J Korean Fract Soc.
2017 Jul;30(3):156-166. 10.12671/jkfs.2017.30.3.156.
Clinical and Radiological Analysis of Angular Deformity of Lower Extremities
- Affiliations
-
- 1Department of Orthopedic Surgery, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea. changhoonj@gmail.com
- KMID: 2424126
- DOI: http://doi.org/10.12671/jkfs.2017.30.3.156
Abstract
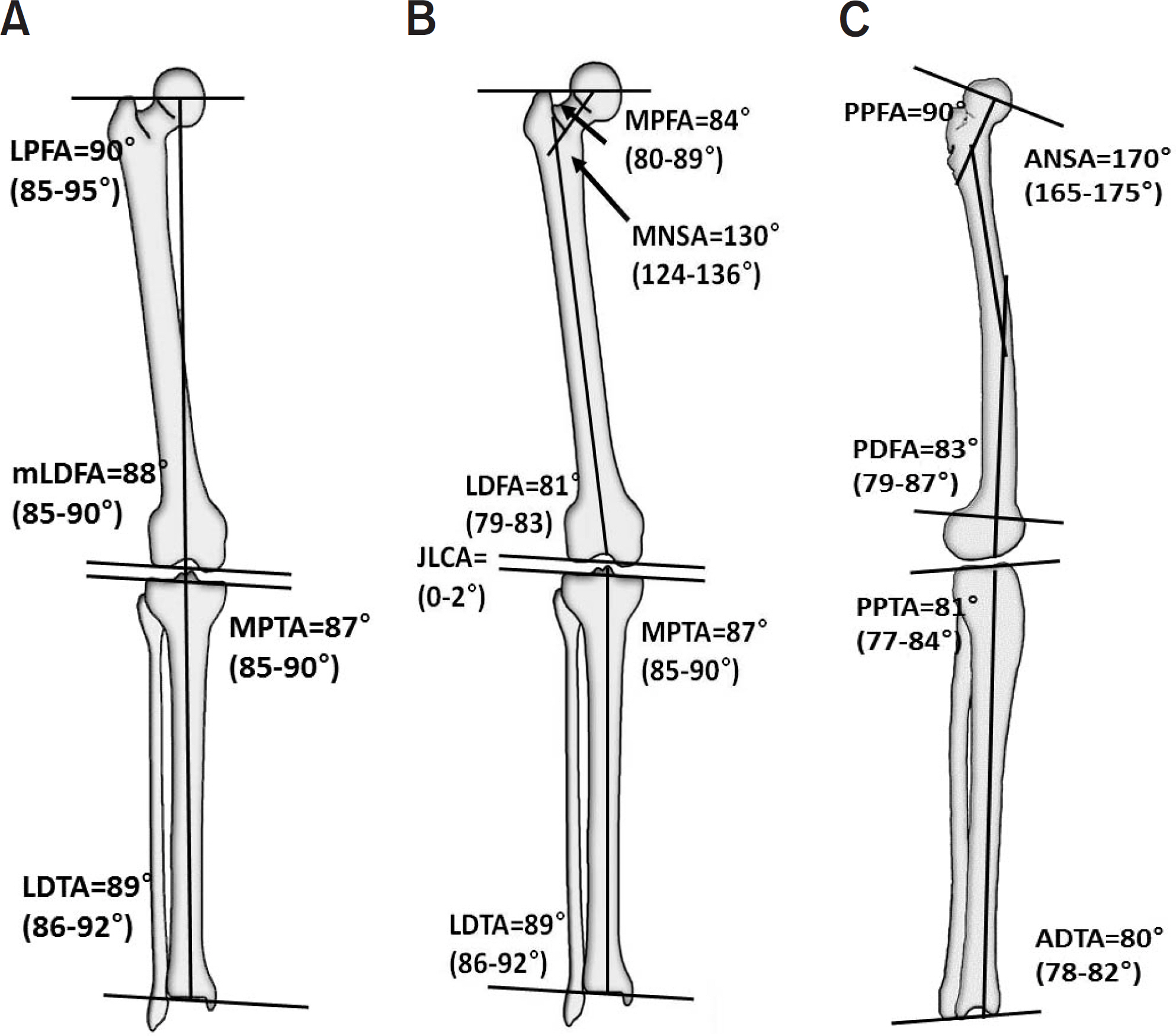
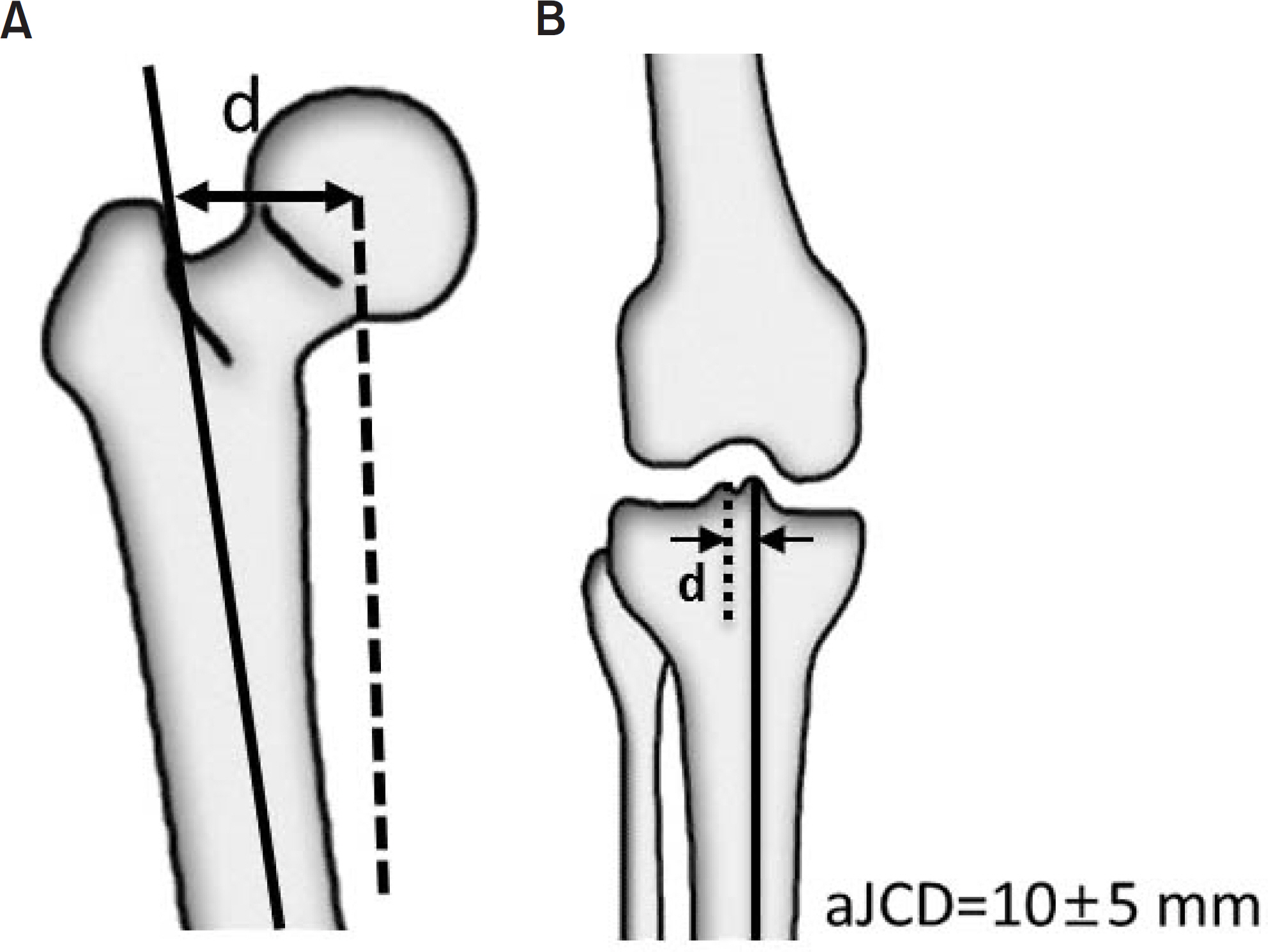
