheng J, Zhang Z, Robson M, et al. Breast-conserving therapy achieves locoregional outcomes comparable to mastectomy in women with T1-2N0 triple-negative breast cancer. Ann Surg Oncol. 2013; 20:3469–76.
Article19. Kindts I, Buelens P, Laenen A, Van Limbergen E, Janssen H, Wildiers H, et al. Omitting radiation therapy in women with triple-negative breast cancer leads to worse breast cancer-specific survival. Breast. 2017; 32:18–25.
Article20. Bhoo-Pathy N, Verkooijen HM, Wong FY, Pignol JP, Kwong A, Tan EY, et al. Prognostic role of adjuvant radiotherapy in triple-negative breast cancer: a historical cohort study. Int J Cancer. 2015; 137:2504–12.
Article21. Mamounas EP, Tang G, Liu Q. The importance of systemic therapy in minimizing local recurrence after breast-conserving surgery: the NSABP experience. J Surg Oncol. 2014; 110:45–50.
Article22. Poortmans P. Postmastectomy radiation in breast cancer with one to three involved lymph nodes: ending the debate. Lancet. 2014; 383:2104–6.
Article23. Recht A, Comen EA, Fine RE, Fleming GF, Hardenbergh PH, Ho AY, et al. Postmastectomy radiotherapy: an American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology focused guideline update. J Clin Oncol. 2016; 34:4431–42.
Article24. Truong PT, Olivotto IA, Kader HA, Panades M, Speers CH, Berthelet E. Selecting breast cancer patients with T1-T2 tumors and one to three positive axillary nodes at high postmastectomy locoregional recurrence risk for adjuvant radiotherapy. Int J Radiat Oncol Biol Phys. 2005; 61:1337–47.
Article25. Tendulkar RD, Rehman S, Shukla ME, Reddy CA, Moore H, Budd GT, et al. Impact of postmastectomy radiation on locoregional recurrence in breast cancer patients with 1-3 positive lymph nodes treated with modern systemic therapy. Int J Radiat Oncol Biol Phys. 2012; 83:e577.
Article26. McBride A, Allen P, Woodward W, Kim M, Kuerer HM, Drinka EK, et al. Locoregional recurrence risk for patients with T1,2 breast cancer with 1-3 positive lymph nodes treated with mastectomy and systemic treatment. Int J Radiat Oncol Biol Phys. 2014; 89:392–8.
Article27. Whelan TJ, Olivotto IA, Parulekar WR, Ackerman I, Chua BH, Nabid A, et al. Regional nodal irradiation in early-stage breast cancer. N Engl J Med. 2015; 373:307–16.
Article28. Poortmans PM, Collette S, Kirkove C, Van Limbergen E, Budach V, Struikmans H, et al. Internal mammary and medial supraclavicular irradiation in breast cancer. N Engl J Med. 2015; 373:317–27.
Article29. van Roozendaal LM, Schipper RJ, Smit LH, Brans BT, Beets-Tan RG, Lobbes MB, et al. Three-dimensional breast radiotherapy and the elective radiation dose at the sentinel lymph nodes site in breast cancer. Ann Surg Oncol. 2015; 22:3824–30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Which Patients Might Benefit from Postmastectomy Radiotherapy in Breast Cancer Patients with T1-2 Tumor and 1-3 Axillary Lymph Nodes Metastasis?
- Are the Outcomes of Breast Conservation Surgery Inferior to Those of Mastectomy in Patients with Stage II-IIIA Triple-Negative Breast Cancer?
- Comment on “Histomorphological Factors Predicting the Response to Neoadjuvant Chemotherapy in Triple-Negative Breast Cancerâ€
- Treatment Outcomes of Weakly Positive Hormone Receptor Breast Cancer and Triple-Negative Breast Cancer
- Evaluation of the Survival Benefit of Different Chemotherapy Regimens in Patients with T1-2N0 Triple-Negative Breast Cancer