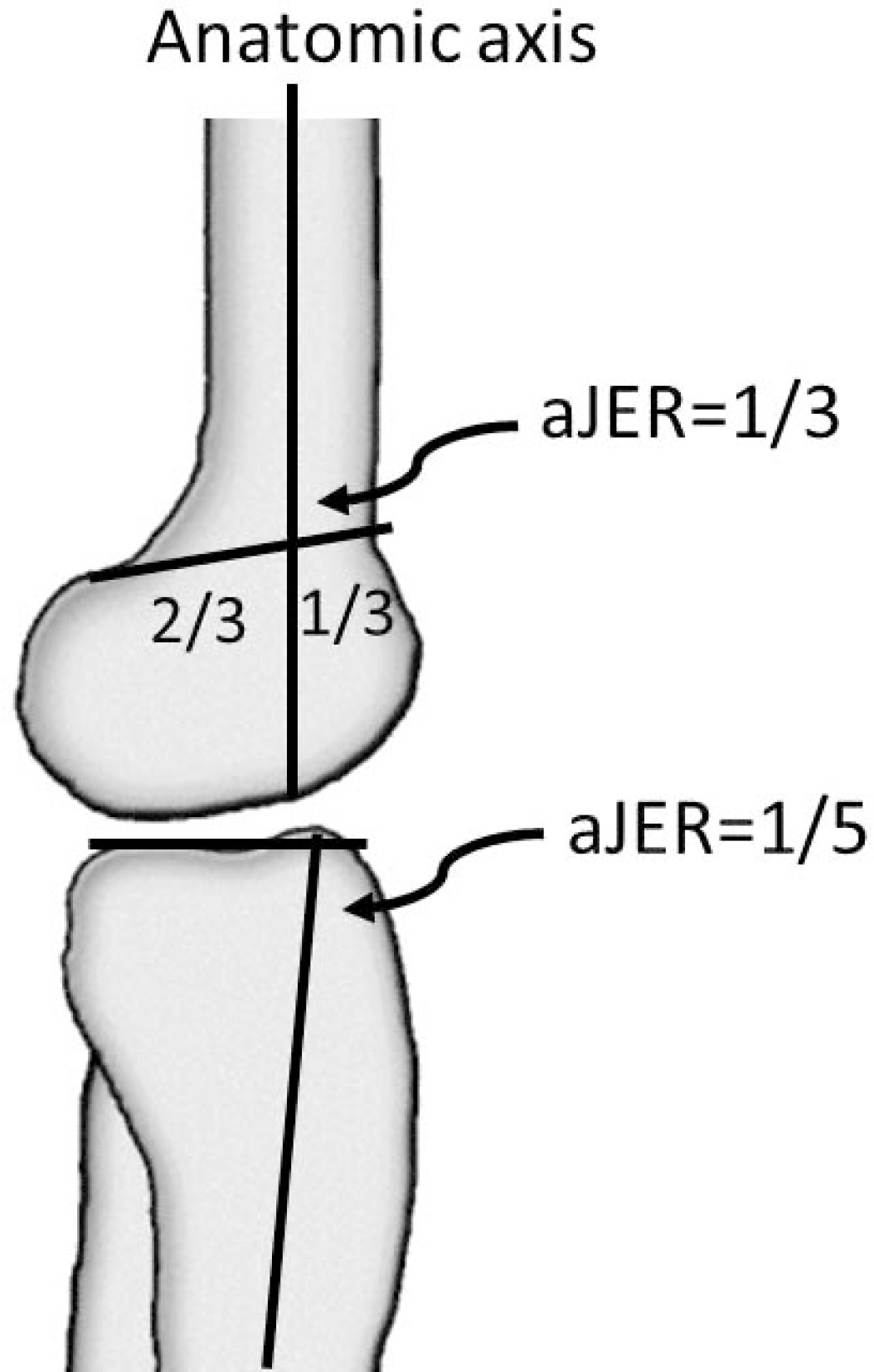
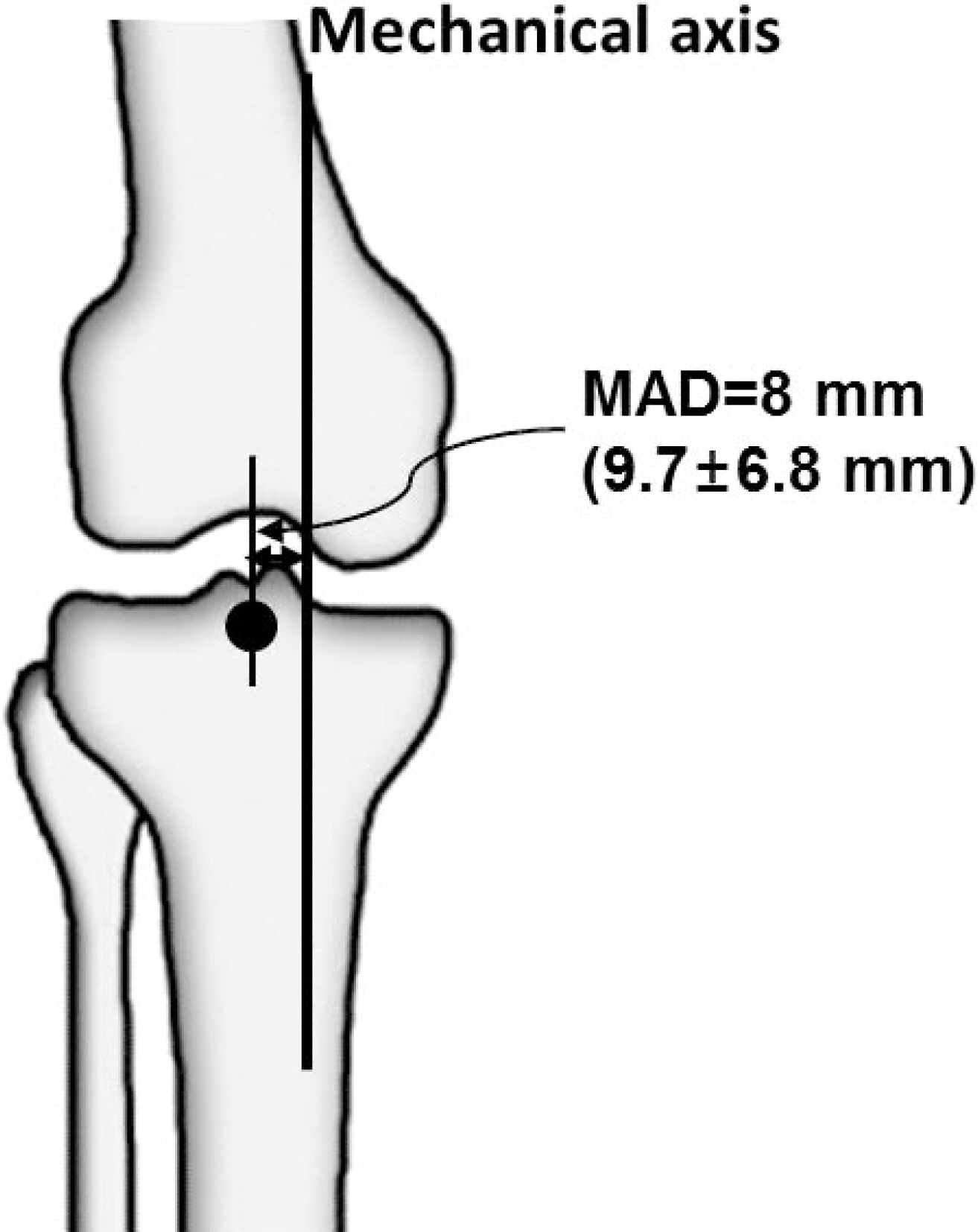
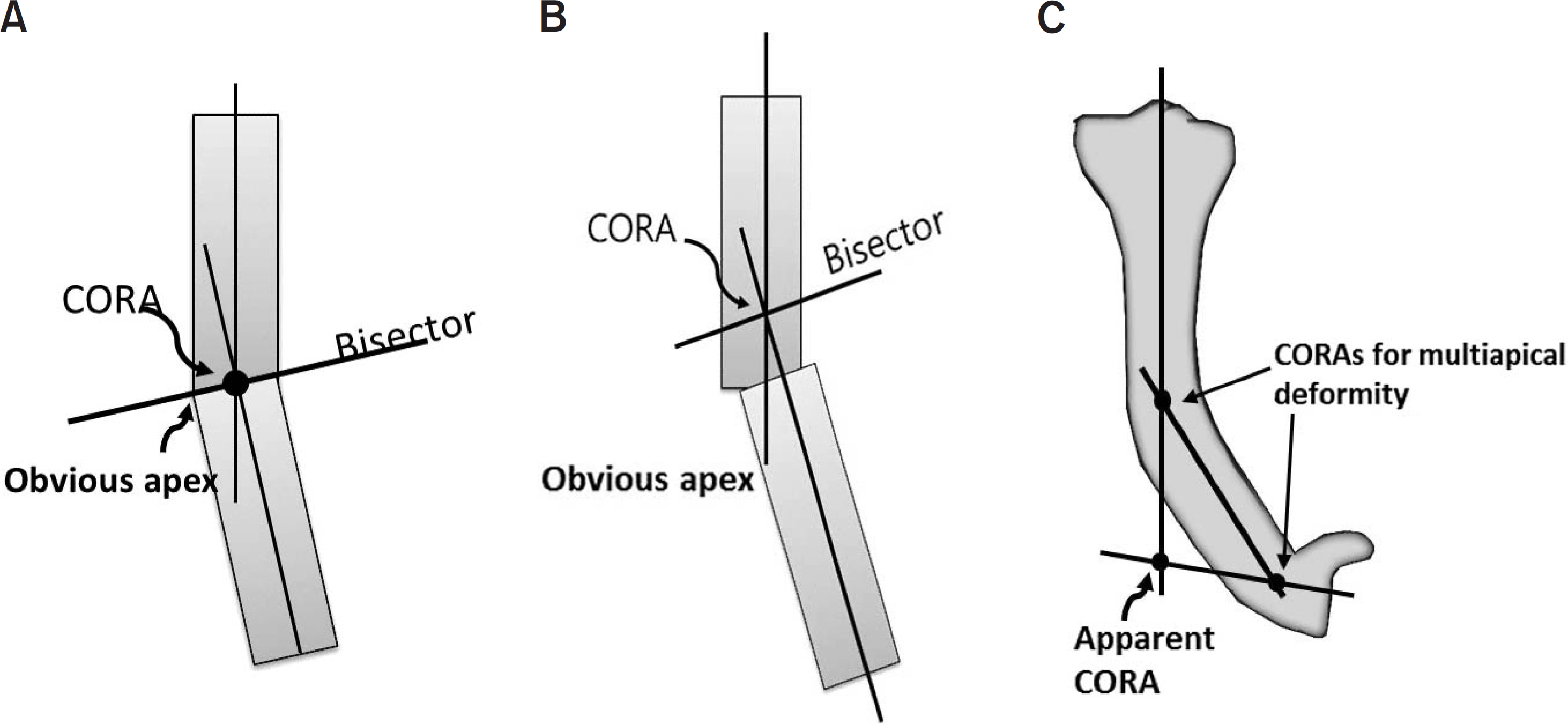
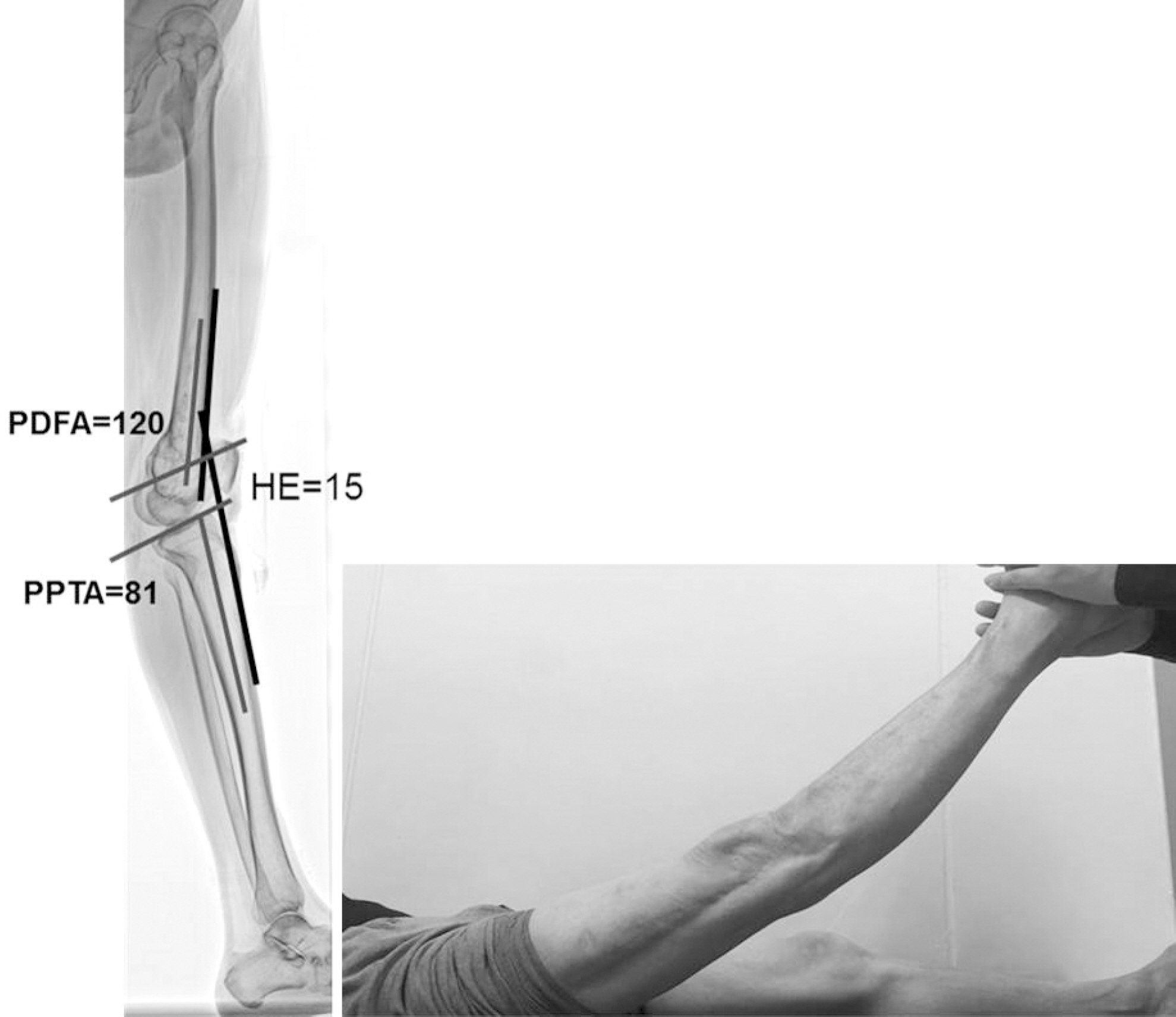
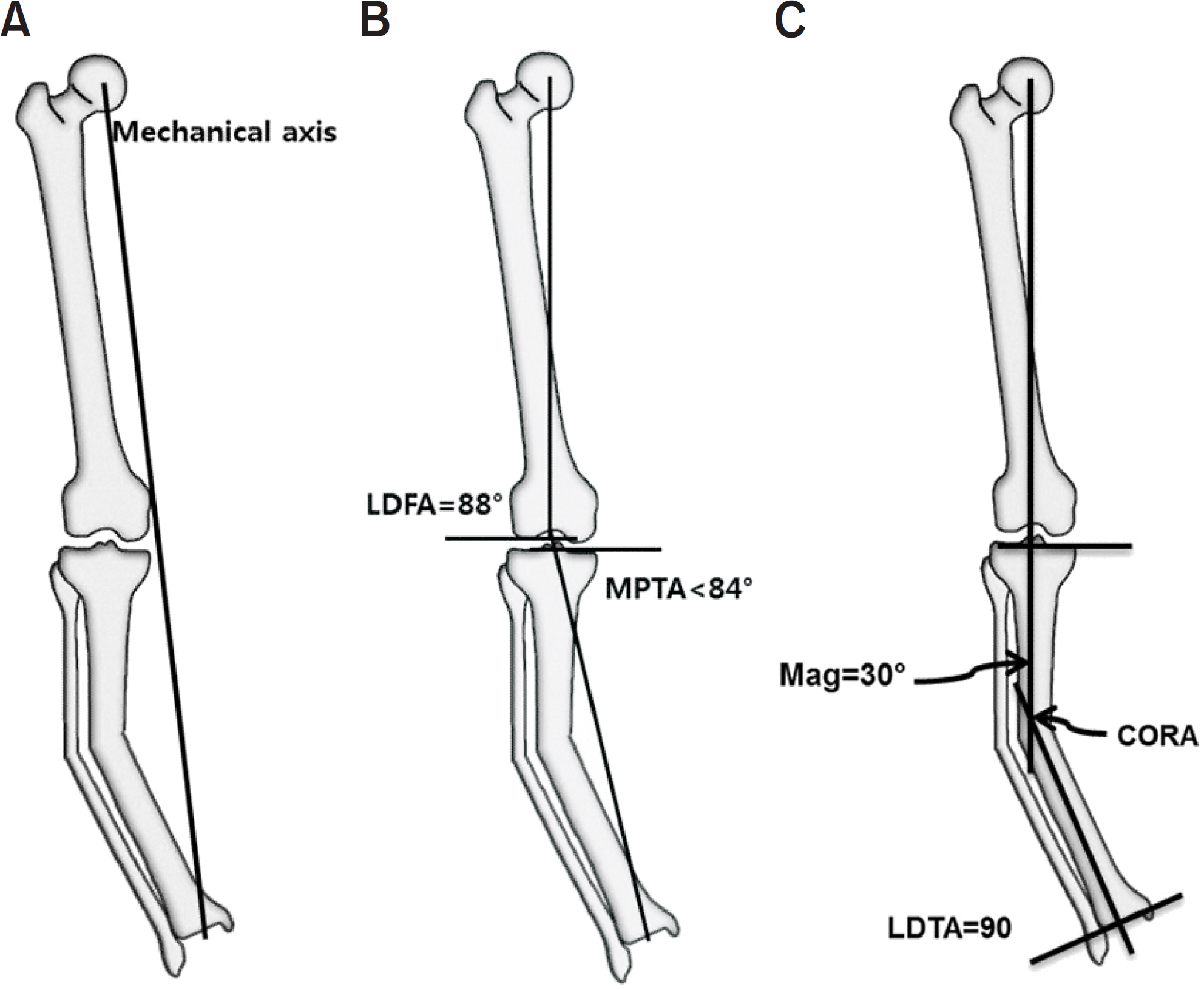
- The alignment of lower extremities is an important consideration in many clinical situations, including fracture reduction, high tibia osteotomy, total knee arthroplasty, and deformity correction. Mal-alignment of lower extremities is not only a simple cosmetic problem, but it can also produce pain, limp, and early degenerative arthritis. An assessment of lower extremity alignment, including its location and magnitude of deformity, can be achieved via mal-alignment test and mal-orientation test, using a lower extremity standing full-length radiography. Proper evaluation allows the surgeon to determine an effective treatment plan for deformity correction.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Beals RK, Stanley G. Surgical correction of bowlegs in achondroplasia. J Pediatr Orthop B. 14:245–249. 2005.
Article2. Cusick BD, Stuberg WA. Assessment of lower-extremity alignment in the transverse plane: implications for management of children with neuromotor dysfunction. Phys Ther. 72:3–15. 1992.
Article3. Song HR, Soma Raju VV, Kumar S, et al. Deformity correction by external fixation and/or intramedullary nailing in hypophosphatemic rickets. Acta Orthop. 77:307–314. 2006.
Article4. Tetsworth K, Paley D. Malalignment and degenerative arthropathy. Orthop Clin North Am. 25:367–377. 1994.
Article5. Felson DT, Niu J, Gross KD, et al. Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the multicenter osteoarthritis study and the osteoarthritis initiative. Arthritis Rheum. 65:355–362. 2013.
Article6. Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 69:745–749. 1987.
Article7. Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 25:425–465. 1994.
Article8. Chao EY, Neluheni EV, Hsu RW, Paley D. Biomechanics of malalignment. Orthop Clin North Am. 25:379–386. 1994.
Article9. Cooke TD, Li J, Scudamore RA. Radiographic assessment of bony contributions to knee deformity. Orthop Clin North Am. 25:387–393. 1994.
Article10. Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur. J Bone Joint Surg Am. 69:873–880. 1987.
Article11. Brinker MR, O'Connor DP. Principles of malunions. Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, III PT, editors. Rockwood and Green's fractures in adults. 8th ed.Philadelphia, Wolters Kluwer Health: 869–894;2015.12. Lesiak AC, Vosseller JT, Rozbruch SR. Osteotomy, arthrodesis, and arthroplasty for complex multiapical deformity of the leg. HSS J. 8:304–308. 2012.
Article13. Krettek C, Miclau T, Grün O, Schandelmaier P, Tscherne H. Intraoperative control of axes, rotation and length in femoral and tibial fractures. Technical note. Injury, 29 Suppl. 3:C29–C39. 1998.
Article14. Sheehy L, Cooke TD, McLean L, Culham E. Standardized standing pelvis-to-floor photographs for the assessment of lower-extremity alignment. Osteoarthr Cartil. 23:379–382. 2015.
Article15. Wu CC. Is clinical measurement of anatomic axis of the femur adequate? Acta Orthop. 1–4:2017.
Article16. Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res. 290:259–268. 1993.
Article17. Wright JG, Treble N, Feinstein AR. Measurement of lower limb alignment using long radiographs. J Bone Joint Surg Br. 73:721–723. 1991.
Article18. Paley D. Principles of deformity correction. 3rd ed.Berlin;Springer: 2005.19. Holme TJ, Henckel J, Hartshorn K, Cobb JP, Hart AJ. Computed tomography scanogram compared to long leg radiograph for determining axial knee alignment. Acta Orthop. 86:440–443. 2015.
Article20. Sabharwal S, Zhao C. Assessment of lower limb alignment: supine fluoroscopy compared with a standing full-length radiograph. J Bone Joint Surg Am. 90:43–51. 2008.
Article21. Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 280:48–64. 1992.22. Paley D. Principles of deformity correction. Berlin: Springer;p. 163. 2005.23. Paley D, Chaudray M, Pirone AM, Lentz P, Kautz D. Treatment of malunions and mal-nonunions of the femur and tibia by detailed preoperative planning and the Ilizarov techniques. Orthop Clin North Am. 21:667–691. 1990.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Angular Deformity Correction by Asymmetrical Physeal Supression in Children
- Remodelling of Angular DeforMity after Femoral Shaft Fractures in Children
- Deformity Correction by Femoral Supracondylar Dome Osteotomy with Retrograde Intramedullary Nailing in Varus Deformity of the Distal Femur after Pathologic Fracture of Giant Cell Tumor
- A case report of osteogenesis imperfecta
- The Angular Deformity of Interlocking Nailing in Tibial Fractures